Tuesday Poster Session
Category: Esophagus
P4923 - Socioeconomic Factors Underlying Treatment Options for Achalasia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LB
Lingyu Bao, MD, PhD
Montefiore Medical Center, Albert Einstein College of Medicine
Bronx, NY
Presenting Author(s)
Lingyu Bao, MD, PhD1, Changlin Gong, MD2, Yichen Wang, MD3, Brian E. Lacy, MD, PhD, FACG4
1Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 2NYC Health + Hospitals/Jacobi, Bronx, NY; 3Hospital of the University of Pennsylvania, Philadelphia, PA; 4Mayo Clinic, Jacksonville, FL, US, Jacksonville, FL
Introduction: Peroral endoscopic myotomy (POEM) was introduced as a treatment for achalasia in 2010. Since then, it has become increasingly well-accepted in clinical practice and recommended in guidelines. We conducted this study to analyze underlying socioeconomic factors that potentially affect treatment choices for achalasia.
Methods: Retrospective data were retrieved from the National Inpatient Sample (NIS) from 2010 to 2022 and the Nationwide Ambulatory Surgery Sample (NASS) from 2016 to 2022. Diagnoses and procedures were identified with Classification of Diseases (ICD) and Current Procedural Terminology (CPT) codes. All adult patients with a primary diagnosis of achalasia were included. Socioeconomic factors including age, insurance, location, and income were compared.
Results: A total of 16,663 admissions with achalasia were included from the NIS database and 6,802 office visits from NASS, representing approximately 83,072 admissions and 8,978 office visits across the US. The numbers of patients undergoing the following treatments in the inpatient vs the outpatient setting are as follows: Heller myotomy (HM), 34,181 vs 5,901; POEM, 3,883 vs 2,039; esophageal dilation, 10,288 vs 160; esophagectomy, 1,305 vs 0; and botulinum toxin injection, 7,943 vs 172.
Patients treated with POEM tend to be older when compared to HM (mean age 58.7 vs 54.9 years, P < 0.001, for inpatients; 57 vs. 48.8 years, P < 0.001, for outpatients). Patients treated with POEM were less likely to have private insurance (39.5% vs 46%, P = 0.005, for inpatients; 23.84% vs. 76.16%, P < 0.001, for outpatients), but more likely to have Medicare (44% vs 