Tuesday Poster Session
Category: Esophagus
P4966 - A Masked Case of Achalasia: Diagnostic Challenges of Eosinophilic Esophagitis Versus Achalasia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Harshitha Mogallapalli, MD
University of Wisconsin Hospitals and Clinics
Madison, WI
Presenting Author(s)
Harshitha Mogallapalli, MD, Luis Lomeli, MD, MPH
University of Wisconsin Hospitals and Clinics, Madison, WI
Introduction: Given the unclear causative relationship between eosinophilic esophagitis (EoE) and achalasia, there is no clear guideline for evaluation of patients that are presenting with overlapping symptoms such as dysphagia, food impactions and acid reflux. EoE can present with esophageal strictures and abnormal motility due to chronic inflammation leading to a delay in diagnosis of achalasia.
Case Description/
Methods: A 42 year old male with a history of eczema and allergies presents to clinic with complaints of acid reflux, dysphagia with every meal and intermittent food impaction requiring regurgitation. He independently increased his omeprazole to 40mg twice a day without symptomatic improvement.
With a history of other atopic conditions, the suspicion for eosinophilic esophagitis was high. His index upper esophagogastroduodenoscopy (EGD) demonstrated esophageal mucosal changes suggestive of eosinophilic esophagitis. Biopsies were positive for increased eosinophils (3-27 per hpf). Due to persistent symptoms, an esophagram was performed, which found a narrowed channel at the gastroesophageal junction with significant esophageal dysmotility. Due to the histologic findings of eosinophils, his treatment was escalated to include