Tuesday Poster Session
Category: Esophagus
P4979 - The Swiss Cheese Esophagus: A Rare Case of Intramural Pseudodiverticulosis Causing Progressive Dysphagia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amirali Tavangar, MD
University of California Irvine Digestive Health Institute
Orange, CA
Presenting Author(s)
Amirali Tavangar, MD1, Suhail Sidhu, MD2, Andy Lin, MD2, Marie Balfour, MD3, Trevor McCracken, MD2, Momin Masroor, MD2, Peter Nguyen, MD2, Gregory Albers, MD, FACG2, Christina Ling, MD2
1University of California Irvine Digestive Health Institute, Orange, CA; 2University of California Irvine, Orange, CA; 3University of California Irvine Health, Orange, CA
Introduction: Esophageal intramural pseudodiverticulosis (EIPD) is a rare condition characterized by dilated excretory ducts of submucosal esophageal glands. It typically presents with progressive dysphagia in middle-aged patients and is frequently under-recognized. Though its pathogenesis remains unclear, associations include Candida esophagitis, eosinophilic esophagitis (EoE), and esophageal motility disorders1.
Case Description/
Methods: A 48-year-old female with advanced fallopian tube cancer s/p resection on chemotherapy presented with progressive solid food dysphagia. Her prior endoscopies had shown EoE and an esophageal stricture which required multiple balloon dilations. Follow-up endoscopy showed proximal stricture, concentric rings, white plaques, and numerous intramural pseudodiverticula (Figures 1 and 2). Brush cytology confirmed candida esophagitis. Biopsies revealed lymphocyte-predominant esophagitis with Civatte bodies. She was treated with high-dose proton pump inhibitors and antifungals.
Discussion: This case illustrates the complex interplay of infectious and inflammatory processes leading to EIPD. Our patient’s history of EoE transitioning to lymphocytic esophagitis, candida infection, and development of EIPD supports the hypothesis that chronic mucosal inflammation and altered immunity may contribute