Tuesday Poster Session
Category: Esophagus
A Non-Stent Management of Esophageal Perforation Secondary to <i>Candida</i> Esophagitis Near the Gastroesophageal Junction
P4983 - A Non-Stent Management of Esophageal Perforation Secondary to Candida Esophagitis Near the Gastroesophageal Junction
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shyamal Sheth, DO (he/him/his)
Franciscan Health Olympia Fields
Chicago, IL
Presenting Author(s)
Shyamal Sheth, DO1, Smrithi Valsaraj, MD1, Jay Shah, DO, MSc2, Amer Alsamman, MD3
1Franciscan Health Olympia Fields, Chicago, IL; 2Franciscan Health, Olympia Fields, IL; 3Franciscan Health Olympia Fields, Olympia Fields, IL
Introduction: Esophageal candidiasis, most commonly caused by Candida albicans, typically affects immunocompromised individuals. While usually treatable with antifungals, esophageal perforation is an exceedingly rare complication. We present a rare case of esophageal candidiasis leading to perforation near the gastroesophageal junction, successfully treated without stent placement.
Case Description/
Methods: A 61-year-old male who recently completed fluconazole therapy for esophageal candidiasis presented with coffee ground emesis and dyspnea. On arrival, he was hypotensive, tachycardic, and tachypneic. Physical examination revealed increased work of breathing and epigastric tenderness. Labs were remarkable for a severe lactic acidosis ( > 17 mmmol/L) with mildly elevated white blood cell count (12.4 x 109/L). A chest radiograph demonstrated a left-sided hydropneumothorax, which was confirmed on CT imaging along with severe distal esophageal thickening. An emergent chest tube was placed, draining serosanginous fluid with aggregated food particles. Pleural fluid analysis was consistent with an exudative effusion, with cultures growing Candida Albicans, leading to initiation of intravenous micafungin therapy. A CT chest with oral gastrografin was obtained that showed contrast leakage from the left lateral esophageal wall into the left hemithorax, raising suspicion for a bronchoesophageal fistula versus esophageal perforation. Patient was then transferred to a tertiary facility where cardiothoracic surgery performed an esophagogastroduodenoscopy with video-assisted thorascopic surgery confirmed esophageal perforation at 27 cm from the incisors, close to the GE junction. Esophageal stenting was avoided due to the proximity GE junction. The patient received nasogastric feeds, IV fluconazole, and PPIs. A subsequent esophagogram showed distal esophageal erosions and focal strictures without leakage. Six weeks later, a chest CT confirmed hydropneumothorax resolution and no perforation.
Discussion: While esophageal candidiasis is common, perforation is a rare but serious complication, with mortality rates ranging from 4% to 80%. Management depends on the perforation site and clinical status, with stenting being a less invasive option for high-risk patients. However, stents near the GE junction often migrate distally (7–75%). In select patients without mediastinitis or large perforation, non-operative management with antifungals, proton pump inhibitors, and supportive care may be a viable alternative.
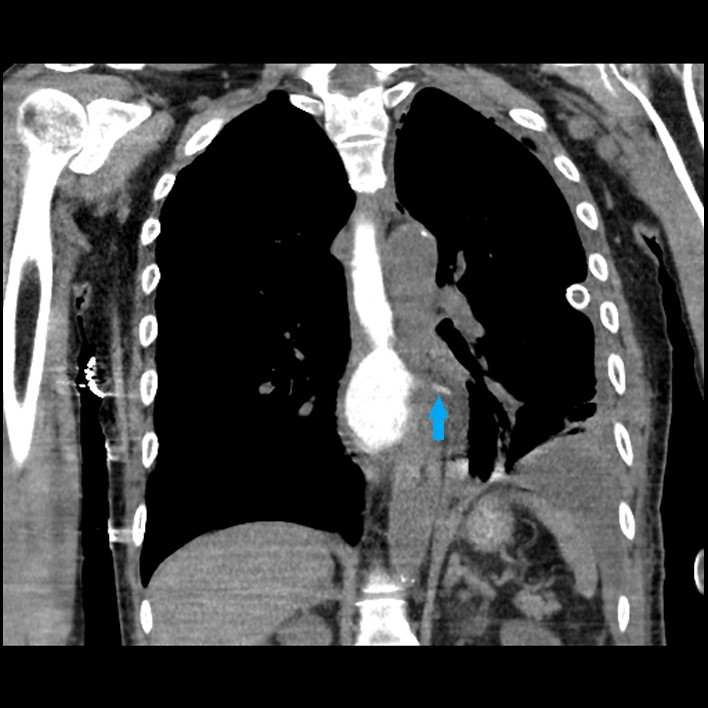
Figure: CT chest with oral gastrografin coronal and axial views showing oral contrast leaking
from the posterior left esophageal lumen into the left hemithorax.