a Budesonide slurry. A repeat EGD was done 2 months later to assess response to therapy. Under careful examination, the esophagus appeared dilated, bubbly and fluid filled, and the lower esophageal sphincter appeared hypertonic, concerning for achalasia. During the procedure, an EndoFlip was performed and demonstrated a low distensibility (0.8-1.0 mm²/mmHg) and diameter (5-6 cm). An empiric dilation was performed without evidence of mucosal disruption. Evaluation with esophageal manometry demonstrated findings consistent with type II achalasia. Budesonide was discontinued as the underlying cause was thought to be achalasia.
Discussion: The conundrum with EoE and achalasia occurs because both primary diagnoses can lead to the other as a consequence. Esophageal stasis, seen in achalasia, can cause eosinophilia in the esophageal mucosa. Eosinophilia, seen in EoE, can release myoactive and neuroactive chemokines that cause an achalasia type abnormality. This case highlights the importance of considering an alternative diagnosis of achalasia in a setting where patients are not responding to standard treatments of EoE. Further evaluation with endoflip and esophageal manometry can aid in reducing the delay in diagnosis and treatment of achalasia.
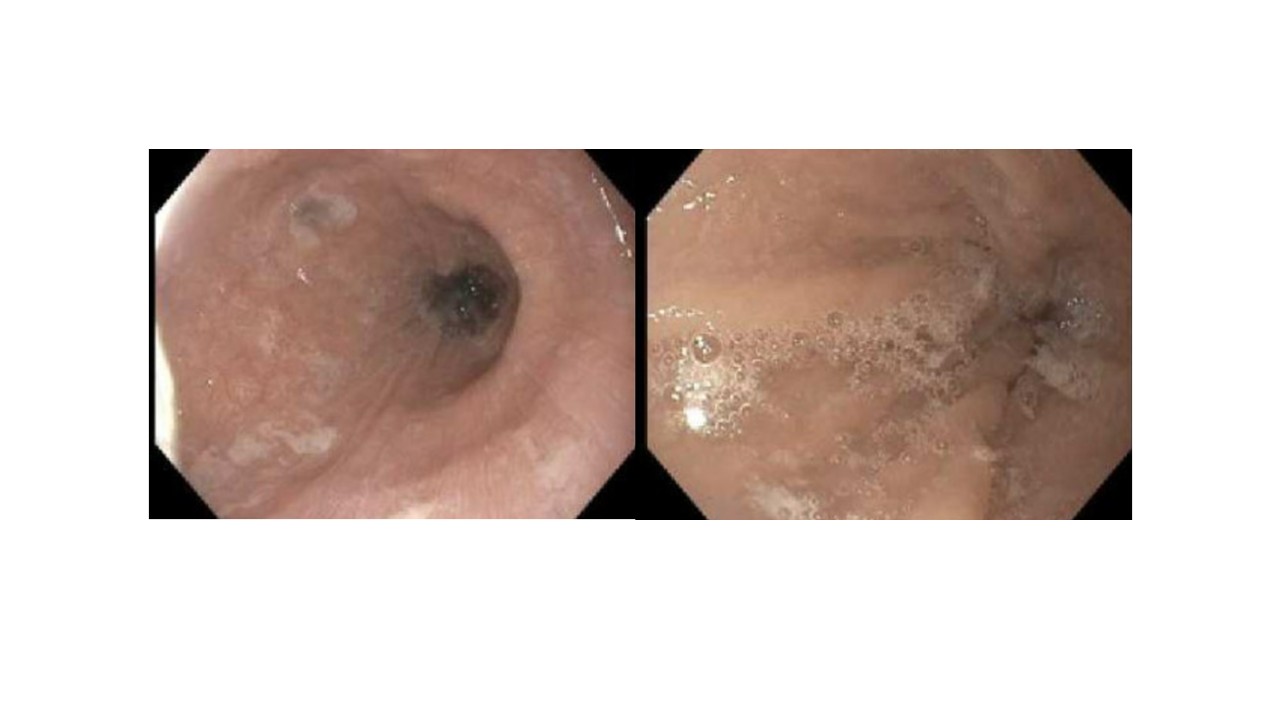
Figure: Figure 1: Endoscopy with evidence of esophageal mucosal changes suggestive of eosinophilic esophagitis
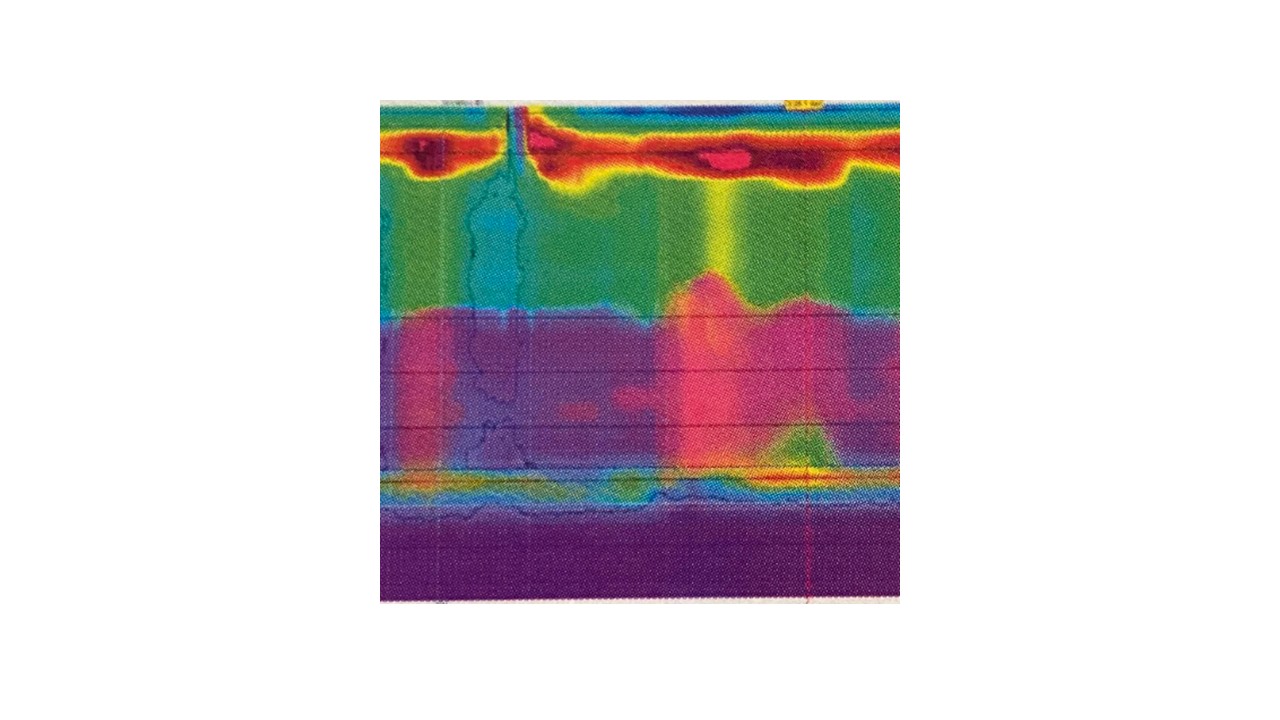
Figure: Figure 2: Esophageal manometry with evidence of type II achalasia
Disclosures:
Harshitha Mogallapalli indicated no relevant financial relationships.
Luis Lomeli: Sanofi – Advisor or Review Panel Member.
