Tuesday Poster Session
Category: Esophagus
P4927 - Efficacy and Safety of Argon Plasma Coagulation vs Radiofrequency Ablation for Barrett's Esophagus: A Systematic Review
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FP
Fortunato S. Principe-Meneses, MD (he/him/his)
Universidad Peruana de Ciencias Aplicadas (UPC)
Lima, Lima, Peru
Presenting Author(s)
Fortunato S. Principe-Meneses, MD1, Luis G.. Azanedo-Garcia, MD2, Adrian Riva, MD3, Andrea Roman-Pimentel, MD4, Karla L. Hernandez Randich, MD4, Andres Chaponan-Lavalle, 4, Eleazar E.. Montalvan-Sanchez, MD5
1Universidad Peruana de Ciencias Aplicadas (UPC), Lima, Lima, Peru; 2Universidad Peruana de Ciencias Aplicadas, Lima, Perú., Orlando, FL; 3Department of Surgery, Northwest Hospital, Randallstown, MD, USA, Lima, Lima, Peru; 4Universidad Peruana de Ciencias Aplicadas, Lima, Lima, Peru; 5Yale University School of Medicine, New Haven, CT
Introduction: Barrett’s Esophagus (BE) is a premalignant condition requiring effective endoscopic eradication therapies (EET) to prevent progression to esophageal adenocarcinoma. Among available treatments, Argon Plasma Coagulation (APC), its newer modality Hybrid Argon Plasma Coagulation (H-APC) and Radiofrequency Ablation (RFA) have gained prominence. However, data comparing their efficacy and safety remains limited. Our aim was to compare the efficacy and safety of APC or its variant H-APC vs RFA in the treatment of BE.
Methods: A systematic search was conducted across six major databases (MEDLINE, Embase, Scopus, Web of Science, CINAHL, and Cochrane Library) for studies published between 2000 and June 2024. We included randomized controlled trials (RCTs) and cohort studies comparing APC or its modality H-APC vs RFA in BE management. Primary outcomes included complete eradication of intestinal metaplasia and dysplasia, as well as adverse event rates (strictures, bleeding, pain, and perforation).
Results: Three studies met inclusion criteria: two RCTs and one retrospective cohort study (Table 1).
Comparing APC vs RFA: Peerally et al. found that the 12-month clearance rate of Barrett’s esophagus was 55.8% for RFA and 48.3% for APC. Stricture rates were slightly higher in the RFA group, with 8.3% compared to 8.1% in the APC group. Additionally, post-procedural chest pain was less frequent in the APC group, with 12% versus 25% in the RFA group. No perforations were reported in APC arm.
Comparing H-APC vs RFA: Knabe et al, reported that short-term eradication rates were 79.1% for H-APC and 64.5% for RFA (p=0.129), while long-term eradication rates were 82.9% and 74.2%, respectively (p=0.07). H-APC demonstrated a superior safety profile, with significantly lower rates of strictures (3.7% vs. 14.9%), reduced post-procedural pain, and fewer adverse events overall (Table 2). Linn et al reported presence of BE in 26% and 11% of patients after RFA and H-APC respectively at short term follow up. Most patients in the RFA group developed stricture in 15% of patients and pain in 4% of patients, meanwhile none of the patients developed adverse events in the H-APC group.
Discussion: APC and its modality appears to be as effective as RFA for BE treatment while offering a more favorable safety profile. However, given the limited number of comparative studies, further high-quality clinical trials are necessary to validate these findings and optimize treatment strategies.
