Tuesday Poster Session
Category: Esophagus
P4986 - Superior Vena Cava Syndrome: A Rare but Severe Complication of Mega-Esophagus in Achalasia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aya Akhras, MD
HCA Florida Aventura Hospital
Aventura, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Aya Akhras, MD, Oscar Hernandez, MD, Ramasamy Nathan, MD
HCA Florida Aventura Hospital, Aventura, FL
Introduction: Megaesophagus is a common complication of achalasia. It arises from mechanical obstruction at the lower esophageal sphincter, resulting in progressive dilation of the esophageal body and subsequent accumulation of food material. While typical symptoms include dysphagia and regurgitation, severe complications such as extrinsic tracheal compression and superior vena cava (SVC) syndrome are rarely reported. We present a challenging case of achalasia complicated by acute airway obstruction and SVC syndrome.
Case Description/
Methods: A 33-year-old male with a known history of achalasia, remotely treated with pneumatic balloon dilation, presented to the emergency department with acute-onset shortness of breath after ingesting a large food bolus. CT imaging revealed a markedly dilated, food-filled esophagus causing significant tracheal compression without perforation (figure 1A&B). His respiratory distress progressed to stridor, necessitating emergent intubation. Post-intubation, he developed facial and neck swelling with plethora and dusky discoloration, concerning for acute SVC syndrome (figure 2A).
Bedside bronchoscopy demonstrated severe tracheal compression by the dilated esophagus, with minimal luminal patency. Post-intubation chest X-ray showed further dilation of the esophagus with increased intra-luminal air. Placement of an orogastric tube resulted in esophageal decompression and resolution of tracheal compression and SVC syndrome (figure 2B). Subsequent