Tuesday Poster Session
Category: Esophagus
P4978 - Type 2 Achalasia in a Patient With History of Pulmonic Valve Replacement
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jonathan Ghobrial, MD
Allegheny Health Network Medicine Institute
Pittsburgh, PA
Presenting Author(s)
Jonathan Ghobrial, MD1, Scarlett Austin, DO2, Nabeeha Mohy-Ud-Din, MD3
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA
Introduction: We present a case of a 29-year-old patient who was ultimately diagnosed with type 2 achalasia following childhood cardiac surgery.
Case Description/
Methods: The patient is a 29-year-old male with a past medical history of congenital, bronchomalacia, pulmonic valves stenosis with valve replacement during childhood, congenital atrial septal defect, anxiety, and cyclic vomiting syndrome who reported progressive post-prandial emesis for two years, now occurring following every meal. For further evaluation an outpatient esophagogastroduodenoscopy (EGD) was attempted; however, the procedure was aborted due to aspiration resulting in hypoxia. He was subsequently admitted to the hospital for further care. Computed tomography (CT) imaging of the chest noted dilation with debris throughout the entire esophagus. EGD was reattempted, with intubation to minimize the risk of aspiration. The EGD re-demonstrated food in the entire esophagus, severe dilation of the esophageal lumen, and a puckered appearance of the gastroesophageal junction. Due to the extensive amount of food in the esophagus, numerous EGDs were required for complete clearance.
Discussion: Type 2 achalasia involves absence of peristalsis and contractile activity in the esophagus with a panesophageal pressurization greater than 30 mm Hg (1). Major causes of achalasia include infection and malignancy. However, this patient did not have common risk factors such as sick contacts, recent travel, and immunodeficiency. A notable aspect of this patient’s history is his cardiac history during childhood and congenital bronchomalacia, which could both be contributing factors to his development of type 2 achalasia. There were no available records regarding the types of procedures he underwent in childhood. The last important aspect of this case is the time to development of achalasia. If his surgical history as a child was the only contributing factor to developing achalasia, the onset of symptoms nearly two decades after insult makes this case unlike other presentations where the time course is usually much shorter. This case adds to the list of the potential causes of type 2 achalasia and the timeframe for developing symptoms.
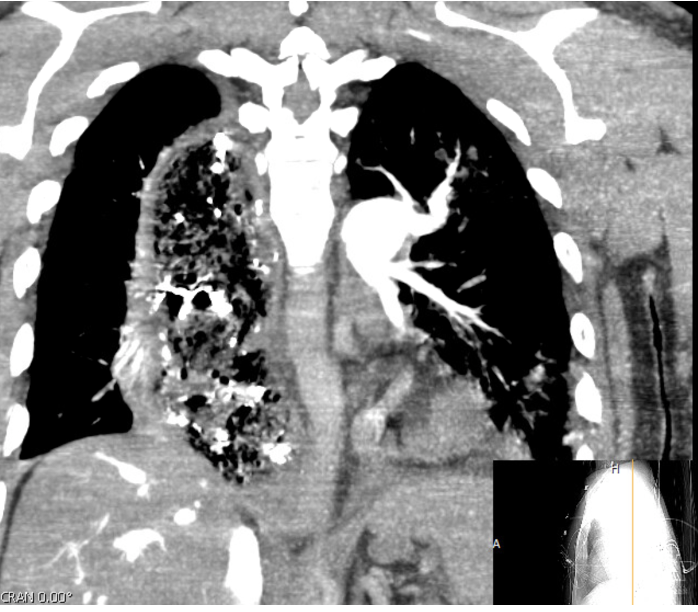
Figure: CT chest without contrast demonstrating retained debris and severe esophageal dilatation.
Disclosures:
Jonathan Ghobrial indicated no relevant financial relationships.
Scarlett Austin indicated no relevant financial relationships.
Nabeeha Mohy-Ud-Din indicated no relevant financial relationships.