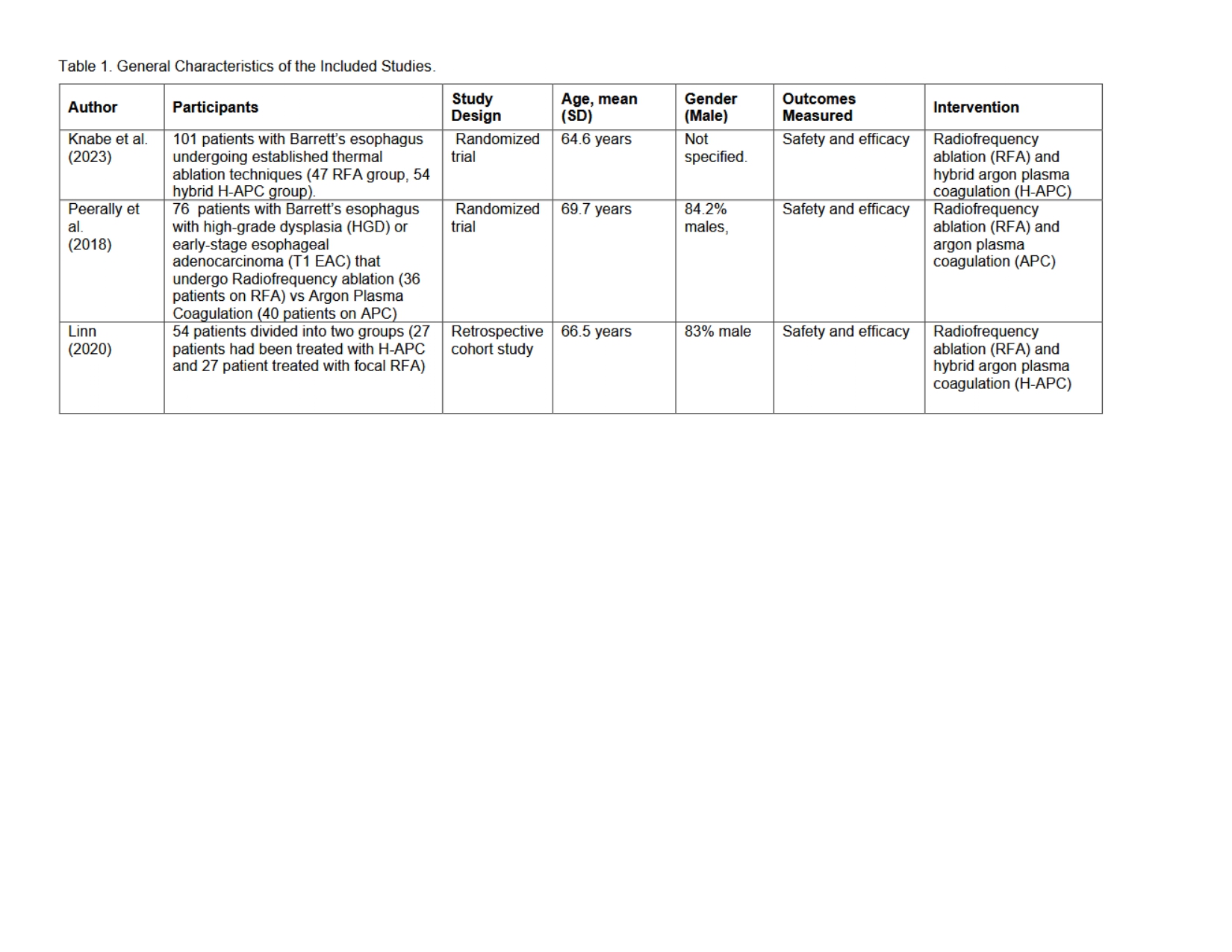
Figure: General Characteristics of Included Studies
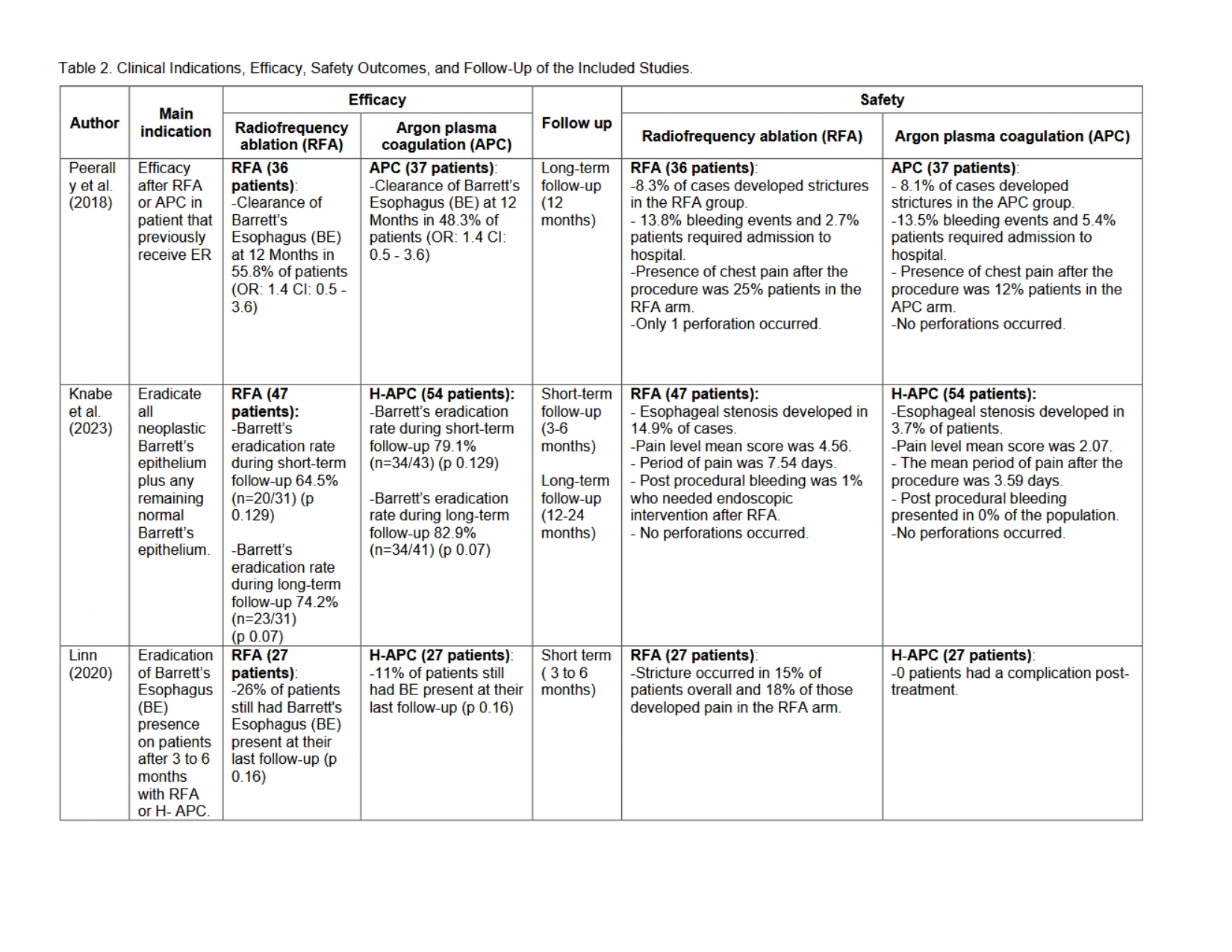
Figure: Efficacy, Safety and Follow-up outcomes of Included Studies
Disclosures:
Fortunato S. Principe-Meneses indicated no relevant financial relationships.
Luis Azanedo-Garcia indicated no relevant financial relationships.
Adrian Riva indicated no relevant financial relationships.
Andrea Roman-Pimentel indicated no relevant financial relationships.
Karla Hernandez Randich indicated no relevant financial relationships.