esophagogastroduodenoscopy (EGD) revealed a markedly dilated, atonic, tortuous esophagus with retained food and blood, semi-circumferential ulcerations, and a widely patent lower esophageal sphincter (LES), consistent with vigorous achalasia. Much of the food material was removed using a Roth net. A barium esophagram demonstrated a classic bird’s beak appearance with contrast passage into the stomach.
Ultimately, the patient's diet was slowly advanced to a regular diet. He was discharged on proton pump inhibitor therapy with plans for further outpatient management of advanced achalasia in his home country.
Discussion: This case highlights a rare but life-threatening complication of achalasia presenting as megaesophagus complicated by acute SVC syndrome, which can occur after endotracheal intubation. Prompt recognition and management, including esophageal decompression, are critical to prevent further deterioration and optimize outcomes.
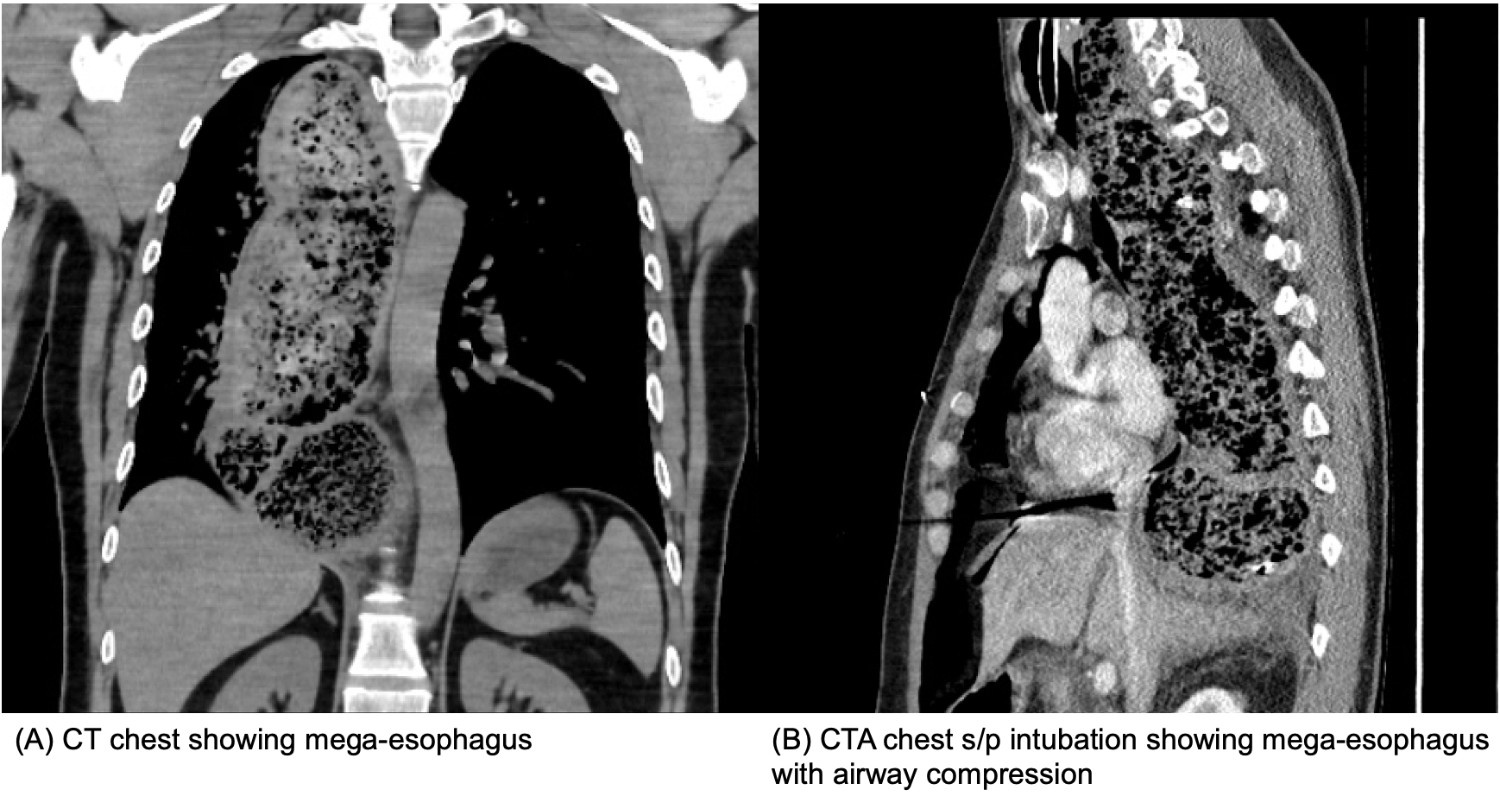
Figure: Figure 1. Mega-esophagus Resulting in Airway Compression
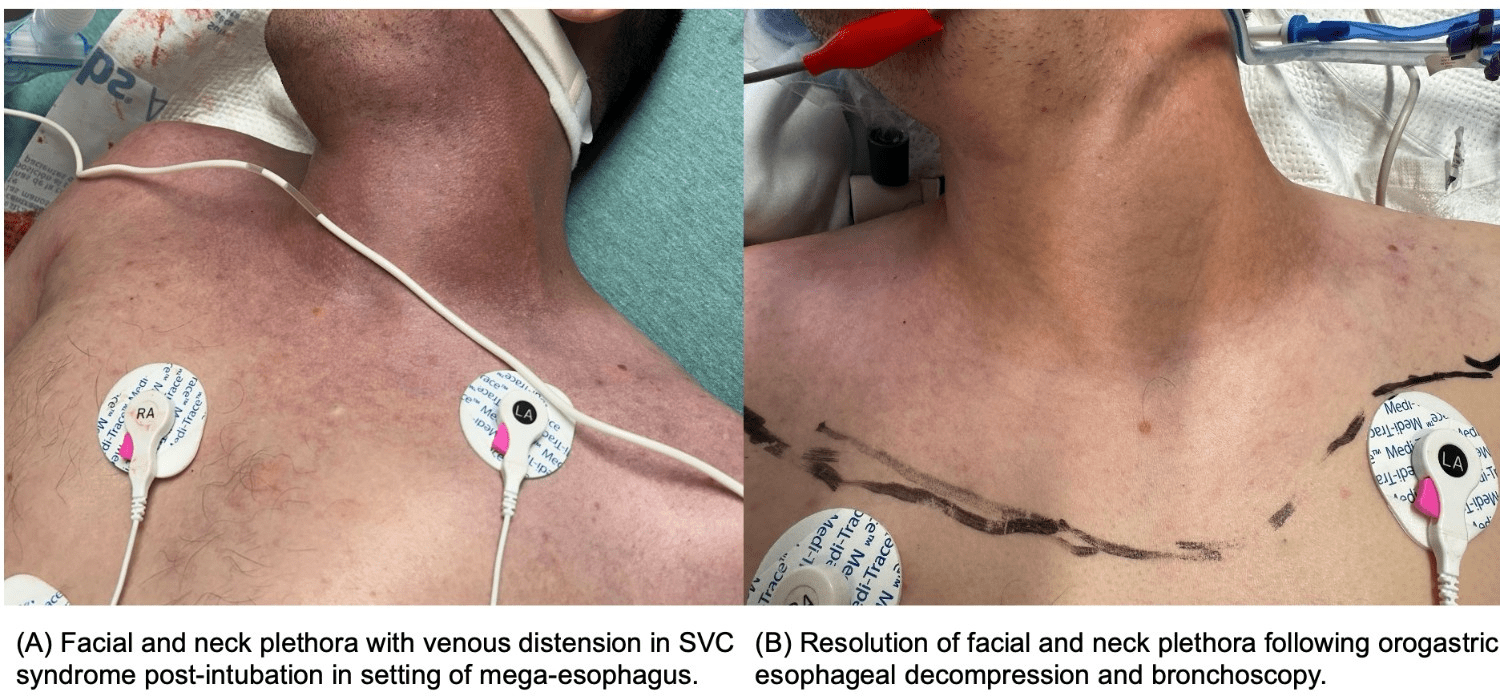
Figure: Figure 2. SVC Syndrome after endotracheal intubation in the setting of mega-esophagus
Disclosures:
Aya Akhras indicated no relevant financial relationships.
Oscar Hernandez indicated no relevant financial relationships.
Ramasamy Nathan indicated no relevant financial relationships.
Aya Akhras, MD, Oscar Hernandez, MD, Ramasamy Nathan, MD. P4986 - Superior Vena Cava Syndrome: A Rare but Severe Complication of Mega-Esophagus in Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Aya Akhras, MD, Oscar Hernandez, MD, Ramasamy Nathan, MD
HCA Florida Aventura Hospital, Aventura, FL
