Tuesday Poster Session
Category: Esophagus
P4991 - A Rare Case of a Giant Idiopathic Esophageal Ulcer in a Pregnant Woman With HIV/AIDS
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abay Gobezie, MD (he/him/his)
Howard University Hospital
Washington, DC
Presenting Author(s)
Abay Gobezie, MD1, Nakul Ganju, MD2, Sneha Rao Adidam, MD1, Melinda Beale, MD1, Farshad Aduli, MD1, Maryam Foroughi, MD1
1Howard University Hospital, Washington, DC; 2Department of Medicine, Howard University Hospital, Washington, DC
Introduction: Esophageal ulcers in immunocompromised patients, especially those with advanced HIV/AIDS, with a prevalence of < 10%, are commonly due to opportunistic infections such as CMV, HSV, or Candida. However, idiopathic HIV-associated giant esophageal ulcers correlate with profound immunosuppression (CD4 < 50 cells/mm³) and cause significant morbidity. Their occurrence during pregnancy, particularly in patients with congenital HIV, is infrequent and poorly documented, posing unique diagnostic and therapeutic challenges. Here, we present a rare case of HIV associated giant idiopathic esophageal ulcer in a pregnant woman, highlighting the diagnostic complexity and the importance of early endoscopic evaluation.
Case Description/
Methods: A 32-year-old pregnant woman (G3P1102 at 21 weeks gestation) presented with a three-week history of odynophagia and dysphagia. Her medical history was notable for congenital HIV/AIDS, non-adherence to ART, and profound immunosuppression (CD4 count of 4 cells/mm³, HIV viral load of 96,000 copies/mL). Esophagogastroduodenoscopy (EGD) revealed multiple deep, cratered esophageal ulcers without active bleeding or recent stigmata (Figure 1). Histopathologic evaluation showed squamous mucosa with diffuse ulceration, acute/chronic inflammation, and granulation tissue formation (Figure 2). Special stains and immunohistochemistry were negative for CMV, HSV, Adenovirus, Candida, and acid-fast bacilli (AFB). Given the clinical context and exclusion of opportunistic infections, a diagnosis of idiopathic HIV-associated esophageal ulcer was made. The patient was re-initiated on ART with close infectious disease and obstetric follow-up. Her symptoms gradually improved, and her pregnancy remained viable at follow-up.
Discussion: Unlike ulcers caused by opportunistic infections, HIV ulcers are believed to result from direct HIV-mediated immune dysfunction, cytokine dysregulation, and mucosal breakdown. The histology in HIV ulcers is typically non-specific, making clinical context and exclusion of other etiologies essential for diagnosis. Management centers on the re-initiation of ART, symptomatic care, and nutritional support. This case reinforces the importance of considering idiopathic HIV ulcers in the differential diagnosis of esophageal ulcerations in immunocompromised patients, especially when infectious workup is negative, and highlights the critical role of early endoscopy and tissue diagnosis in guiding management.
