Tuesday Poster Session
Category: Esophagus
P4973 - A Case of Postoperative Intramural Esophageal Hematoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DR
Deirdre Reidy, MD
NewYork-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Deirdre Reidy, MD1, Lauren Callans, MD2, Sean Rangwani, MD, MBA3, Emily S. Smith, MD1, Carl V. Crawford, MD1, David Wan, MD4
1NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 2Weill Cornell Medicine, New York, NY; 3NewYork-Presbyterian / Weill Cornell Medical Center, New Albany, OH; 4NewYork-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction: Intramural esophageal hematomas (IEH) are rare, but important cause of acute chest pain and dysphagia and can mimic life-threatening cardiothoracic and esophageal conditions. Identification requires a high index of suspicion for timely diagnosis and appropriate management.
Case Description/
Methods: A 76-year-old male with hyperlipidemia, type 2 diabetes, coronary artery disease with multiple stents (on aspirin and clopidogrel), and invasive adenocarcinoma status post left upper lobe lobectomy, underwent a left chest wall desmoid fibromatosis resection. Dual-antiplatelet therapy was held 3-5 days prior to procedure. On post-operative day 3, he developed acute dysphagia and was unable to tolerate oral secretions. Urgent CT scan of the chest showed a distended esophagus with debris, concerning for luminal obstruction. Esophagogastroduodenoscopy (EGD) revealed a large esophageal hematoma causing mid-to-distal luminal narrowing of the esophagus, with hematin seen throughout the stomach. The patient was started on omeprazole, a nasogastric tube was placed, and diet was gradually advanced. On the day of discharge (post-EGD day 3), a subsequent esophagogram showed resolution of obstruction with return of normal swallow function. He was discharged on single antiplatelet therapy with aspirin. At 8-month follow-up, he reported normal swallowing and repeat chest CT showed resolution of the hematoma.
Discussion: IEHs are rare entities that typically present with chest pain, dysphagia, and hematemesis and can mimic other cardiac or esophageal emergencies. They may occur spontaneously, or more commonly following esophageal instrumentation, trauma, or excessive retching and vomiting. Antiplatelet and anticoagulation therapy increases bleeding risk, predisposing patients to hematoma formation. Diagnosis is established through imaging (CT with IV contrast favored) followed by endoscopy. Esophagograms are useful to assess obstruction and swallowing function after the hematoma has been diagnosed. Most cases resolve with conservative treatment and without intervention. For this patient, esophageal stenting was deferred and conservative treatment was favored based on stable hemoglobin and successful passage of the endoscope past the hematoma. Hemoglobin remained stable following endoscopy. In this patient, the development of the IEH was likely multifactorial, including recent surgical stress and manipulation, underlying comorbidities, and recent use of dual-antiplatelet therapy.
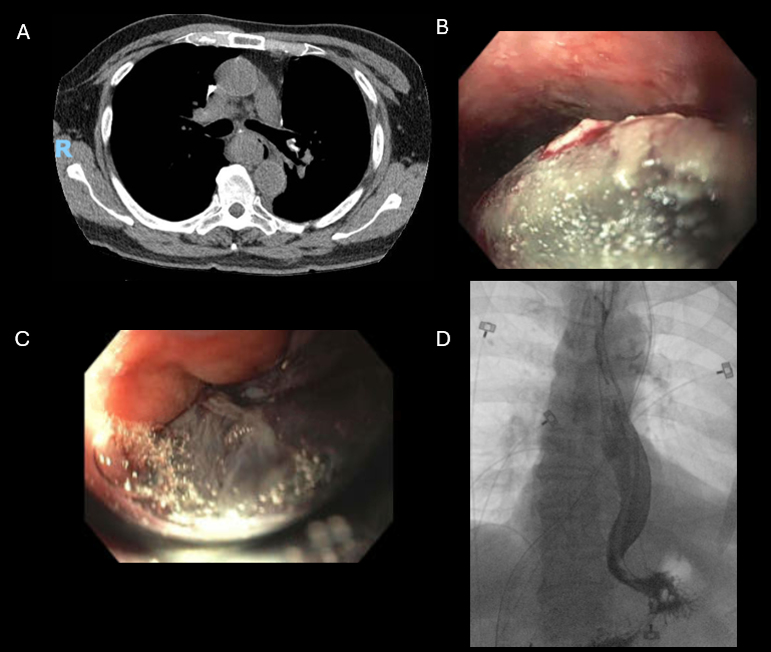
Figure: Figure 1 - A: Axial chest CT without contrast. B: Middle third of esophagus. C: Lower third of esophagus. D: Fluoroscopic imaging during esophagogastroduodenoscopy.
Disclosures:
Deirdre Reidy indicated no relevant financial relationships.
Lauren Callans indicated no relevant financial relationships.
Sean Rangwani indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
David Wan: Medtronic – Data Monitoring Committee.
