Tuesday Poster Session
Category: Esophagus
P4944 - Epithelial Interleukin-8 in Eosinophilic Esophagitis: A Potential New Marker for Disease Activity and Lamina Propria Fibrosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sharef Al-Mulaabed, MD (he/him/his)
Center for Digestive Health and Nutrition, Orlando Health Arnold Palmer Hospital
Orlando, FL
Presenting Author(s)
Award: ACG Outstanding Research Award in the Esophagus Category (Trainee)
Award: ACG Presidential Poster Award
Sharef Al-Mulaabed, MD1, Yamen Smadi, MD1, Mary Schreck, PhD2, Noah Stoeckel, MS3, Nidhi Kapoor, PhD3
1Center for Digestive Health and Nutrition, Orlando Health Arnold Palmer Hospital, Orlando, FL; 2Orlando Health Medical Group Pediatrics Specialty Practice; Orlando Health, Orlando, FL; 3Specialty Diagnostic Clinical and Translational Research Lab, Arnold Palmer Hospital for Children, Orlando, FL
Introduction: The pathogenesis of eosinophilic esophagitis (EoE) is predominantly driven by T helper 2 cells cytokines such as IL-4, IL-5, and IL-13, however, IL-8 may play an important role in its inflammation and fibrogenesis. We aim to evaluate IL-8 levels in EoE patients and assess its correlation with histology and fibrosis.
Methods: We conducted a longitudinal analysis of EoE patients who underwent endoscopy (Jan 2021 to May 2025) at EoE center with previously collected esophageal brushing samples available to measure IL-8 levels (sample extracted using cell lysis buffer and the homogenate was centrifuged, then IL-8 was measured using ELISA). EoE diagnosis and activity were evaluated per published guidelines, with controls being those with normal endoscopy and histology.
Results: We included a total of 87 subjects: 54 confirmed EoE (mean ± SD age of 10.2 ±5 years; 30 [56%] male), and 33 controls (mean ± SD age of 9.9±5.2 years; 21 (64%) male). Out of 54 EoE patients, 38 were active with no treatment, with significantly higher IL-8 levels (median 814 pg/mL) compared to controls (median 30 pg/mL), p< 0.001, figure 1-A. There was a significant reduction of IL-8 levels upon repeat endoscopy in EoE patients with successful treatment (41/54, 76%), p< 0.001, figure 1-B. In contrast, EoE patients with failed treatment (13/54, 24%) showed no significant change in IL-8. IL-8 showed a significant positive correlation with peak eosinophilic count (PEC), figure 2-A.
ROC analysis for IL-8 to differentiate active EoE patients from controls revealed an optimal IL-8 threshold of 203 pg/ml (85% sensitivity and 100% specificity). Using IL-8 to distinguish active EoE from remission, the optimal threshold is 159 pg/ml, with 91% sensitivity and 78% specificity, figure 2-B.
IL-8 was significantly elevated in EoE patients with evidence of lamina propria fibrosis [median (IQR) of 845 (256-1310) pg/ml], compared to those with no fibrosis [median (IQR) of 207 (57-760) pg/ml], p=0.002. IL-8 threshold of 784 pg/mL yielded 86% sensitivity and of 58% specificity for predicting fibrosis.
Discussion: Our study demonstrates that epithelial IL-8 is significantly elevated in EoE patients and strongly correlates with PEC, with excellent accuracy in distinguishing active EoE from remission. Additionally, epithelial IL-8 may serve as a predictive marker of lamina propria fibrosis. These findings support the potential role of IL-8 as a new biomarker of disease activity and fibrosis with possible future utility as a therapeutic target.