to ductal obstruction and pseudodiverticulum formation. Proximal stenosis in EIPD is likely due to the high density of submucosal glands in the upper esophagus2. EIPD should be considered in patients with recurrent dysphagia and overlapping esophagitis phenotypes, warranting thorough endoscopic evaluation. Management is generally conservative, focusing on controlling inflammation and preventing complications. Treatment may include antifungal therapy for Candida, acid suppression, endoscopic dilation for stenosis and smoking cessation. Early recognition and tailored intervention are essential to minimize chronic morbidity.
References
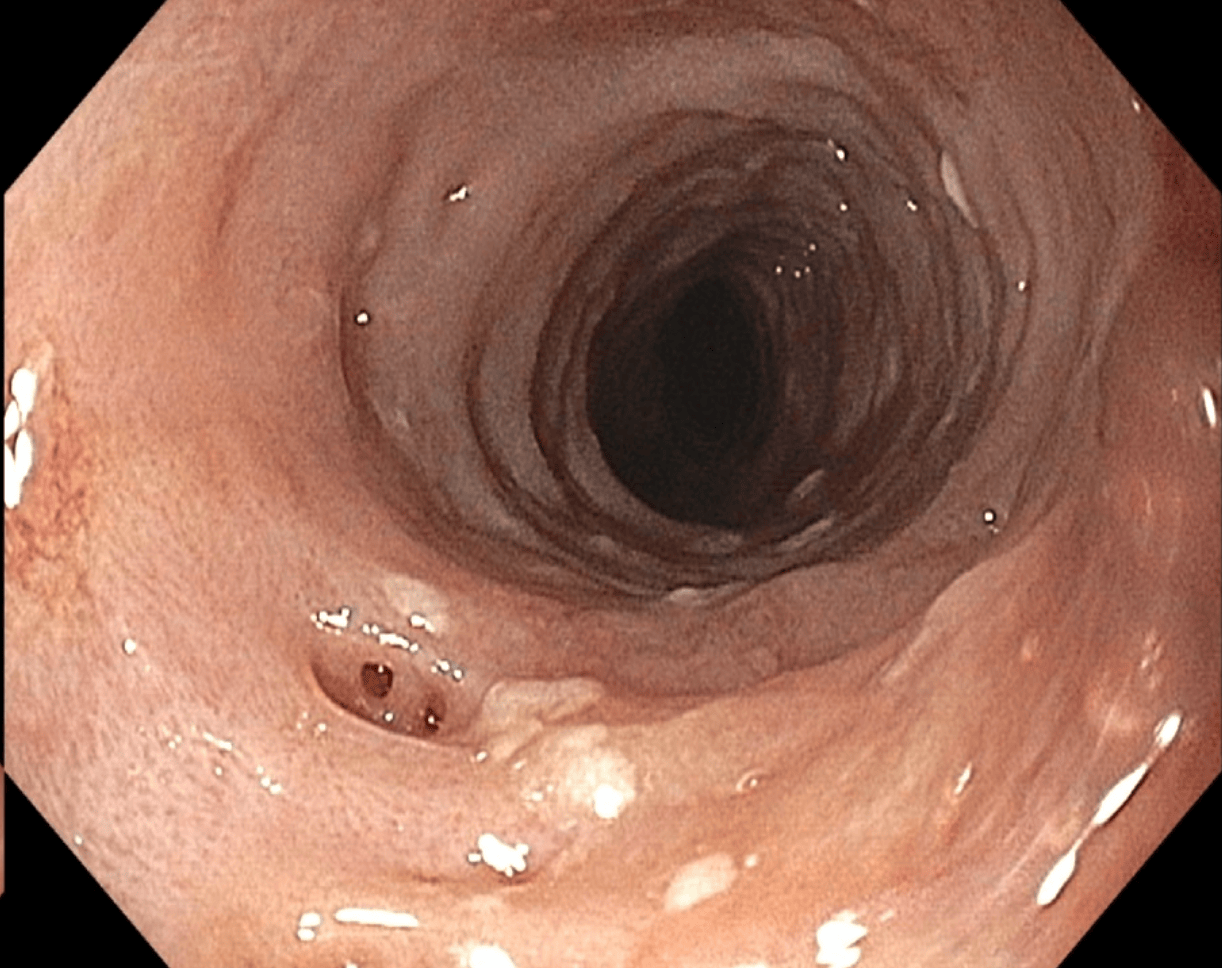
Figure: Figure 1: Endoscopic image showing multiple small mucosal openings in the proximal esophagus, consistent with EIPD.
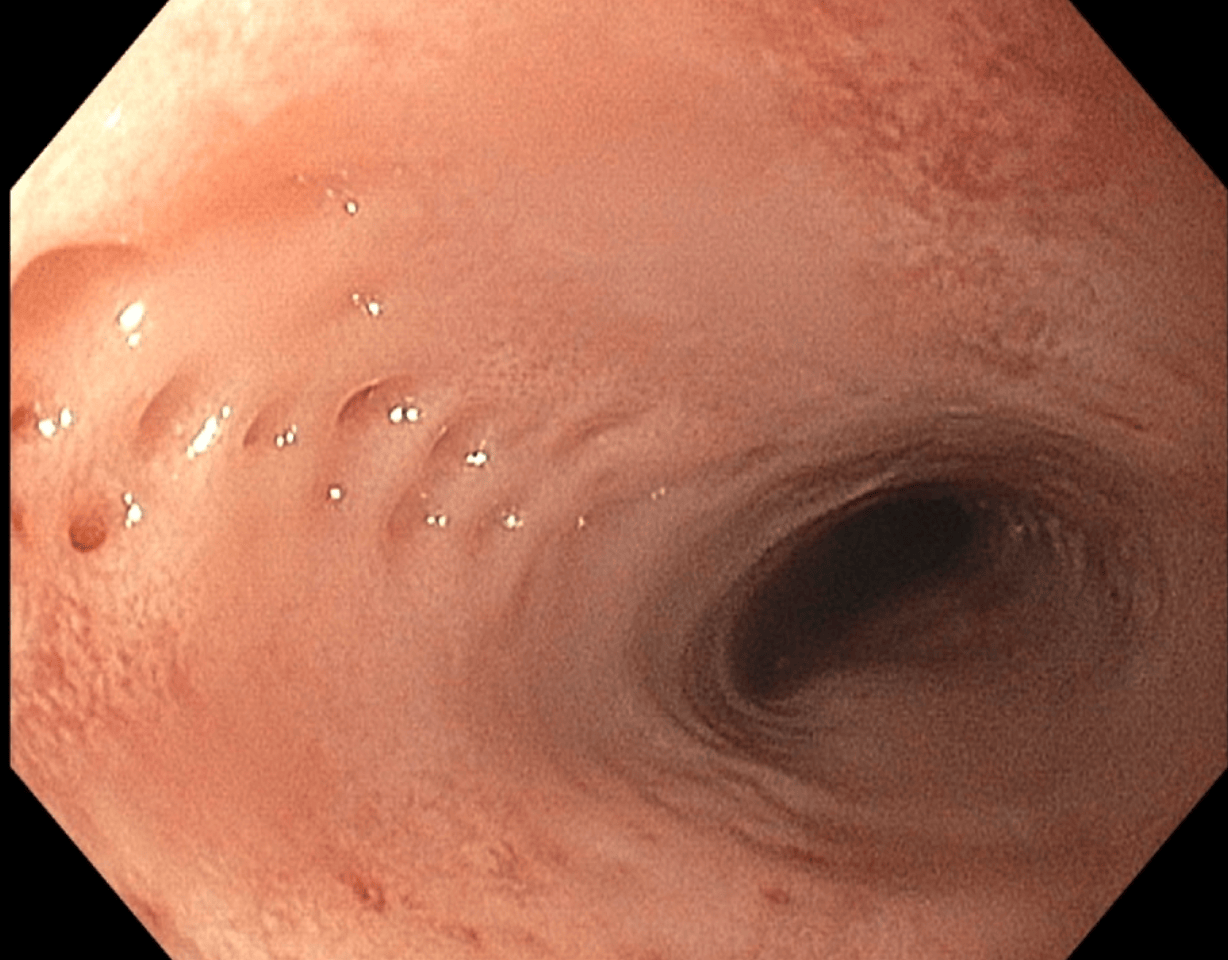
Figure: Figure 2: Endoscopic image consistent with Candida esophagitis in the mid-esophagus, accompanied by pseudodiverticulosis.
Disclosures:
Amirali Tavangar indicated no relevant financial relationships.
Suhail Sidhu indicated no relevant financial relationships.
Andy Lin indicated no relevant financial relationships.
Marie Balfour indicated no relevant financial relationships.
Trevor McCracken indicated no relevant financial relationships.
Momin Masroor indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Gregory Albers: Nestle Pharmaceuticals – Speakers Bureau.
Christina Ling indicated no relevant financial relationships.
Amirali Tavangar, MD1, Suhail Sidhu, MD2, Andy Lin, MD2, Marie Balfour, MD3, Trevor McCracken, MD2, Momin Masroor, MD2, Peter Nguyen, MD2, Gregory Albers, MD, FACG2, Christina Ling, MD2. P4979 - The Swiss Cheese Esophagus: A Rare Case of Intramural Pseudodiverticulosis Causing Progressive Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Irvine Digestive Health Institute, Orange, CA; 2University of California Irvine, Orange, CA; 3University of California Irvine Health, Orange, CA