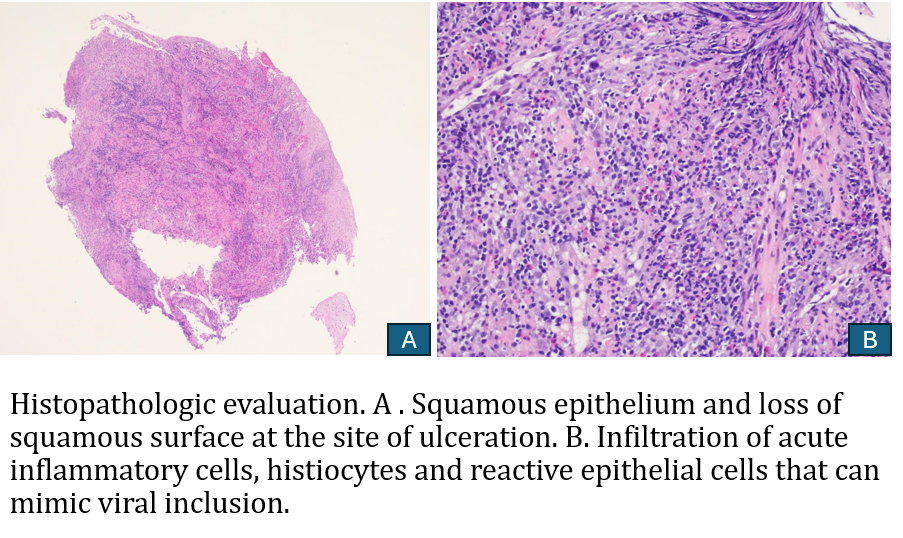
Figure: Giant HIV Esophageal ulcer
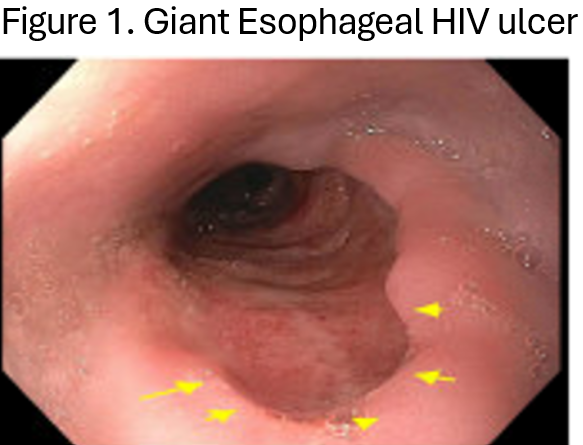
Figure: Histopathologic evaluation. A. Squamous epithelium and loss of squamous surface at the site of ulceration. B. Infiltration of acute inflammatory cells, histiocytes, and reactive epithelial cells that can mimic viral inclusion.
Disclosures:
Abay Gobezie indicated no relevant financial relationships.
Nakul Ganju indicated no relevant financial relationships.
Sneha Rao Adidam indicated no relevant financial relationships.
Melinda Beale indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Maryam Foroughi indicated no relevant financial relationships.
Abay Gobezie, MD1, Nakul Ganju, MD2, Sneha Rao Adidam, MD1, Melinda Beale, MD1, Farshad Aduli, MD1, Maryam Foroughi, MD1. P4991 - A Rare Case of a Giant Idiopathic Esophageal Ulcer in a Pregnant Woman With HIV/AIDS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Howard University Hospital, Washington, DC; 2Department of Medicine, Howard University Hospital, Washington, DC
Introduction: Esophageal ulcers in immunocompromised patients, especially those with advanced HIV/AIDS, with a prevalence of < 10%, are commonly due to opportunistic infections such as CMV, HSV, or Candida. However, idiopathic HIV-associated giant esophageal ulcers correlate with profound immunosuppression (CD4 < 50 cells/mm³) and cause significant morbidity. Their occurrence during pregnancy, particularly in patients with congenital HIV, is infrequent and poorly documented, posing unique diagnostic and therapeutic challenges. Here, we present a rare case of HIV associated giant idiopathic esophageal ulcer in a pregnant woman, highlighting the diagnostic complexity and the importance of early endoscopic evaluation.
Case Description/
Methods: A 32-year-old pregnant woman (G3P1102 at 21 weeks gestation) presented with a three-week history of odynophagia and dysphagia. Her medical history was notable for congenital HIV/AIDS, non-adherence to ART, and profound immunosuppression (CD4 count of 4 cells/mm³, HIV viral load of 96,000 copies/mL). Esophagogastroduodenoscopy (EGD) revealed multiple deep, cratered esophageal ulcers without active bleeding or recent stigmata (Figure 1). Histopathologic evaluation showed squamous mucosa with diffuse ulceration, acute/chronic inflammation, and granulation tissue formation (Figure 2). Special stains and immunohistochemistry were negative for CMV, HSV, Adenovirus, Candida, and acid-fast bacilli (AFB). Given the clinical context and exclusion of opportunistic infections, a diagnosis of idiopathic HIV-associated esophageal ulcer was made. The patient was re-initiated on ART with close infectious disease and obstetric follow-up. Her symptoms gradually improved, and her pregnancy remained viable at follow-up.