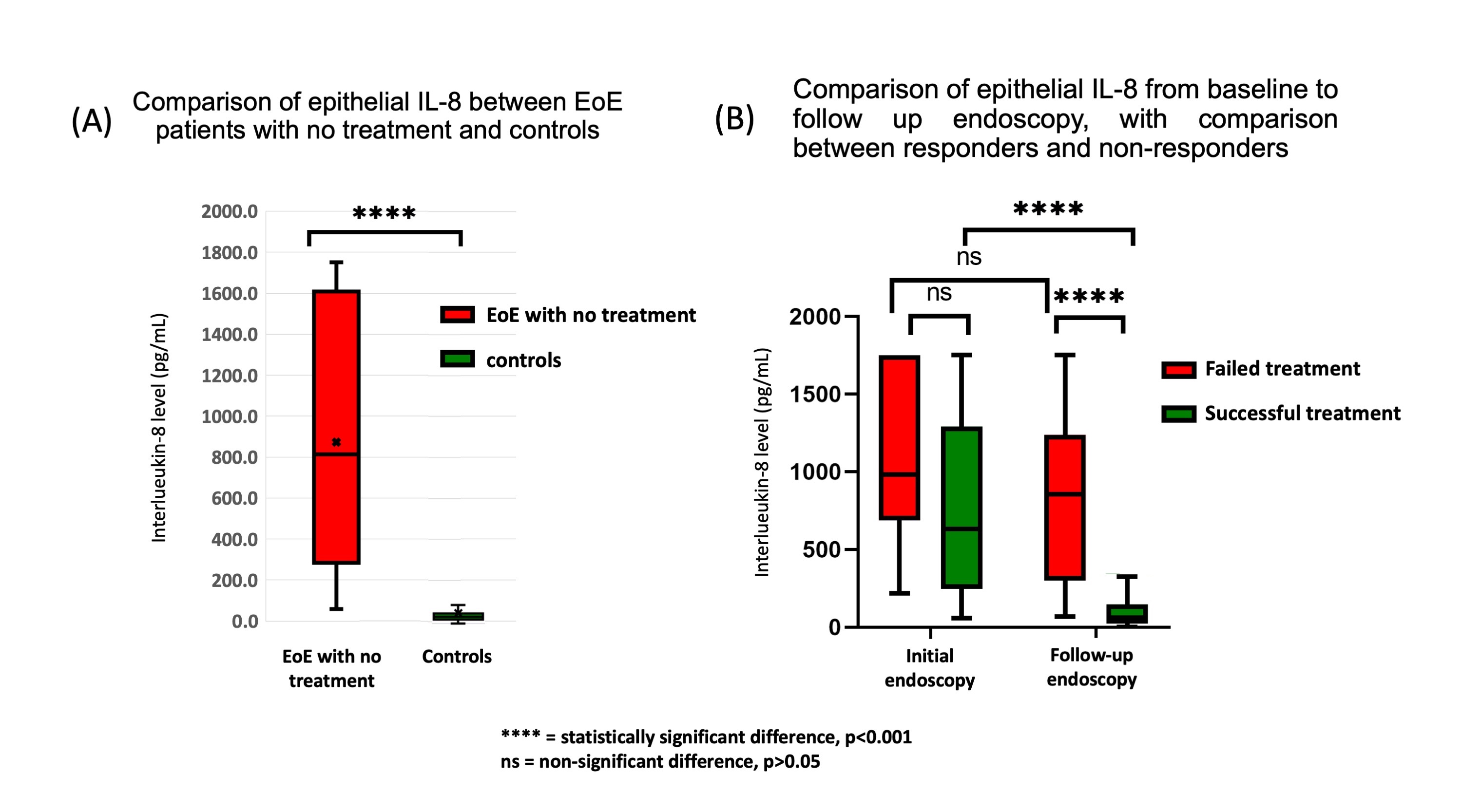
Figure: Figure 1: Comparison of epithelial IL-8 (A) between EoE patients with no treatment and controls, (B) from baseline to follow up endoscopy
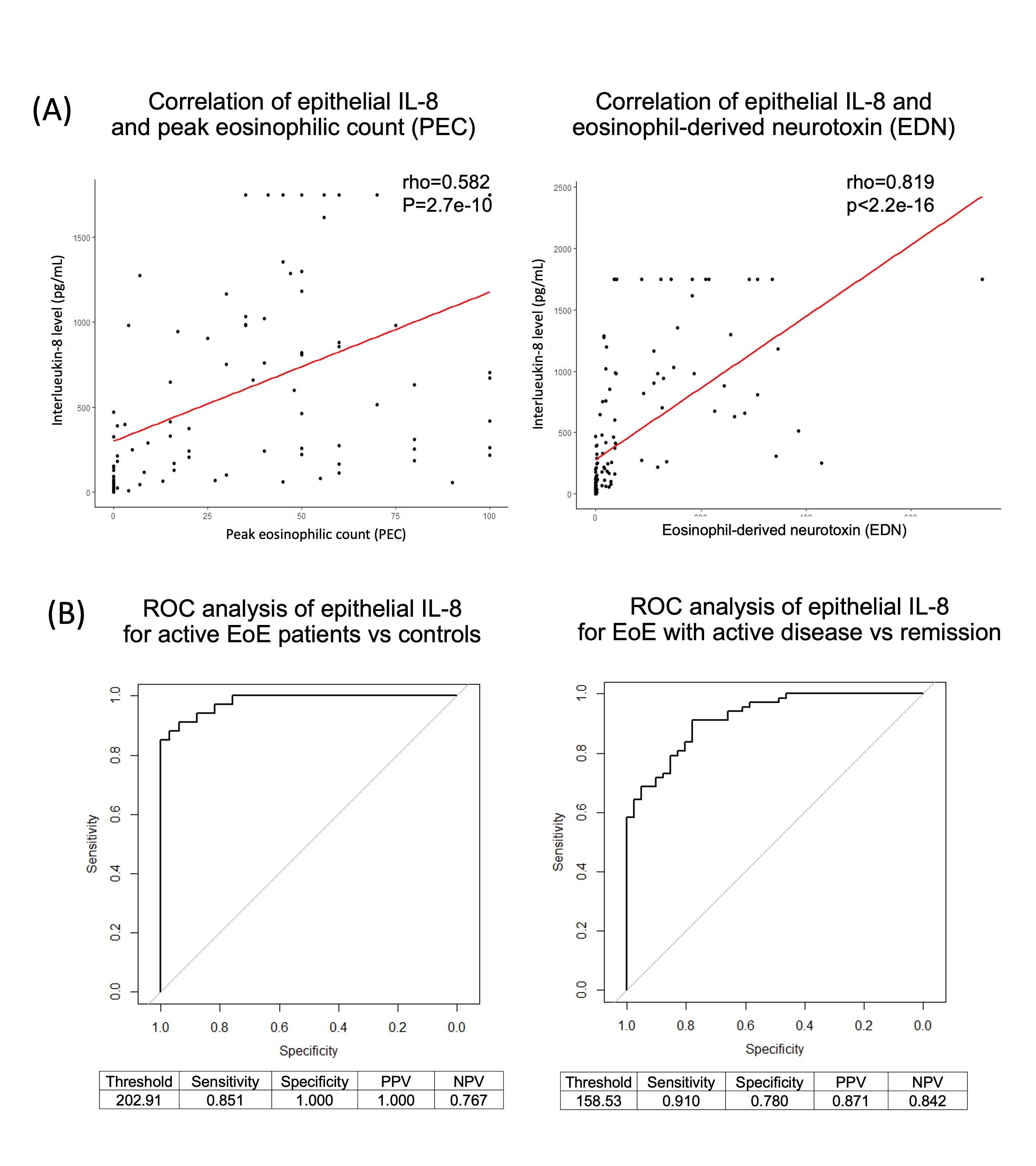
Figure: Figure 2: (A) Correlation of epithelial IL-8 with peak eosinophilic count and eosinophil-derived neurotoxin.
(B) ROC analysis of epithelial IL-8 for active EoE patients vs controls, and EoE with active disease vs remission
Disclosures:
Sharef Al-Mulaabed indicated no relevant financial relationships.
Yamen Smadi indicated no relevant financial relationships.
Mary Schreck indicated no relevant financial relationships.
Noah Stoeckel indicated no relevant financial relationships.
Nidhi Kapoor indicated no relevant financial relationships.