Deirdre Reidy, MD1, Lauren Callans, MD2, Sean Rangwani, MD, MBA3, Emily S. Smith, MD1, Carl V. Crawford, MD1, David Wan, MD4. P4973 - A Case of Postoperative Intramural Esophageal Hematoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY; 2Weill Cornell Medicine, New York, NY; 3NewYork-Presbyterian / Weill Cornell Medical Center, New Albany, OH; 4NewYork-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction: Intramural esophageal hematomas (IEH) are rare, but important cause of acute chest pain and dysphagia and can mimic life-threatening cardiothoracic and esophageal conditions. Identification requires a high index of suspicion for timely diagnosis and appropriate management.
Case Description/
Methods: A 76-year-old male with hyperlipidemia, type 2 diabetes, coronary artery disease with multiple stents (on aspirin and clopidogrel), and invasive adenocarcinoma status post left upper lobe lobectomy, underwent a left chest wall desmoid fibromatosis resection. Dual-antiplatelet therapy was held 3-5 days prior to procedure. On post-operative day 3, he developed acute dysphagia and was unable to tolerate oral secretions. Urgent CT scan of the chest showed a distended esophagus with debris, concerning for luminal obstruction. Esophagogastroduodenoscopy (EGD) revealed a large esophageal hematoma causing mid-to-distal luminal narrowing of the esophagus, with hematin seen throughout the stomach. The patient was started on omeprazole, a nasogastric tube was placed, and diet was gradually advanced. On the day of discharge (post-EGD day 3), a subsequent esophagogram showed resolution of obstruction with return of normal swallow function. He was discharged on single antiplatelet therapy with aspirin. At 8-month follow-up, he reported normal swallowing and repeat chest CT showed resolution of the hematoma.
Discussion: IEHs are rare entities that typically present with chest pain, dysphagia, and hematemesis and can mimic other cardiac or esophageal emergencies. They may occur spontaneously, or more commonly following esophageal instrumentation, trauma, or excessive retching and vomiting. Antiplatelet and anticoagulation therapy increases bleeding risk, predisposing patients to hematoma formation. Diagnosis is established through imaging (CT with IV contrast favored) followed by endoscopy. Esophagograms are useful to assess obstruction and swallowing function after the hematoma has been diagnosed. Most cases resolve with conservative treatment and without intervention. For this patient, esophageal stenting was deferred and conservative treatment was favored based on stable hemoglobin and successful passage of the endoscope past the hematoma. Hemoglobin remained stable following endoscopy. In this patient, the development of the IEH was likely multifactorial, including recent surgical stress and manipulation, underlying comorbidities, and recent use of dual-antiplatelet therapy.
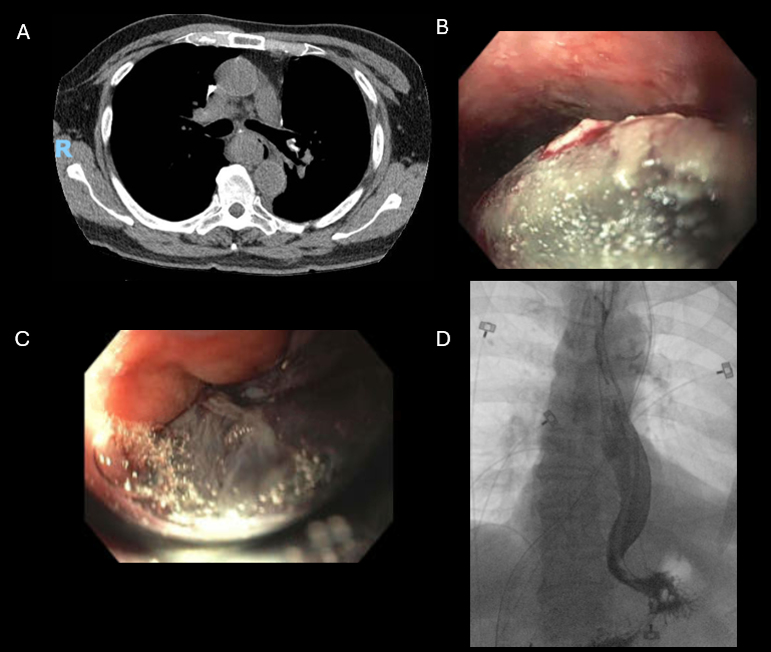
Figure: Figure 1 - A: Axial chest CT without contrast. B: Middle third of esophagus. C: Lower third of esophagus. D: Fluoroscopic imaging during esophagogastroduodenoscopy.
Disclosures:
Deirdre Reidy indicated no relevant financial relationships.
Lauren Callans indicated no relevant financial relationships.
Sean Rangwani indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Carl Crawford: Ferring – Advisor or Review Panel Member, Consultant, Grant/Research Support, Speakers Bureau. lumen – Grant/Research Support. nestle – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speakers Bureau. Phathom – Speakers Bureau. vedanta – Grant/Research Support.
David Wan: Medtronic – Data Monitoring Committee.
Deirdre Reidy, MD1, Lauren Callans, MD2, Sean Rangwani, MD, MBA3, Emily S. Smith, MD1, Carl V. Crawford, MD1, David Wan, MD4. P4973 - A Case of Postoperative Intramural Esophageal Hematoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