Introduction: Esophageal intramural pseudodiverticulosis (EIPD) is a rare condition characterized by dilated excretory ducts of submucosal esophageal glands. It typically presents with progressive dysphagia in middle-aged patients and is frequently under-recognized. Though its pathogenesis remains unclear, associations include Candida esophagitis, eosinophilic esophagitis (EoE), and esophageal motility disorders1.
Case Description/
Methods: A 48-year-old female with advanced fallopian tube cancer s/p resection on chemotherapy presented with progressive solid food dysphagia. Her prior endoscopies had shown EoE and an esophageal stricture which required multiple balloon dilations. Follow-up endoscopy showed proximal stricture, concentric rings, white plaques, and numerous intramural pseudodiverticula (Figures 1 and 2). Brush cytology confirmed candida esophagitis. Biopsies revealed lymphocyte-predominant esophagitis with Civatte bodies. She was treated with high-dose proton pump inhibitors and antifungals.
Discussion: This case illustrates the complex interplay of infectious and inflammatory processes leading to EIPD. Our patient’s history of EoE transitioning to lymphocytic esophagitis, candida infection, and development of EIPD supports the hypothesis that chronic mucosal inflammation and altered immunity may contribute to ductal obstruction and pseudodiverticulum formation. Proximal stenosis in EIPD is likely due to the high density of submucosal glands in the upper esophagus2. EIPD should be considered in patients with recurrent dysphagia and overlapping esophagitis phenotypes, warranting thorough endoscopic evaluation. Management is generally conservative, focusing on controlling inflammation and preventing complications. Treatment may include antifungal therapy for Candida, acid suppression, endoscopic dilation for stenosis and smoking cessation. Early recognition and tailored intervention are essential to minimize chronic morbidity.
References
- Shintaku M. World Journal of Gastroenterology. 2024 Jan 14; 30(2): 137.