Sharef Al-Mulaabed, MD1, Yamen Smadi, MD1, Mary Schreck, PhD2, Noah Stoeckel, MS3, Nidhi Kapoor, PhD3. P4944 - Epithelial Interleukin-8 in Eosinophilic Esophagitis: A Potential New Marker for Disease Activity and Lamina Propria Fibrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Award: ACG Presidential Poster Award
Sharef Al-Mulaabed, MD1, Yamen Smadi, MD1, Mary Schreck, PhD2, Noah Stoeckel, MS3, Nidhi Kapoor, PhD3
1Center for Digestive Health and Nutrition, Orlando Health Arnold Palmer Hospital, Orlando, FL; 2Orlando Health Medical Group Pediatrics Specialty Practice; Orlando Health, Orlando, FL; 3Specialty Diagnostic Clinical and Translational Research Lab, Arnold Palmer Hospital for Children, Orlando, FL
Introduction: The pathogenesis of eosinophilic esophagitis (EoE) is predominantly driven by T helper 2 cells cytokines such as IL-4, IL-5, and IL-13, however, IL-8 may play an important role in its inflammation and fibrogenesis. We aim to evaluate IL-8 levels in EoE patients and assess its correlation with histology and fibrosis.
Methods: We conducted a longitudinal analysis of EoE patients who underwent endoscopy (Jan 2021 to May 2025) at EoE center with previously collected esophageal brushing samples available to measure IL-8 levels (sample extracted using cell lysis buffer and the homogenate was centrifuged, then IL-8 was measured using ELISA). EoE diagnosis and activity were evaluated per published guidelines, with controls being those with normal endoscopy and histology.
Results: We included a total of 87 subjects: 54 confirmed EoE (mean ± SD age of 10.2 ±5 years; 30 [56%] male), and 33 controls (mean ± SD age of 9.9±5.2 years; 21 (64%) male). Out of 54 EoE patients, 38 were active with no treatment, with significantly higher IL-8 levels (median 814 pg/mL) compared to controls (median 30 pg/mL), p< 0.001, figure 1-A. There was a significant reduction of IL-8 levels upon repeat endoscopy in EoE patients with successful treatment (41/54, 76%), p< 0.001, figure 1-B. In contrast, EoE patients with failed treatment (13/54, 24%) showed no significant change in IL-8. IL-8 showed a significant positive correlation with peak eosinophilic count (PEC), figure 2-A.
ROC analysis for IL-8 to differentiate active EoE patients from controls revealed an optimal IL-8 threshold of 203 pg/ml (85% sensitivity and 100% specificity). Using IL-8 to distinguish active EoE from remission, the optimal threshold is 159 pg/ml, with 91% sensitivity and 78% specificity, figure 2-B.
IL-8 was significantly elevated in EoE patients with evidence of lamina propria fibrosis [median (IQR) of 845 (256-1310) pg/ml], compared to those with no fibrosis [median (IQR) of 207 (57-760) pg/ml], p=0.002. IL-8 threshold of 784 pg/mL yielded 86% sensitivity and of 58% specificity for predicting fibrosis.
Discussion: Our study demonstrates that epithelial IL-8 is significantly elevated in EoE patients and strongly correlates with PEC, with excellent accuracy in distinguishing active EoE from remission. Additionally, epithelial IL-8 may serve as a predictive marker of lamina propria fibrosis. These findings support the potential role of IL-8 as a new biomarker of disease activity and fibrosis with possible future utility as a therapeutic target.
