Tuesday Poster Session
Category: Esophagus
P4981 - When Textbook Meets Reality: A Rare Case of Boerhaave’s Syndrome with Mackler’s Triad
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Taiwo Ajani, MD (he/him/his)
University of Texas Rio Grande Valley
McAllen, TX
Presenting Author(s)
Taiwo Ajani, MD, Jose Loayza Pintado, MD, Nayiri Derian, MD, Andres Suarez Parraga, MD, Ernesto Garza, MD
University of Texas Rio Grande Valley, McAllen, TX
Introduction: Boerhaave’s syndrome is a rare, life-threatening cause of esophageal perforation, typically triggered by forceful vomiting and often misdiagnosed due to nonspecific symptoms. Although Mackler’s triad is classically described, it is infrequently observed. Prompt recognition and imaging are vital, as early intervention dramatically improves outcomes. We report a striking case of Boerhaave’s syndrome in a young man presenting with the complete triad.
Case Description/
Methods: A 32-year-old man with ulcerative colitis presented with acute chest pain and repeated vomiting following dinner. He reported food impaction sensation and sought care two hours after symptom onset. Examination revealed subcutaneous emphysema and abdominal tenderness; imaging confirmed pneumomediastinum, pneumoperitoneum, and a distal esophageal perforation consistent with Boerhaave’s syndrome. He underwent emergent robotic-assisted laparoscopic repair with fundoplication, esophageal stenting, and drainage. Postoperative recovery included antibiotics and gradual diet advancement but was complicated by a pleural effusion requiring thoracentesis. Furthermore, a mild ulcerative colitis (UC) flare was managed with mesalamine. He was discharged on postoperative day nine in stable condition, with follow-up showing full radiologic recovery at three months.
Discussion: Boerhaave’s syndrome, a spontaneous full-thickness esophageal rupture typically caused by forceful vomiting, is a rare but life-threatening condition. While Mackler’s triad is a classic diagnostic marker, it appears in fewer than 15% of cases, making our patient’s complete presentation diagnostically valuable. Esophageal perforation often mimics other critical conditions, making timely recognition challenging. Imaging, particularly contrast-enhanced CT, plays a pivotal role in diagnosis and treatment planning. Management strategies vary depending on the severity and containment. Our patient underwent early robotic-assisted laparoscopic repair with anterior fundoplication and endoscopic stenting, supported by drainage and broad-spectrum antibiotics. His age and concurrent ulcerative colitis added clinical complexity, requiring coordinated multidisciplinary care. This case highlights the importance of heightened suspicion of Boerhaave’s syndrome in atypical patients. It reflects how early, minimally invasive intervention, paired with comprehensive care, can lead to successful outcomes in what is otherwise a high-risk clinical emergency.
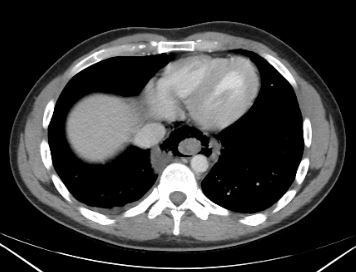
Figure: Image 1. Computed Tomography (CT) of the Chest with Oral Contrast - Axial view
Prominent pneumomediastinum is seen surrounding the esophagus.

Figure: Image 2. Computed Tomography (CT) of the Chest with Oral Contrast - Sagital view
Pneumomediastinum tracking along the esophageal course, with extension of free air into the upper abdomen, consistent with pneumoperitoneum due to esophageal rupture.
Disclosures:
Taiwo Ajani indicated no relevant financial relationships.
Jose Loayza Pintado indicated no relevant financial relationships.
Nayiri Derian indicated no relevant financial relationships.
Andres Suarez Parraga indicated no relevant financial relationships.
Ernesto Garza indicated no relevant financial relationships.
Taiwo Ajani, MD, Jose Loayza Pintado, MD, Nayiri Derian, MD, Andres Suarez Parraga, MD, Ernesto Garza, MD. P4981 - When Textbook Meets Reality: A Rare Case of Boerhaave’s Syndrome with Mackler’s Triad, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Rio Grande Valley, McAllen, TX
Introduction: Boerhaave’s syndrome is a rare, life-threatening cause of esophageal perforation, typically triggered by forceful vomiting and often misdiagnosed due to nonspecific symptoms. Although Mackler’s triad is classically described, it is infrequently observed. Prompt recognition and imaging are vital, as early intervention dramatically improves outcomes. We report a striking case of Boerhaave’s syndrome in a young man presenting with the complete triad.
Case Description/
Methods: A 32-year-old man with ulcerative colitis presented with acute chest pain and repeated vomiting following dinner. He reported food impaction sensation and sought care two hours after symptom onset. Examination revealed subcutaneous emphysema and abdominal tenderness; imaging confirmed pneumomediastinum, pneumoperitoneum, and a distal esophageal perforation consistent with Boerhaave’s syndrome. He underwent emergent robotic-assisted laparoscopic repair with fundoplication, esophageal stenting, and drainage. Postoperative recovery included antibiotics and gradual diet advancement but was complicated by a pleural effusion requiring thoracentesis. Furthermore, a mild ulcerative colitis (UC) flare was managed with mesalamine. He was discharged on postoperative day nine in stable condition, with follow-up showing full radiologic recovery at three months.
Discussion: Boerhaave’s syndrome, a spontaneous full-thickness esophageal rupture typically caused by forceful vomiting, is a rare but life-threatening condition. While Mackler’s triad is a classic diagnostic marker, it appears in fewer than 15% of cases, making our patient’s complete presentation diagnostically valuable. Esophageal perforation often mimics other critical conditions, making timely recognition challenging. Imaging, particularly contrast-enhanced CT, plays a pivotal role in diagnosis and treatment planning. Management strategies vary depending on the severity and containment. Our patient underwent early robotic-assisted laparoscopic repair with anterior fundoplication and endoscopic stenting, supported by drainage and broad-spectrum antibiotics. His age and concurrent ulcerative colitis added clinical complexity, requiring coordinated multidisciplinary care. This case highlights the importance of heightened suspicion of Boerhaave’s syndrome in atypical patients. It reflects how early, minimally invasive intervention, paired with comprehensive care, can lead to successful outcomes in what is otherwise a high-risk clinical emergency.
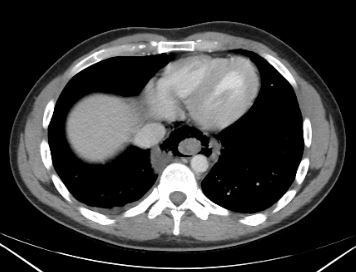
Figure: Image 1. Computed Tomography (CT) of the Chest with Oral Contrast - Axial view
Prominent pneumomediastinum is seen surrounding the esophagus.

Figure: Image 2. Computed Tomography (CT) of the Chest with Oral Contrast - Sagital view
Pneumomediastinum tracking along the esophageal course, with extension of free air into the upper abdomen, consistent with pneumoperitoneum due to esophageal rupture.
Disclosures:
Taiwo Ajani indicated no relevant financial relationships.
Jose Loayza Pintado indicated no relevant financial relationships.
Nayiri Derian indicated no relevant financial relationships.
Andres Suarez Parraga indicated no relevant financial relationships.
Ernesto Garza indicated no relevant financial relationships.
Taiwo Ajani, MD, Jose Loayza Pintado, MD, Nayiri Derian, MD, Andres Suarez Parraga, MD, Ernesto Garza, MD. P4981 - When Textbook Meets Reality: A Rare Case of Boerhaave’s Syndrome with Mackler’s Triad, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