Andres Chaponan-Lavalle indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Fortunato S. Principe-Meneses, MD1, Luis G.. Azanedo-Garcia, MD2, Adrian Riva, MD3, Andrea Roman-Pimentel, MD4, Karla L. Hernandez Randich, MD4, Andres Chaponan-Lavalle, 4, Eleazar E.. Montalvan-Sanchez, MD5. P4927 - Efficacy and Safety of Argon Plasma Coagulation vs Radiofrequency Ablation for Barrett's Esophagus: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Universidad Peruana de Ciencias Aplicadas (UPC), Lima, Lima, Peru; 2Universidad Peruana de Ciencias Aplicadas, Lima, Perú., Orlando, FL; 3Department of Surgery, Northwest Hospital, Randallstown, MD, USA, Lima, Lima, Peru; 4Universidad Peruana de Ciencias Aplicadas, Lima, Lima, Peru; 5Yale University School of Medicine, New Haven, CT
Introduction: Barrett’s Esophagus (BE) is a premalignant condition requiring effective endoscopic eradication therapies (EET) to prevent progression to esophageal adenocarcinoma. Among available treatments, Argon Plasma Coagulation (APC), its newer modality Hybrid Argon Plasma Coagulation (H-APC) and Radiofrequency Ablation (RFA) have gained prominence. However, data comparing their efficacy and safety remains limited. Our aim was to compare the efficacy and safety of APC or its variant H-APC vs RFA in the treatment of BE.
Methods: A systematic search was conducted across six major databases (MEDLINE, Embase, Scopus, Web of Science, CINAHL, and Cochrane Library) for studies published between 2000 and June 2024. We included randomized controlled trials (RCTs) and cohort studies comparing APC or its modality H-APC vs RFA in BE management. Primary outcomes included complete eradication of intestinal metaplasia and dysplasia, as well as adverse event rates (strictures, bleeding, pain, and perforation).
Results: Three studies met inclusion criteria: two RCTs and one retrospective cohort study (Table 1).
Comparing APC vs RFA: Peerally et al. found that the 12-month clearance rate of Barrett’s esophagus was 55.8% for RFA and 48.3% for APC. Stricture rates were slightly higher in the RFA group, with 8.3% compared to 8.1% in the APC group. Additionally, post-procedural chest pain was less frequent in the APC group, with 12% versus 25% in the RFA group. No perforations were reported in APC arm.
Comparing H-APC vs RFA: Knabe et al, reported that short-term eradication rates were 79.1% for H-APC and 64.5% for RFA (p=0.129), while long-term eradication rates were 82.9% and 74.2%, respectively (p=0.07). H-APC demonstrated a superior safety profile, with significantly lower rates of strictures (3.7% vs. 14.9%), reduced post-procedural pain, and fewer adverse events overall (Table 2). Linn et al reported presence of BE in 26% and 11% of patients after RFA and H-APC respectively at short term follow up. Most patients in the RFA group developed stricture in 15% of patients and pain in 4% of patients, meanwhile none of the patients developed adverse events in the H-APC group.
Discussion: APC and its modality appears to be as effective as RFA for BE treatment while offering a more favorable safety profile. However, given the limited number of comparative studies, further high-quality clinical trials are necessary to validate these findings and optimize treatment strategies.