37.3% for inpatients, 40.5% vs. 14.1% for outpatients). Patients who underwent POEM tended to have higher Charlson Comorbidity Index (CCI) scores, especially for outpatients: 98.3% of POEM patients had a CCI ≥ 3, compared to only 30% in HM patients. Inpatients treated with POEM are more likely to reside in higher-income locations and more likely to be treated in urban teaching hospitals (93.5% vs 86.4%, P < 0.001).
Discussion: POEM is more commonly performed in older patients and those with limited insurance coverage. In the outpatient setting, POEM is more likely to be performed for patients with a higher number of comorbidities. A possible explanation is its safety and cost-effectiveness. POEM is also more frequently carried out in higher-income and urban settings, where physicians are more likely to have had more training and exposure to this innovative endoscopic procedure.
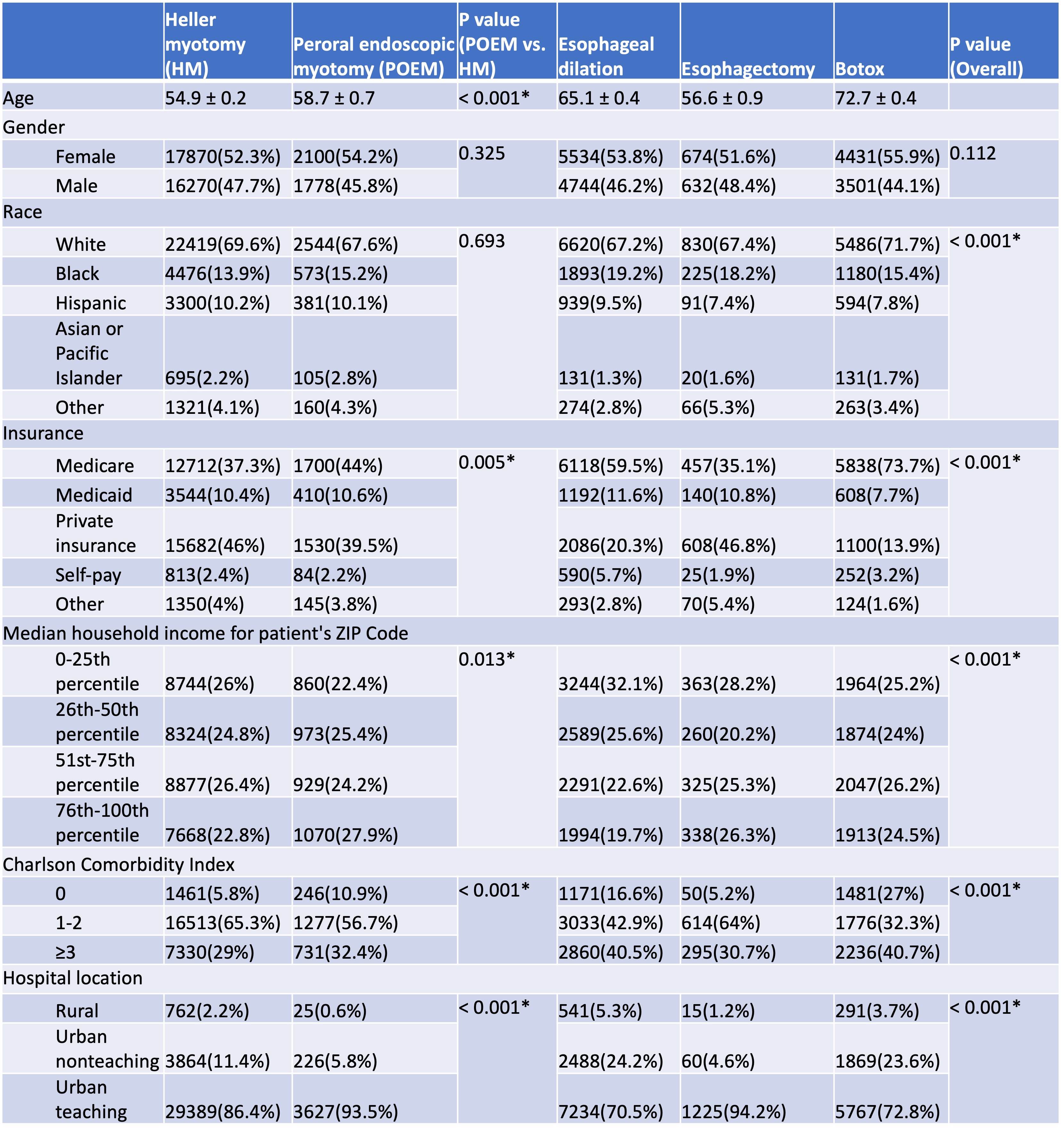
Figure: Socioeconomic characteristics of inpatients who received different procedures for achalasia treatment
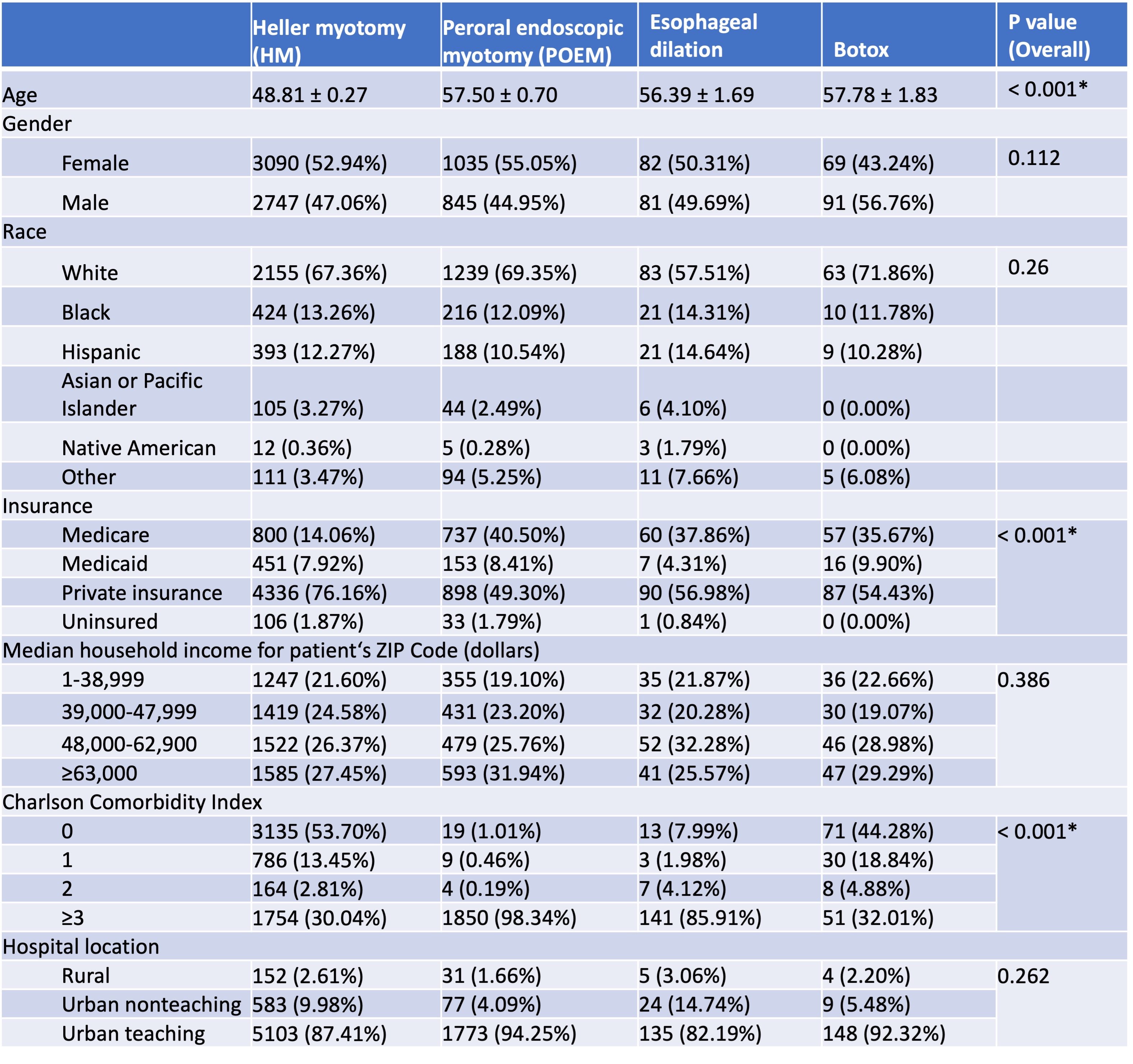
Figure: Socioeconomic characteristics of outpatients who received different procedures for achalasia treatment
Disclosures:
Lingyu Bao indicated no relevant financial relationships.
Changlin Gong indicated no relevant financial relationships.
Yichen Wang indicated no relevant financial relationships.
Brian Lacy: AbbVie – Grant/Research Support. Ardelyx – Consultant. Gemelli Biotech – Consultant. GSK – Consultant. Ironwood Pharmaceuticals – Consultant, Grant/Research Support.
Lingyu Bao, MD, PhD1, Changlin Gong, MD2, Yichen Wang, MD3, Brian E. Lacy, MD, PhD, FACG4. P4923 - Socioeconomic Factors Underlying Treatment Options for Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 2NYC Health + Hospitals/Jacobi, Bronx, NY; 3Hospital of the University of Pennsylvania, Philadelphia, PA; 4Mayo Clinic, Jacksonville, FL, US, Jacksonville, FL
Introduction: Peroral endoscopic myotomy (POEM) was introduced as a treatment for achalasia in 2010. Since then, it has become increasingly well-accepted in clinical practice and recommended in guidelines. We conducted this study to analyze underlying socioeconomic factors that potentially affect treatment choices for achalasia.