- Halm U, Lamberts R, Knigge I, Mössner J, Zachäus M. Diseases of the Esophagus. 2014 Apr 1; 27(3): 230–234.
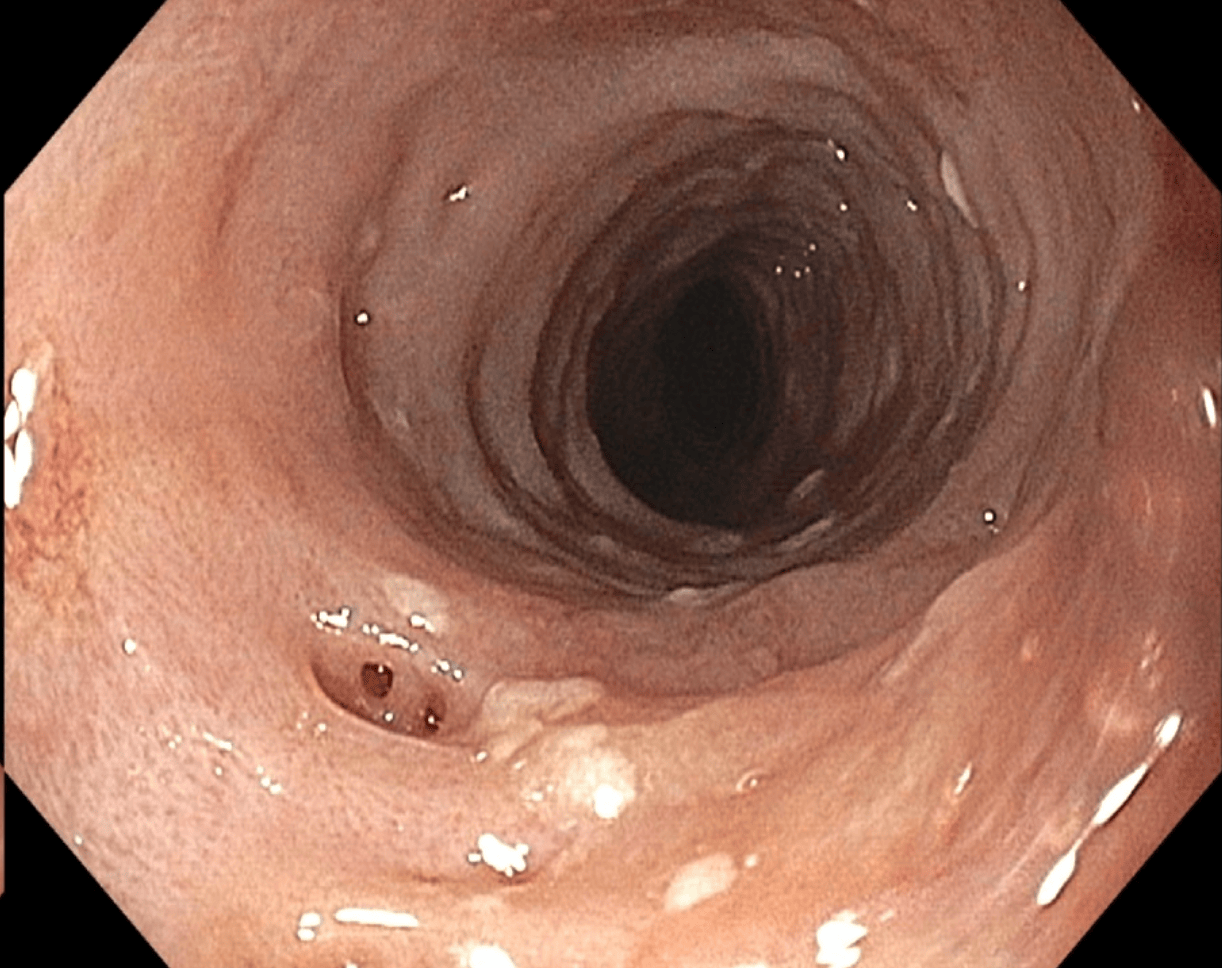
Figure: Figure 1: Endoscopic image showing multiple small mucosal openings in the proximal esophagus, consistent with EIPD.