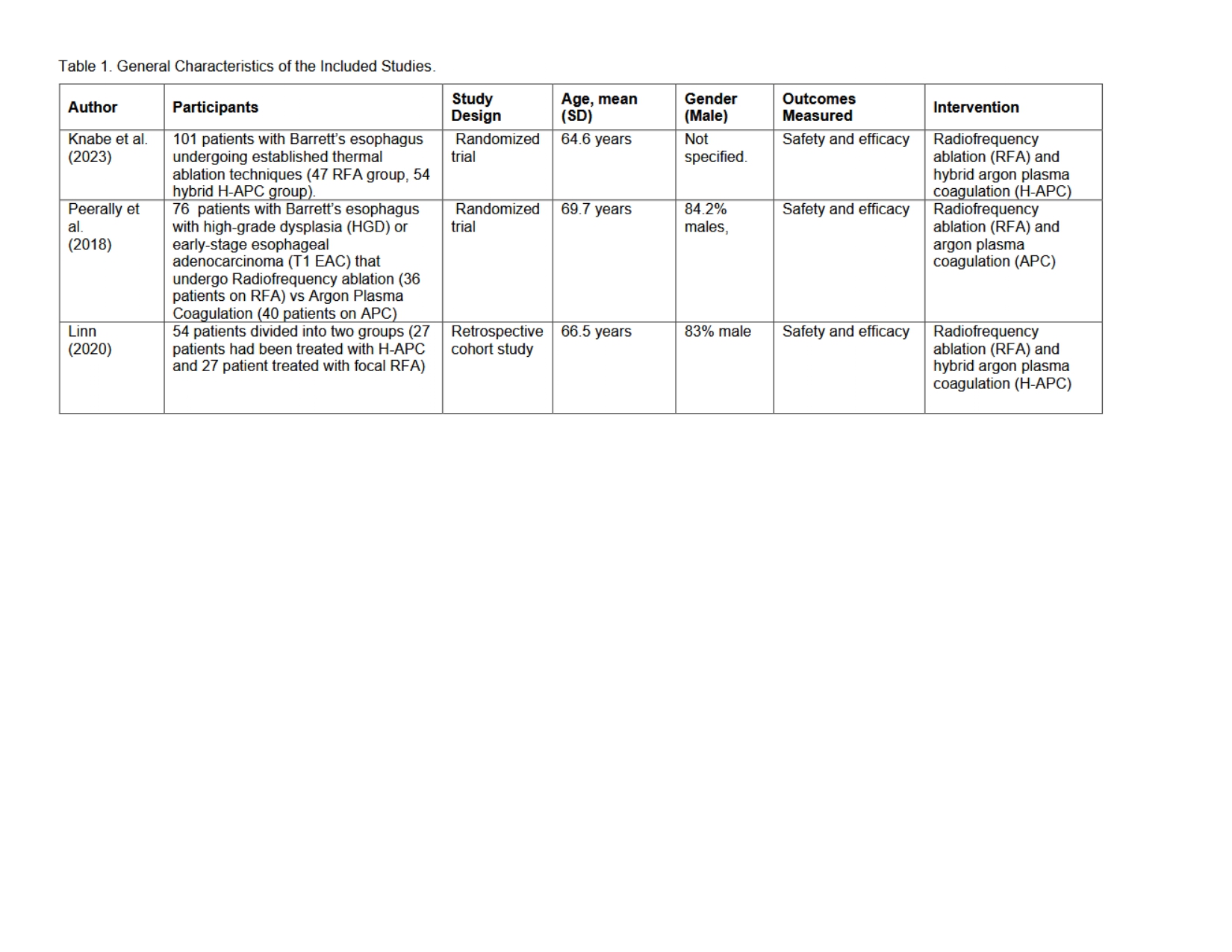
Figure: General Characteristics of Included Studies
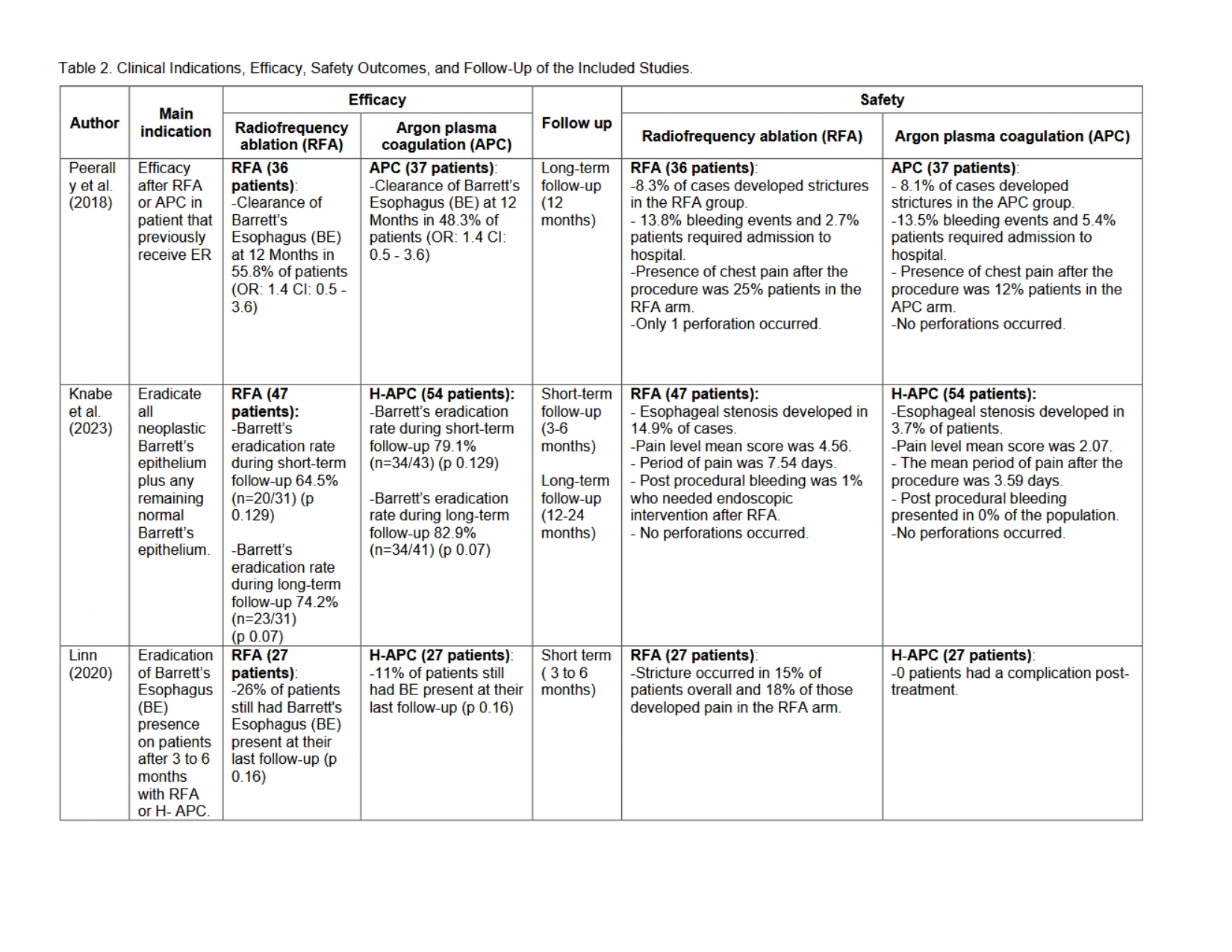
Figure: Efficacy, Safety and Follow-up outcomes of Included Studies
Disclosures:
Fortunato S. Principe-Meneses indicated no relevant financial relationships.
Luis Azanedo-Garcia indicated no relevant financial relationships.
Adrian Riva indicated no relevant financial relationships.
Andrea Roman-Pimentel indicated no relevant financial relationships.
Karla Hernandez Randich indicated no relevant financial relationships.
Andres Chaponan-Lavalle indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Fortunato S. Principe-Meneses, MD1, Luis G.. Azanedo-Garcia, MD2, Adrian Riva, MD3, Andrea Roman-Pimentel, MD4, Karla L. Hernandez Randich, MD4, Andres Chaponan-Lavalle, 4, Eleazar E.. Montalvan-Sanchez, MD5. P4927 - Efficacy and Safety of Argon Plasma Coagulation vs Radiofrequency Ablation for Barrett's Esophagus: A Systematic Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