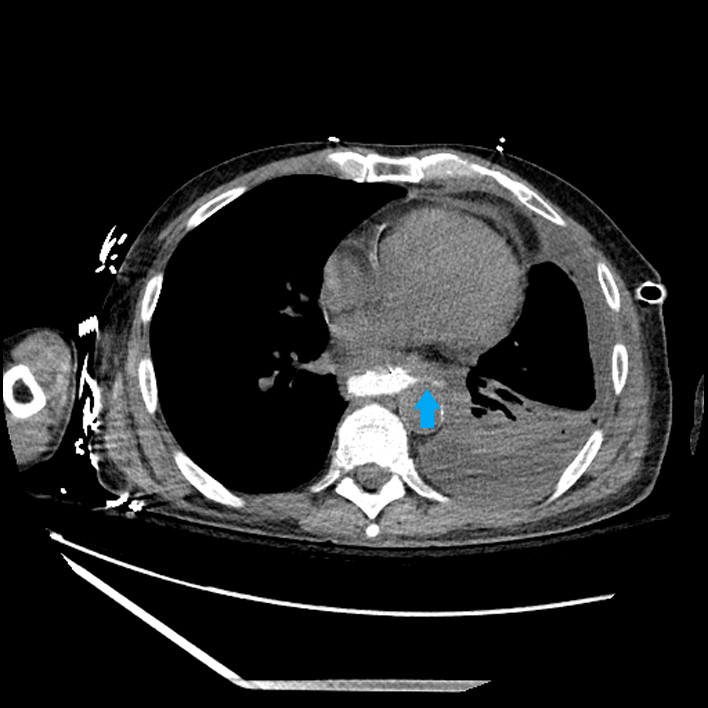
Figure: CT chest with oral gastrografin coronal and axial views showing oral contrast leaking
from the posterior left esophageal lumen into the left hemithorax.
Disclosures:
Shyamal Sheth indicated no relevant financial relationships.
Smrithi Valsaraj indicated no relevant financial relationships.
Jay Shah indicated no relevant financial relationships.
Amer Alsamman indicated no relevant financial relationships.
Shyamal Sheth, DO1, Smrithi Valsaraj, MD1, Jay Shah, DO, MSc2, Amer Alsamman, MD3. P4983 - A Non-Stent Management of Esophageal Perforation Secondary to <i>Candida</i> Esophagitis Near the Gastroesophageal Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Chicago, IL; 2Franciscan Health, Olympia Fields, IL; 3Franciscan Health Olympia Fields, Olympia Fields, IL
Introduction: Esophageal candidiasis, most commonly caused by Candida albicans, typically affects immunocompromised individuals. While usually treatable with antifungals, esophageal perforation is an exceedingly rare complication. We present a rare case of esophageal candidiasis leading to perforation near the gastroesophageal junction, successfully treated without stent placement.
Case Description/
Methods: A 61-year-old male who recently completed fluconazole therapy for esophageal candidiasis presented with coffee ground emesis and dyspnea. On arrival, he was hypotensive, tachycardic, and tachypneic. Physical examination revealed increased work of breathing and epigastric tenderness. Labs were remarkable for a severe lactic acidosis ( > 17 mmmol/L) with mildly elevated white blood cell count (12.4 x 109/L). A chest radiograph demonstrated a left-sided hydropneumothorax, which was confirmed on CT imaging along with severe distal esophageal thickening. An emergent chest tube was placed, draining serosanginous fluid with aggregated food particles. Pleural fluid analysis was consistent with an exudative effusion, with cultures growing Candida Albicans, leading to initiation of intravenous micafungin therapy. A CT chest with oral gastrografin was obtained that showed contrast leakage from the left lateral esophageal wall into the left hemithorax, raising suspicion for a bronchoesophageal fistula versus esophageal perforation. Patient was then transferred to a tertiary facility where cardiothoracic surgery performed an esophagogastroduodenoscopy with video-assisted thorascopic surgery confirmed esophageal perforation at 27 cm from the incisors, close to the GE junction. Esophageal stenting was avoided due to the proximity GE junction. The patient received nasogastric feeds, IV fluconazole, and PPIs. A subsequent esophagogram showed distal esophageal erosions and focal strictures without leakage. Six weeks later, a chest CT confirmed hydropneumothorax resolution and no perforation.