Introduction: Megaesophagus is a common complication of achalasia. It arises from mechanical obstruction at the lower esophageal sphincter, resulting in progressive dilation of the esophageal body and subsequent accumulation of food material. While typical symptoms include dysphagia and regurgitation, severe complications such as extrinsic tracheal compression and superior vena cava (SVC) syndrome are rarely reported. We present a challenging case of achalasia complicated by acute airway obstruction and SVC syndrome.
Case Description/
Methods: A 33-year-old male with a known history of achalasia, remotely treated with pneumatic balloon dilation, presented to the emergency department with acute-onset shortness of breath after ingesting a large food bolus. CT imaging revealed a markedly dilated, food-filled esophagus causing significant tracheal compression without perforation (figure 1A&B). His respiratory distress progressed to stridor, necessitating emergent intubation. Post-intubation, he developed facial and neck swelling with plethora and dusky discoloration, concerning for acute SVC syndrome (figure 2A).
Bedside bronchoscopy demonstrated severe tracheal compression by the dilated esophagus, with minimal luminal patency. Post-intubation chest X-ray showed further dilation of the esophagus with increased intra-luminal air. Placement of an orogastric tube resulted in esophageal decompression and resolution of tracheal compression and SVC syndrome (figure 2B). Subsequent esophagogastroduodenoscopy (EGD) revealed a markedly dilated, atonic, tortuous esophagus with retained food and blood, semi-circumferential ulcerations, and a widely patent lower esophageal sphincter (LES), consistent with vigorous achalasia. Much of the food material was removed using a Roth net. A barium esophagram demonstrated a classic bird’s beak appearance with contrast passage into the stomach.
Ultimately, the patient's diet was slowly advanced to a regular diet. He was discharged on proton pump inhibitor therapy with plans for further outpatient management of advanced achalasia in his home country.