Discussion: Unlike ulcers caused by opportunistic infections, HIV ulcers are believed to result from direct HIV-mediated immune dysfunction, cytokine dysregulation, and mucosal breakdown. The histology in HIV ulcers is typically non-specific, making clinical context and exclusion of other etiologies essential for diagnosis. Management centers on the re-initiation of ART, symptomatic care, and nutritional support. This case reinforces the importance of considering idiopathic HIV ulcers in the differential diagnosis of esophageal ulcerations in immunocompromised patients, especially when infectious workup is negative, and highlights the critical role of early endoscopy and tissue diagnosis in guiding management.
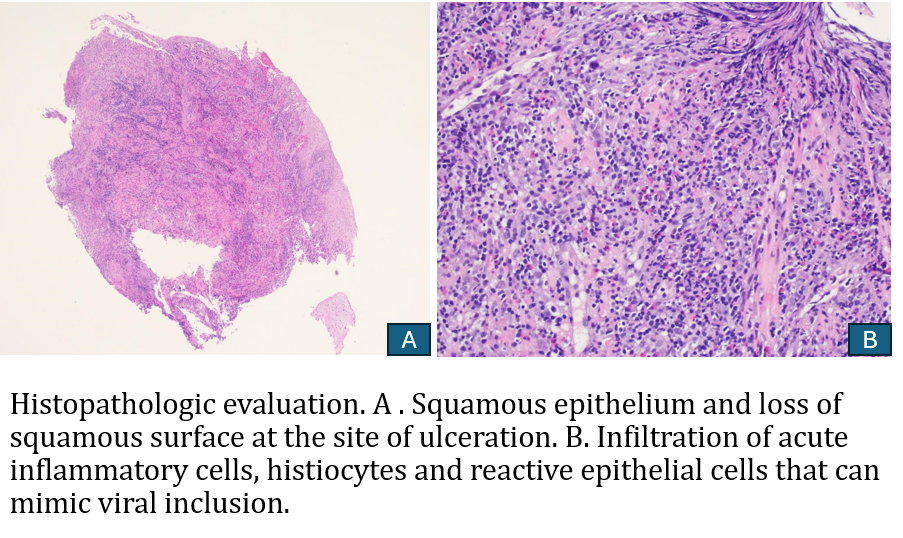
Figure: Giant HIV Esophageal ulcer
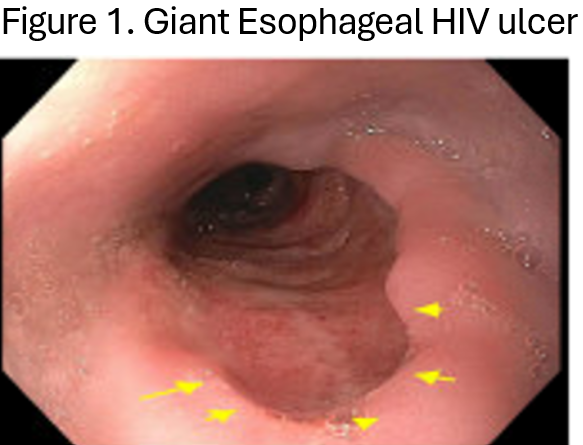
Figure: Histopathologic evaluation. A. Squamous epithelium and loss of squamous surface at the site of ulceration. B. Infiltration of acute inflammatory cells, histiocytes, and reactive epithelial cells that can mimic viral inclusion.
Disclosures:
Abay Gobezie indicated no relevant financial relationships.
Nakul Ganju indicated no relevant financial relationships.
Sneha Rao Adidam indicated no relevant financial relationships.
Melinda Beale indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Maryam Foroughi indicated no relevant financial relationships.
Abay Gobezie, MD1, Nakul Ganju, MD2, Sneha Rao Adidam, MD1, Melinda Beale, MD1, Farshad Aduli, MD1, Maryam Foroughi, MD1. P4991 - A Rare Case of a Giant Idiopathic Esophageal Ulcer in a Pregnant Woman With HIV/AIDS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