Discussion: While esophageal candidiasis is common, perforation is a rare but serious complication, with mortality rates ranging from 4% to 80%. Management depends on the perforation site and clinical status, with stenting being a less invasive option for high-risk patients. However, stents near the GE junction often migrate distally (7–75%). In select patients without mediastinitis or large perforation, non-operative management with antifungals, proton pump inhibitors, and supportive care may be a viable alternative.
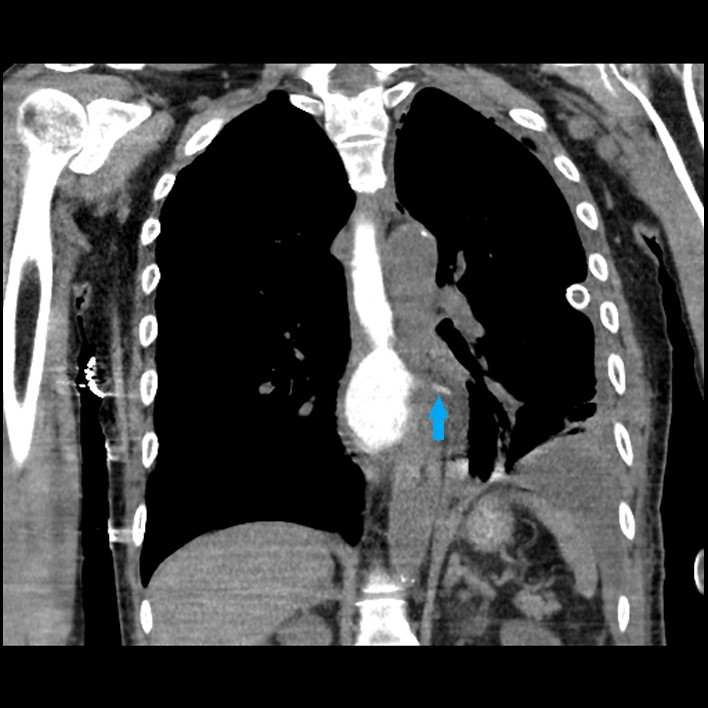
Figure: CT chest with oral gastrografin coronal and axial views showing oral contrast leaking
from the posterior left esophageal lumen into the left hemithorax.
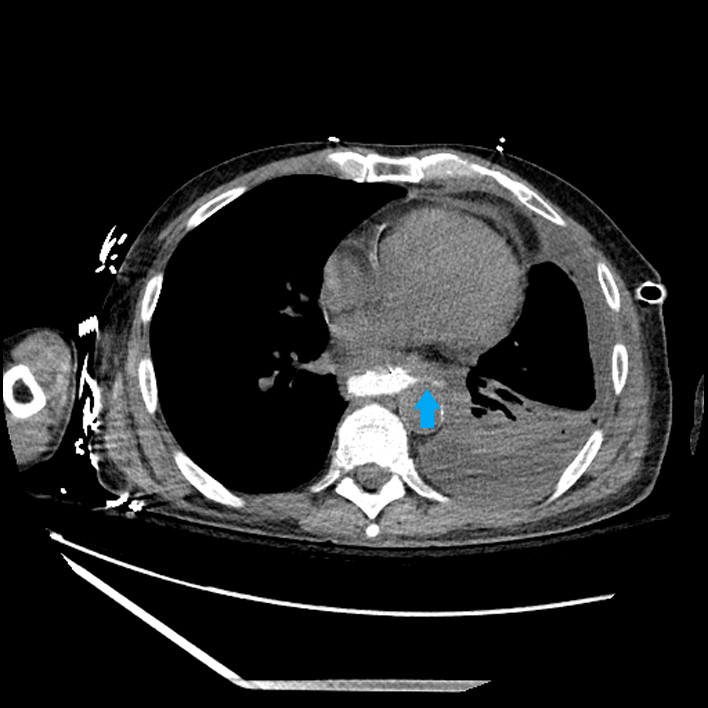
Figure: CT chest with oral gastrografin coronal and axial views showing oral contrast leaking
from the posterior left esophageal lumen into the left hemithorax.
Disclosures:
Shyamal Sheth indicated no relevant financial relationships.
Smrithi Valsaraj indicated no relevant financial relationships.
Jay Shah indicated no relevant financial relationships.
Amer Alsamman indicated no relevant financial relationships.
Shyamal Sheth, DO1, Smrithi Valsaraj, MD1, Jay Shah, DO, MSc2, Amer Alsamman, MD3. P4983 - A Non-Stent Management of Esophageal Perforation Secondary to <i>Candida</i> Esophagitis Near the Gastroesophageal Junction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
