Tuesday Poster Session
Category: Esophagus
P4926 - Clinical Predictors of Breakthrough Acid Reflux Despite Proton Pump Inhibitor Use During 24-hour pH-Impedance Testing
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ankit M. Shah, MD (he/him/his)
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ankit M.. Shah, MD, Daniela Jodorkovsky, MD
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The Lyon Consensus establishes criteria for conclusive Gastroesophageal Reflux Disease (GERD) using pH-impedance testing. Performing testing while off proton pump inhibitor (PPI) therapy is recommended in unproven GERD. However, barriers for this recommendation include the inability of patients to stop therapy and unawareness of the limitations of on-PPI testing by providers. The aim of our study was to determine pre-testing clinical factors that may predict breakthrough positive results on pH-impedance despite testing on PPI.
Methods: A retrospective chart review was conducted of 326 patients with 24-hour pH-impedance testing on PPI at a single tertiary care academic center. Exclusion criteria included known esophagitis, prior fundoplication, and incomplete charts. Sociodemographic variables, symptom presentation, clinical variables, and testing data were manually extracted via chart review. Symptoms of heartburn, regurgitation, and chest pain were considered typical. Other symptoms were considered atypical. Presence and size of hiatal hernia (HH) was assessed by prior endoscopy. A breakthrough positive result was defined as Acid Exposure Time >4%. Univariate and focused multivariate logistic regression analyses were performed.
Results: 204 patients were included. The median age was 57 years and median BMI was 27. In our cohort, 46% were non-Hispanic (NH) White, 13% where NH Black, 13% were Hispanic, 7% were Asian, and 21% were Other. 37% of patients had a history of tobacco use and 51% had a history of alcohol use. A history of any size hiatal hernia was noted in 23% of patients and 6% had one larger than 2 cm. 39% of patients were tested on once daily PPI. On multivariable analysis, once daily PPI (OR: 3.26, 95% CI: 1.50 - 7.06) and a history of hiatal hernia (OR: 3.33, 95% CI: 1.44 - 7.68) were predictors of having breakthrough acid reflux on testing. Conversely, patients with combined typical and atypical symptoms were less likely to have a positive test (OR: 0.21, 95% CI: 0.08 - 0.59).
Discussion: While off-PPI testing is recommended for patients with unproven GERD, some patients or providers may be hesitant to stop therapy prior to diagnostic testing which may lead to diagnostic uncertainty. This study suggests that if patients do not have atypical symptoms, have a hiatal hernia, or only on once daily PPI, on-PPI testing may still yield breakthrough positive results. Without the presence of these clinical predictors, barriers to off PPI testing should be investigated and addressed.
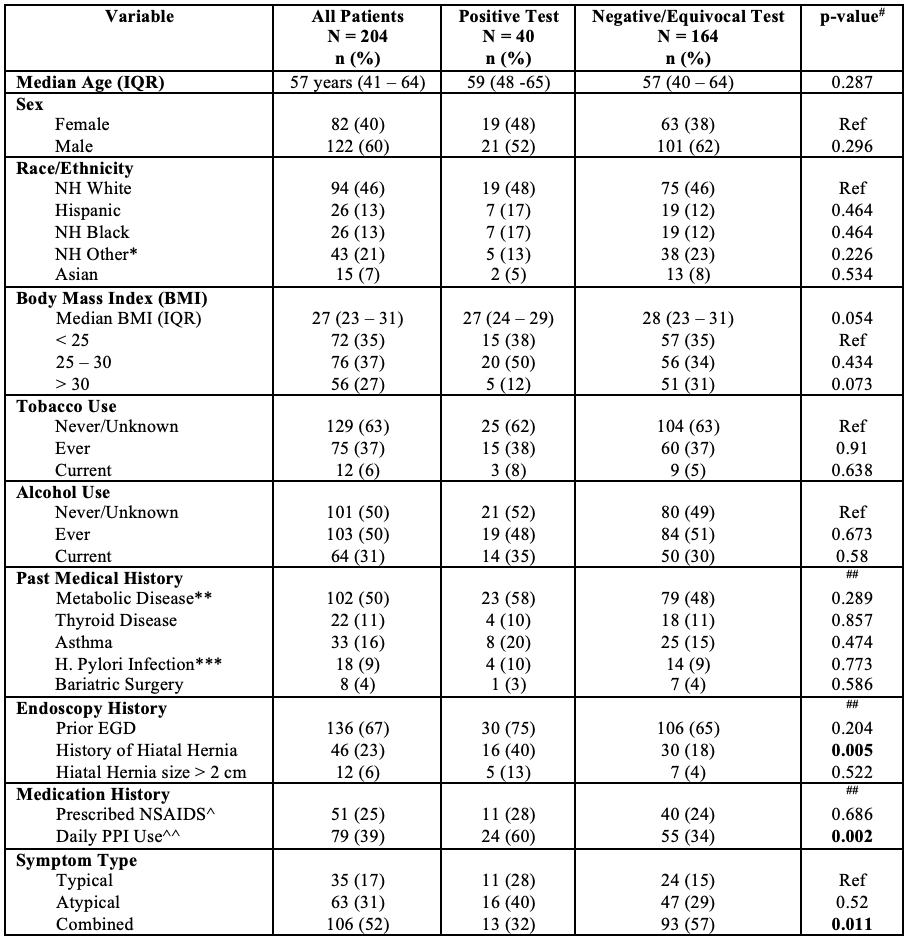
Figure: Table 1. Cohort Characteristics. NH = non-Hispanic, EGD = esophagogastroduodenoscopy, PPI = proton pump inhibitor, H. Pylori = Helicobacter Pylori, Ref = reference group for odds ratio calculation on univariate analysis. *NH Other includes patients with “Unknown” ethnicity. **Metabolic Disease includes having any of the following: Type 2 Diabetes Mellitus, Hypertension, Hyperlipidemia, or Statin use. ***Includes any documented prior infection, regardless of treatment status. ^Includes daily low-dose aspirin. ^^ Non-daily PPI group includes 1 patient prescribed PPI TID and the rest were prescribed PPI BID. #P-values obtained from univariate logistic regression. ##Reference value was patients without the presence of the variable.