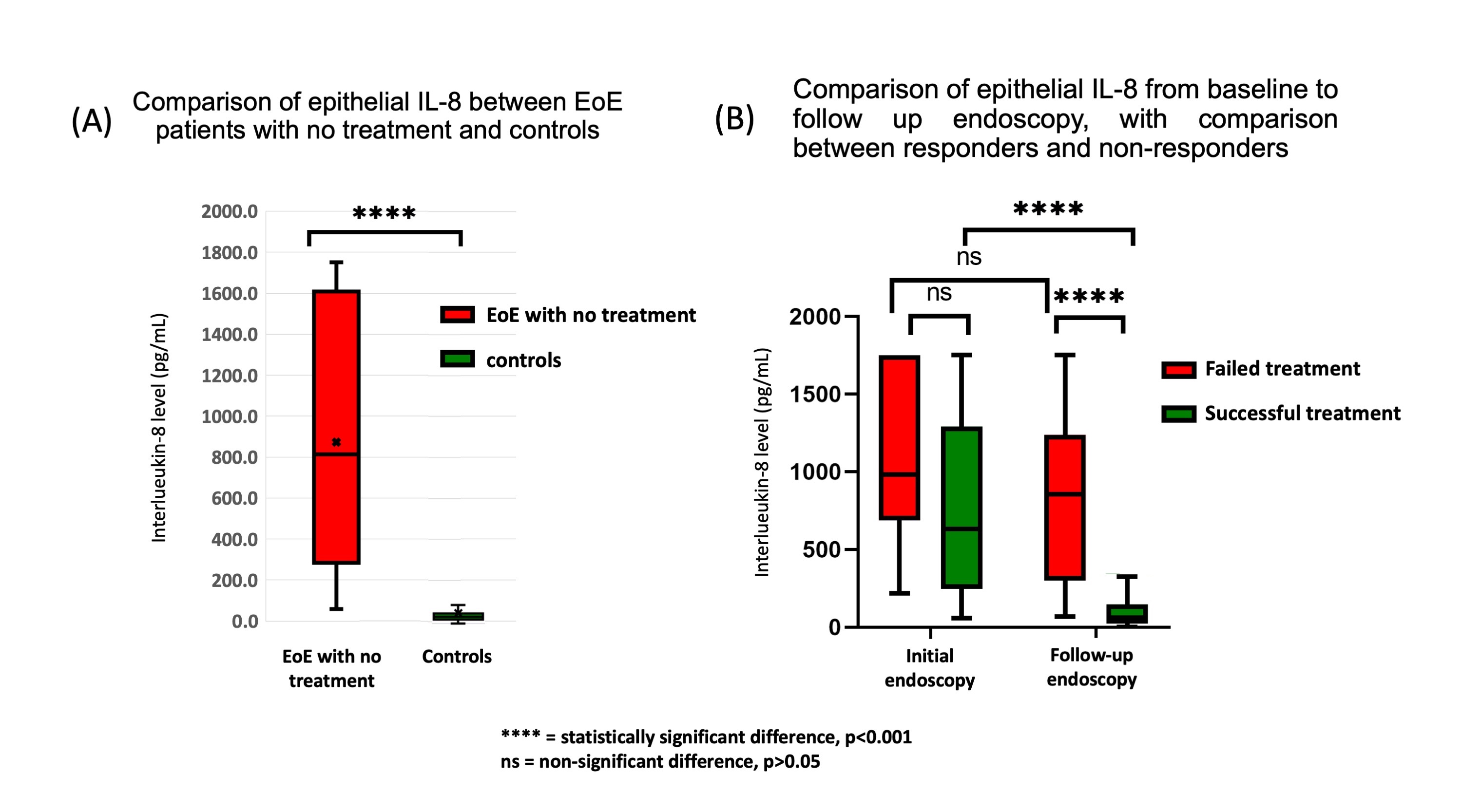
Figure: Figure 1: Comparison of epithelial IL-8 (A) between EoE patients with no treatment and controls, (B) from baseline to follow up endoscopy
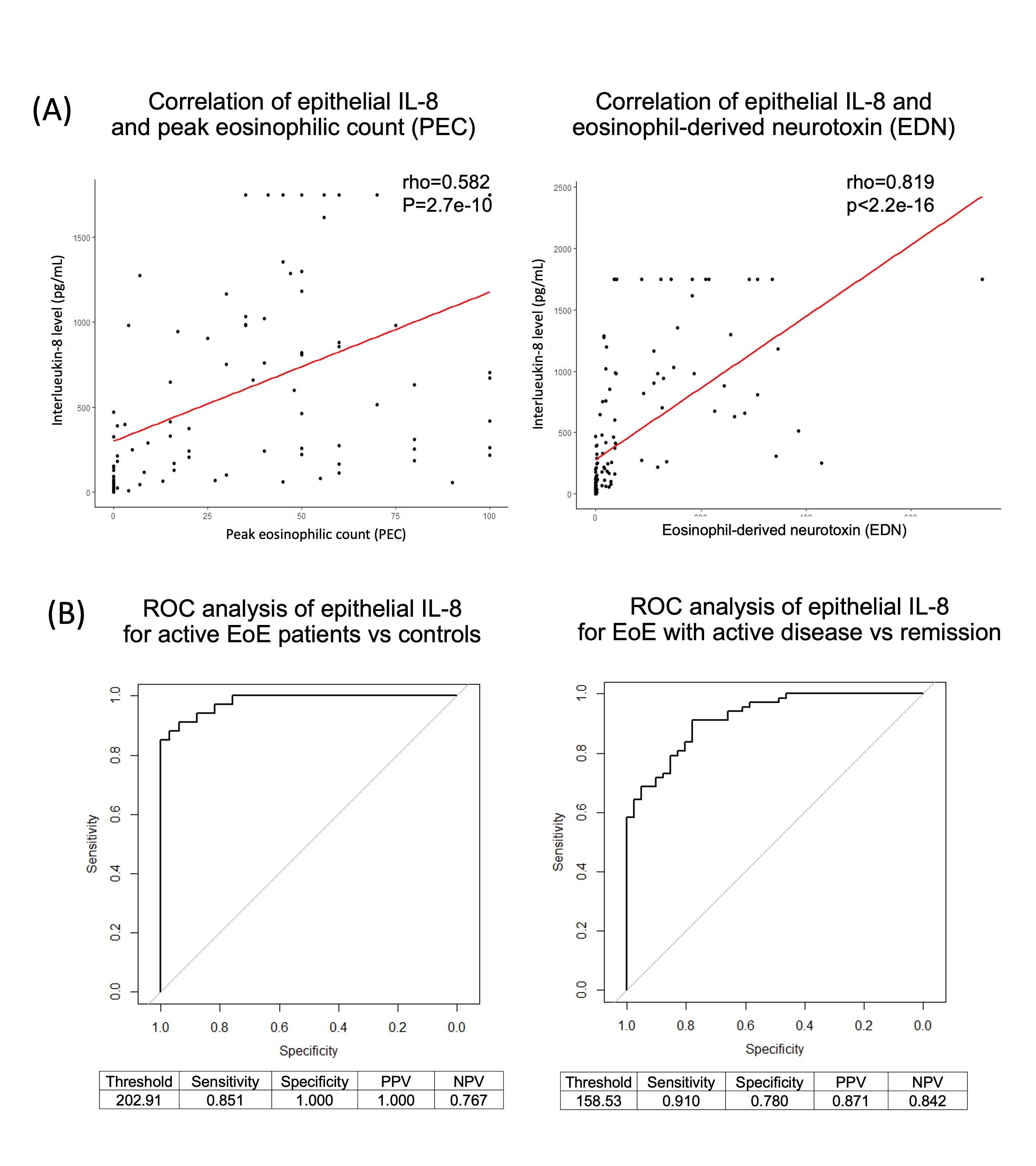
Figure: Figure 2: (A) Correlation of epithelial IL-8 with peak eosinophilic count and eosinophil-derived neurotoxin.
(B) ROC analysis of epithelial IL-8 for active EoE patients vs controls, and EoE with active disease vs remission
Disclosures:
Sharef Al-Mulaabed indicated no relevant financial relationships.
Yamen Smadi indicated no relevant financial relationships.
Mary Schreck indicated no relevant financial relationships.
Noah Stoeckel indicated no relevant financial relationships.
Nidhi Kapoor indicated no relevant financial relationships.
Sharef Al-Mulaabed, MD1, Yamen Smadi, MD1, Mary Schreck, PhD2, Noah Stoeckel, MS3, Nidhi Kapoor, PhD3. P4944 - Epithelial Interleukin-8 in Eosinophilic Esophagitis: A Potential New Marker for Disease Activity and Lamina Propria Fibrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