Harshitha Mogallapalli, MD, Luis Lomeli, MD, MPH. P4966 - A Masked Case of Achalasia: Diagnostic Challenges of Eosinophilic Esophagitis Versus Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Wisconsin Hospitals and Clinics, Madison, WI
Introduction: Given the unclear causative relationship between eosinophilic esophagitis (EoE) and achalasia, there is no clear guideline for evaluation of patients that are presenting with overlapping symptoms such as dysphagia, food impactions and acid reflux. EoE can present with esophageal strictures and abnormal motility due to chronic inflammation leading to a delay in diagnosis of achalasia.
Case Description/
Methods: A 42 year old male with a history of eczema and allergies presents to clinic with complaints of acid reflux, dysphagia with every meal and intermittent food impaction requiring regurgitation. He independently increased his omeprazole to 40mg twice a day without symptomatic improvement.
With a history of other atopic conditions, the suspicion for eosinophilic esophagitis was high. His index upper esophagogastroduodenoscopy (EGD) demonstrated esophageal mucosal changes suggestive of eosinophilic esophagitis. Biopsies were positive for increased eosinophils (3-27 per hpf). Due to persistent symptoms, an esophagram was performed, which found a narrowed channel at the gastroesophageal junction with significant esophageal dysmotility. Due to the histologic findings of eosinophils, his treatment was escalated to include a Budesonide slurry. A repeat EGD was done 2 months later to assess response to therapy. Under careful examination, the esophagus appeared dilated, bubbly and fluid filled, and the