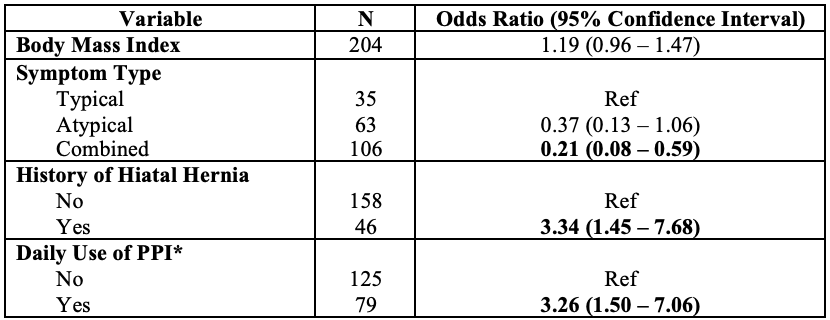
Figure: Table 2. Multivariable Logistic Regression. PPI = proton pump inhibitor. *Non-daily PPI group includes 1 patient prescribed PPI TID and the rest were prescribed PPI BID.
Disclosures:
Ankit Shah indicated no relevant financial relationships.
Daniela Jodorkovsky indicated no relevant financial relationships.
Ankit M.. Shah, MD, Daniela Jodorkovsky, MD. P4926 - Clinical Predictors of Breakthrough Acid Reflux Despite Proton Pump Inhibitor Use During 24-hour pH-Impedance Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The Lyon Consensus establishes criteria for conclusive Gastroesophageal Reflux Disease (GERD) using pH-impedance testing. Performing testing while off proton pump inhibitor (PPI) therapy is recommended in unproven GERD. However, barriers for this recommendation include the inability of patients to stop therapy and unawareness of the limitations of on-PPI testing by providers. The aim of our study was to determine pre-testing clinical factors that may predict breakthrough positive results on pH-impedance despite testing on PPI.
Methods: A retrospective chart review was conducted of 326 patients with 24-hour pH-impedance testing on PPI at a single tertiary care academic center. Exclusion criteria included known esophagitis, prior fundoplication, and incomplete charts. Sociodemographic variables, symptom presentation, clinical variables, and testing data were manually extracted via chart review. Symptoms of heartburn, regurgitation, and chest pain were considered typical. Other symptoms were considered atypical. Presence and size of hiatal hernia (HH) was assessed by prior endoscopy. A breakthrough positive result was defined as Acid Exposure Time >4%. Univariate and focused multivariate logistic regression analyses were performed.
Results: 204 patients were included. The median age was 57 years and median BMI was 27. In our cohort, 46% were non-Hispanic (NH) White, 13% where NH Black, 13% were Hispanic, 7% were Asian, and 21% were Other. 37% of patients had a history of tobacco use and 51% had a history of alcohol use. A history of any size hiatal hernia was noted in 23% of patients and 6% had one larger than 2 cm. 39% of patients were tested on once daily PPI. On multivariable analysis, once daily PPI (OR: 3.26, 95% CI: 1.50 - 7.06) and a history of hiatal hernia (OR: 3.33, 95% CI: 1.44 - 7.68) were predictors of having breakthrough acid reflux on testing. Conversely, patients with combined typical and atypical symptoms were less likely to have a positive test (OR: 0.21, 95% CI: 0.08 - 0.59).
Discussion: While off-PPI testing is recommended for patients with unproven GERD, some patients or providers may be hesitant to stop therapy prior to diagnostic testing which may lead to diagnostic uncertainty. This study suggests that if patients do not have atypical symptoms, have a hiatal hernia, or only on once daily PPI, on-PPI testing may still yield breakthrough positive results. Without the presence of these clinical predictors, barriers to off PPI testing should be investigated and addressed.