Discussion: This case highlights a rare but life-threatening complication of achalasia presenting as megaesophagus complicated by acute SVC syndrome, which can occur after endotracheal intubation. Prompt recognition and management, including esophageal decompression, are critical to prevent further deterioration and optimize outcomes.
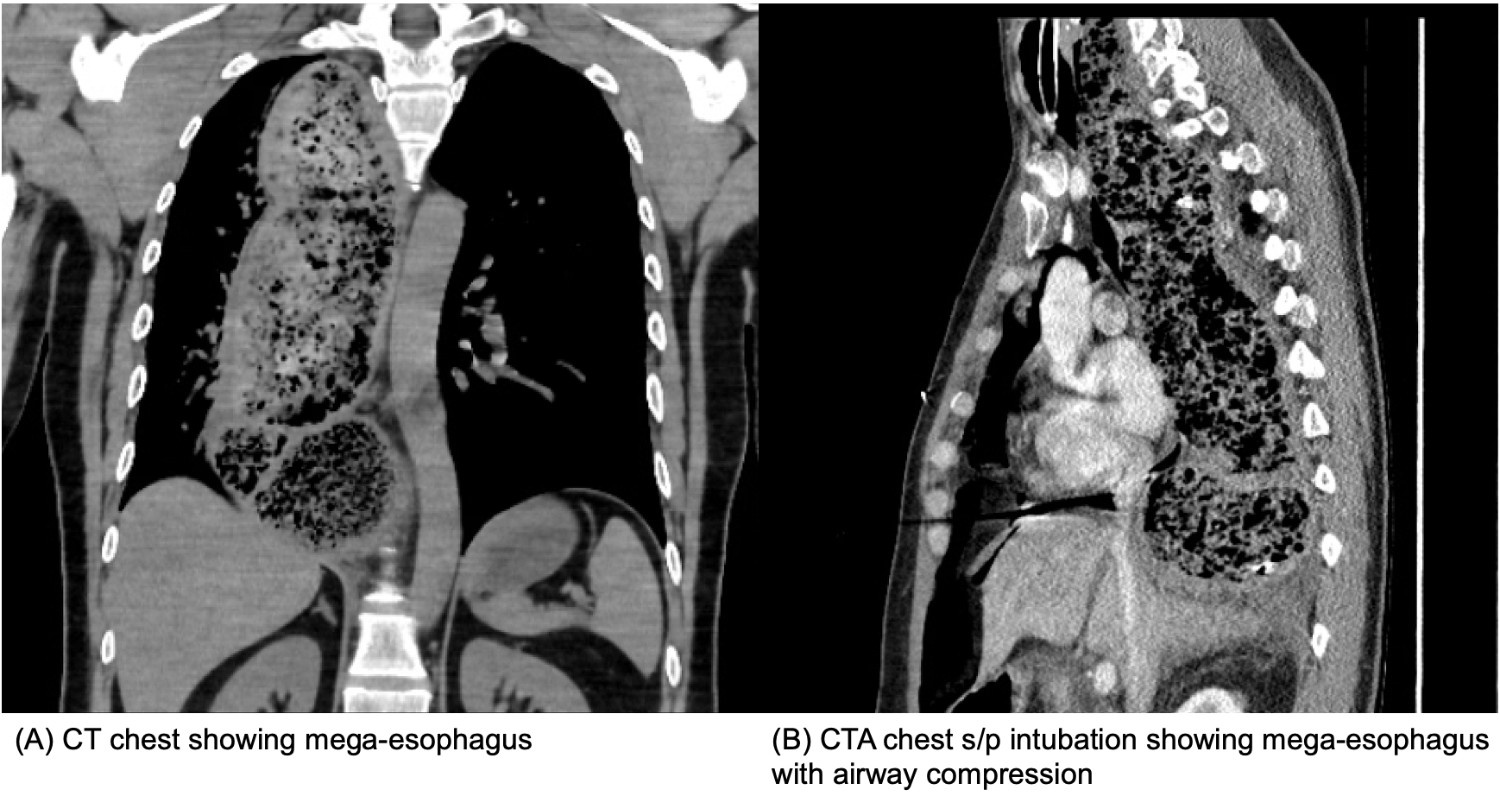
Figure: Figure 1. Mega-esophagus Resulting in Airway Compression
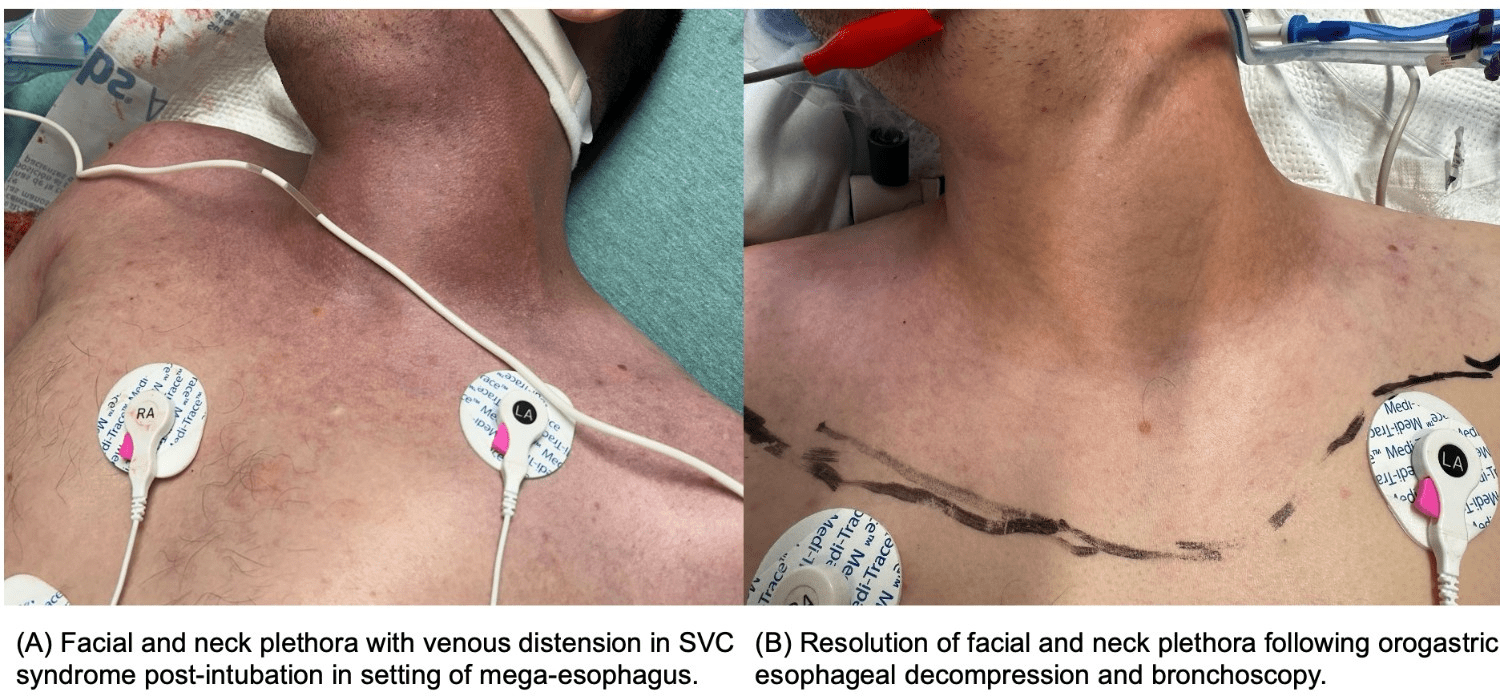
Figure: Figure 2. SVC Syndrome after endotracheal intubation in the setting of mega-esophagus
Disclosures:
Aya Akhras indicated no relevant financial relationships.
Oscar Hernandez indicated no relevant financial relationships.
Ramasamy Nathan indicated no relevant financial relationships.
Aya Akhras, MD, Oscar Hernandez, MD, Ramasamy Nathan, MD. P4986 - Superior Vena Cava Syndrome: A Rare but Severe Complication of Mega-Esophagus in Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