lower esophageal sphincter appeared hypertonic, concerning for achalasia. During the procedure, an EndoFlip was performed and demonstrated a low distensibility (0.8-1.0 mm²/mmHg) and diameter (5-6 cm). An empiric dilation was performed without evidence of mucosal disruption. Evaluation with esophageal manometry demonstrated findings consistent with type II achalasia. Budesonide was discontinued as the underlying cause was thought to be achalasia.
Discussion: The conundrum with EoE and achalasia occurs because both primary diagnoses can lead to the other as a consequence. Esophageal stasis, seen in achalasia, can cause eosinophilia in the esophageal mucosa. Eosinophilia, seen in EoE, can release myoactive and neuroactive chemokines that cause an achalasia type abnormality. This case highlights the importance of considering an alternative diagnosis of achalasia in a setting where patients are not responding to standard treatments of EoE. Further evaluation with endoflip and esophageal manometry can aid in reducing the delay in diagnosis and treatment of achalasia.
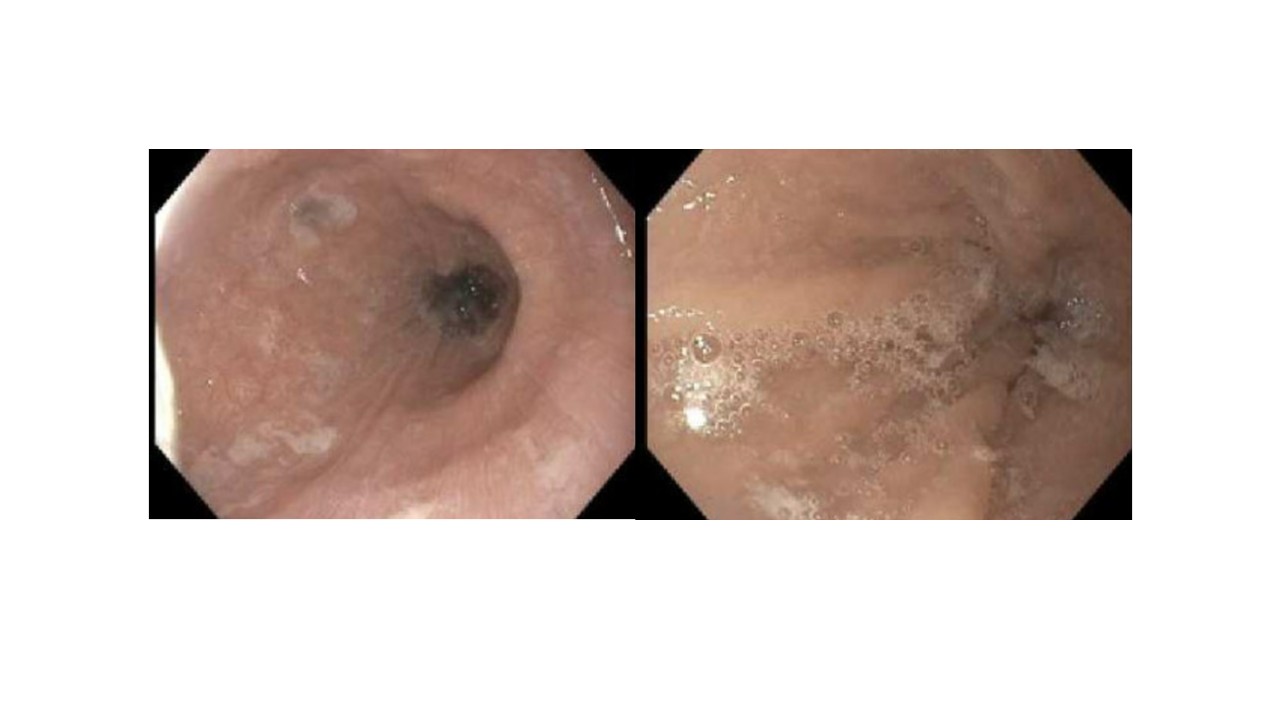
Figure: Figure 1: Endoscopy with evidence of esophageal mucosal changes suggestive of eosinophilic esophagitis
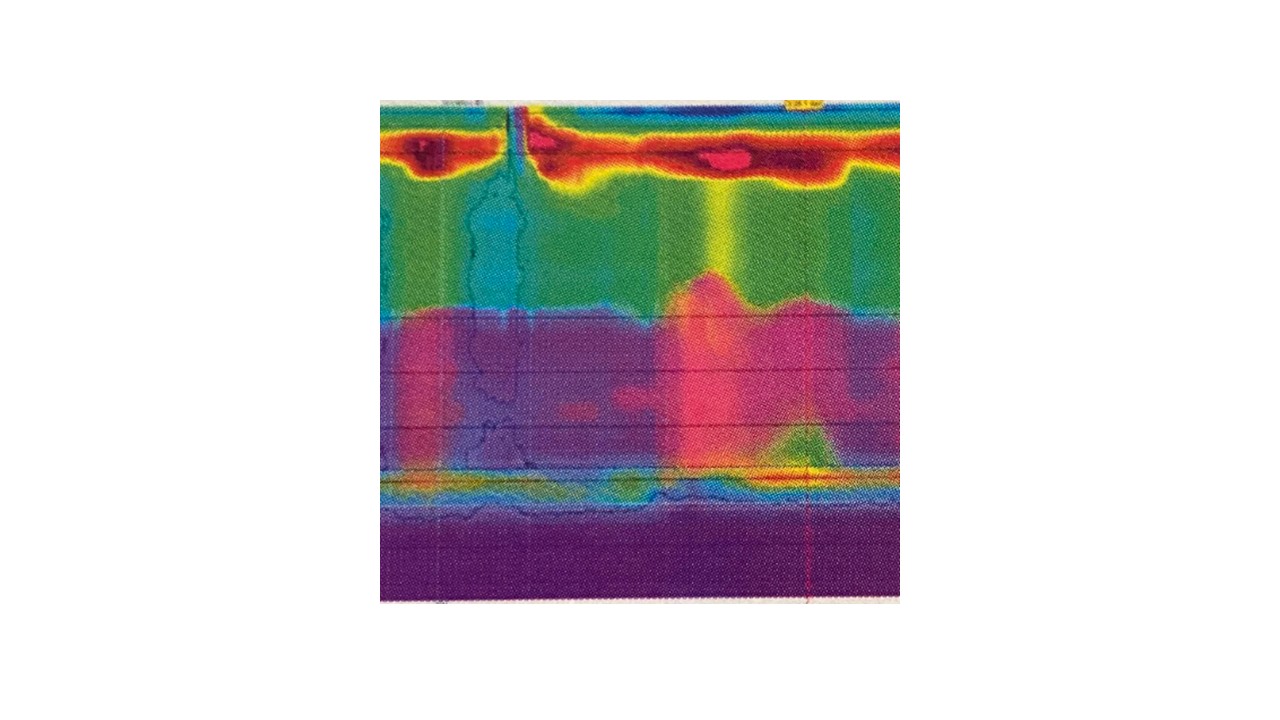
Figure: Figure 2: Esophageal manometry with evidence of type II achalasia
Disclosures:
Harshitha Mogallapalli indicated no relevant financial relationships.
Luis Lomeli: Sanofi – Advisor or Review Panel Member.
Harshitha Mogallapalli, MD, Luis Lomeli, MD, MPH. P4966 - A Masked Case of Achalasia: Diagnostic Challenges of Eosinophilic Esophagitis Versus Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