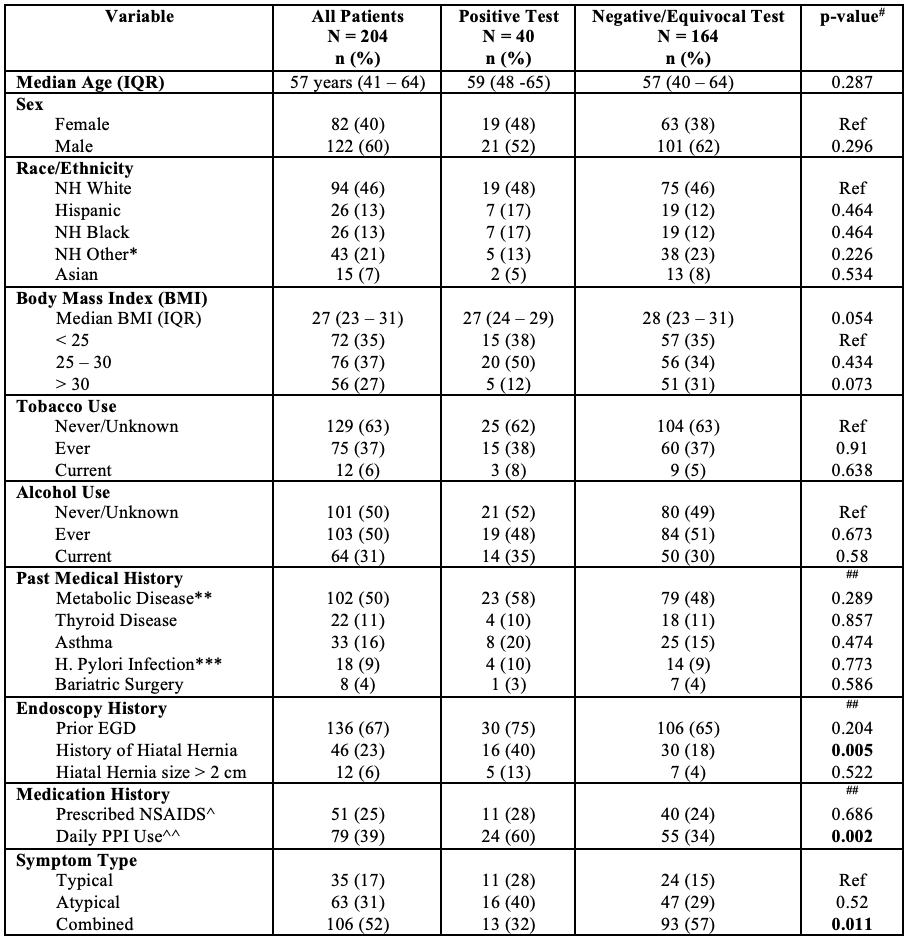
Figure: Table 1. Cohort Characteristics. NH = non-Hispanic, EGD = esophagogastroduodenoscopy, PPI = proton pump inhibitor, H. Pylori = Helicobacter Pylori, Ref = reference group for odds ratio calculation on univariate analysis. *NH Other includes patients with “Unknown” ethnicity. **Metabolic Disease includes having any of the following: Type 2 Diabetes Mellitus, Hypertension, Hyperlipidemia, or Statin use. ***Includes any documented prior infection, regardless of treatment status. ^Includes daily low-dose aspirin. ^^ Non-daily PPI group includes 1 patient prescribed PPI TID and the rest were prescribed PPI BID. #P-values obtained from univariate logistic regression. ##Reference value was patients without the presence of the variable.
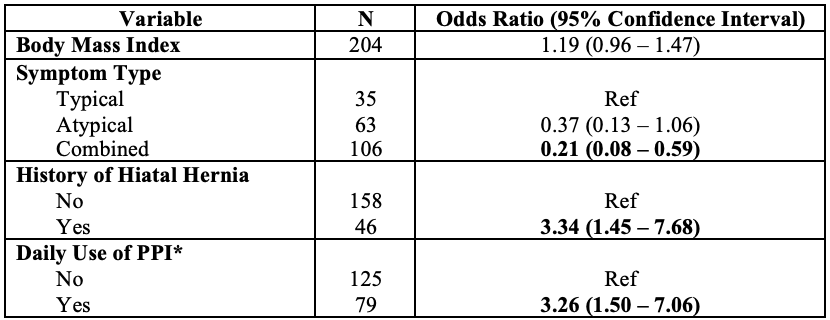
Figure: Table 2. Multivariable Logistic Regression. PPI = proton pump inhibitor. *Non-daily PPI group includes 1 patient prescribed PPI TID and the rest were prescribed PPI BID.
Disclosures:
Ankit Shah indicated no relevant financial relationships.
Daniela Jodorkovsky indicated no relevant financial relationships.
Ankit M.. Shah, MD, Daniela Jodorkovsky, MD. P4926 - Clinical Predictors of Breakthrough Acid Reflux Despite Proton Pump Inhibitor Use During 24-hour pH-Impedance Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