Jonathan Ghobrial, MD1, Scarlett Austin, DO2, Nabeeha Mohy-Ud-Din, MD3. P4978 - Type 2 Achalasia in a Patient With History of Pulmonic Valve Replacement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Health Network Medicine Institute, Pittsburgh, PA; 2Allegheny Center for Digestive Health, Pittsburgh, PA; 3Allegheny Health Network, Pittsburgh, PA
Introduction: We present a case of a 29-year-old patient who was ultimately diagnosed with type 2 achalasia following childhood cardiac surgery.
Case Description/
Methods: The patient is a 29-year-old male with a past medical history of congenital, bronchomalacia, pulmonic valves stenosis with valve replacement during childhood, congenital atrial septal defect, anxiety, and cyclic vomiting syndrome who reported progressive post-prandial emesis for two years, now occurring following every meal. For further evaluation an outpatient esophagogastroduodenoscopy (EGD) was attempted; however, the procedure was aborted due to aspiration resulting in hypoxia. He was subsequently admitted to the hospital for further care. Computed tomography (CT) imaging of the chest noted dilation with debris throughout the entire esophagus. EGD was reattempted, with intubation to minimize the risk of aspiration. The EGD re-demonstrated food in the entire esophagus, severe dilation of the esophageal lumen, and a puckered appearance of the gastroesophageal junction. Due to the extensive amount of food in the esophagus, numerous EGDs were required for complete clearance.
Discussion: Type 2 achalasia involves absence of peristalsis and contractile activity in the esophagus with a panesophageal pressurization greater than 30 mm Hg (1). Major causes of achalasia include infection and malignancy. However, this patient did not have common risk factors such as sick contacts, recent travel, and immunodeficiency. A notable aspect of this patient’s history is his cardiac history during childhood and congenital bronchomalacia, which could both be contributing factors to his development of type 2 achalasia. There were no available records regarding the types of procedures he underwent in childhood. The last important aspect of this case is the time to development of achalasia. If his surgical history as a child was the only contributing factor to developing achalasia, the onset of symptoms nearly two decades after insult makes this case unlike other presentations where the time course is usually much shorter. This case adds to the list of the potential causes of type 2 achalasia and the timeframe for developing symptoms.
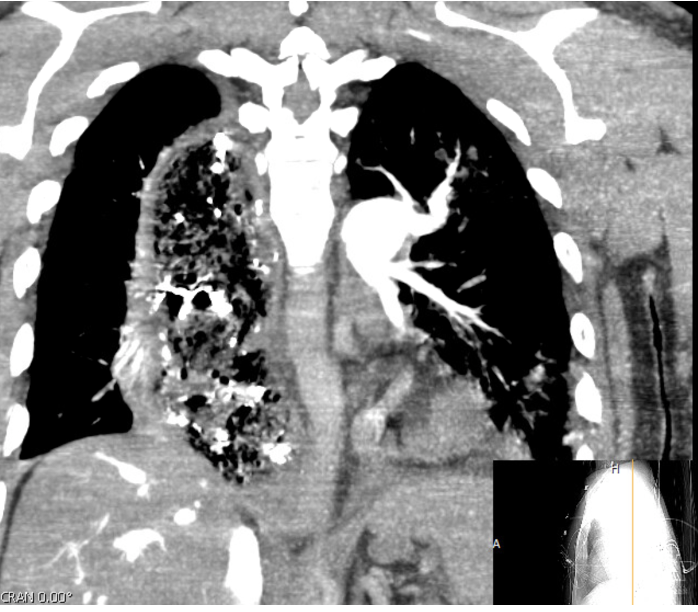
Figure: CT chest without contrast demonstrating retained debris and severe esophageal dilatation.
Disclosures:
Jonathan Ghobrial indicated no relevant financial relationships.
Scarlett Austin indicated no relevant financial relationships.
Nabeeha Mohy-Ud-Din indicated no relevant financial relationships.
Jonathan Ghobrial, MD1, Scarlett Austin, DO2, Nabeeha Mohy-Ud-Din, MD3. P4978 - Type 2 Achalasia in a Patient With History of Pulmonic Valve Replacement, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