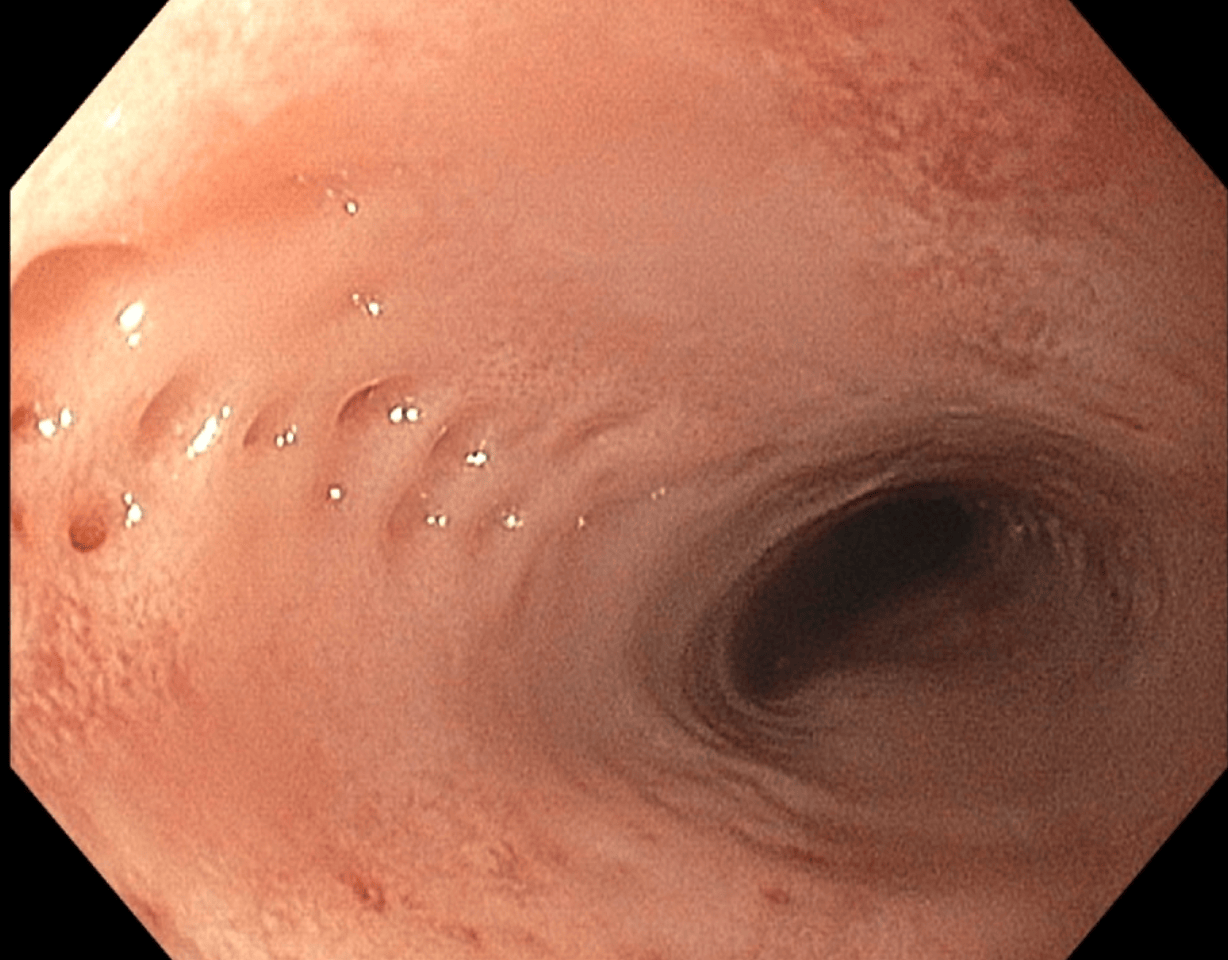
Figure: Figure 2: Endoscopic image consistent with Candida esophagitis in the mid-esophagus, accompanied by pseudodiverticulosis.
Disclosures:
Amirali Tavangar indicated no relevant financial relationships.
Suhail Sidhu indicated no relevant financial relationships.
Andy Lin indicated no relevant financial relationships.
Marie Balfour indicated no relevant financial relationships.
Trevor McCracken indicated no relevant financial relationships.
Momin Masroor indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Gregory Albers: Nestle Pharmaceuticals – Speakers Bureau.
Christina Ling indicated no relevant financial relationships.
Amirali Tavangar, MD1, Suhail Sidhu, MD2, Andy Lin, MD2, Marie Balfour, MD3, Trevor McCracken, MD2, Momin Masroor, MD2, Peter Nguyen, MD2, Gregory Albers, MD, FACG2, Christina Ling, MD2. P4979 - The Swiss Cheese Esophagus: A Rare Case of Intramural Pseudodiverticulosis Causing Progressive Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