Methods: Retrospective data were retrieved from the National Inpatient Sample (NIS) from 2010 to 2022 and the Nationwide Ambulatory Surgery Sample (NASS) from 2016 to 2022. Diagnoses and procedures were identified with Classification of Diseases (ICD) and Current Procedural Terminology (CPT) codes. All adult patients with a primary diagnosis of achalasia were included. Socioeconomic factors including age, insurance, location, and income were compared.
Results: A total of 16,663 admissions with achalasia were included from the NIS database and 6,802 office visits from NASS, representing approximately 83,072 admissions and 8,978 office visits across the US. The numbers of patients undergoing the following treatments in the inpatient vs the outpatient setting are as follows: Heller myotomy (HM), 34,181 vs 5,901; POEM, 3,883 vs 2,039; esophageal dilation, 10,288 vs 160; esophagectomy, 1,305 vs 0; and botulinum toxin injection, 7,943 vs 172.
Patients treated with POEM tend to be older when compared to HM (mean age 58.7 vs 54.9 years, P < 0.001, for inpatients; 57 vs. 48.8 years, P < 0.001, for outpatients). Patients treated with POEM were less likely to have private insurance (39.5% vs 46%, P = 0.005, for inpatients; 23.84% vs. 76.16%, P < 0.001, for outpatients), but more likely to have Medicare (44% vs 37.3% for inpatients, 40.5% vs. 14.1% for outpatients). Patients who underwent POEM tended to have higher Charlson Comorbidity Index (CCI) scores, especially for outpatients: 98.3% of POEM patients had a CCI ≥ 3, compared to only 30% in HM patients. Inpatients treated with POEM are more likely to reside in higher-income locations and more likely to be treated in urban teaching hospitals (93.5% vs 86.4%, P < 0.001).
Discussion: POEM is more commonly performed in older patients and those with limited insurance coverage. In the outpatient setting, POEM is more likely to be performed for patients with a higher number of comorbidities. A possible explanation is its safety and cost-effectiveness. POEM is also more frequently carried out in higher-income and urban settings, where physicians are more likely to have had more training and exposure to this innovative endoscopic procedure.
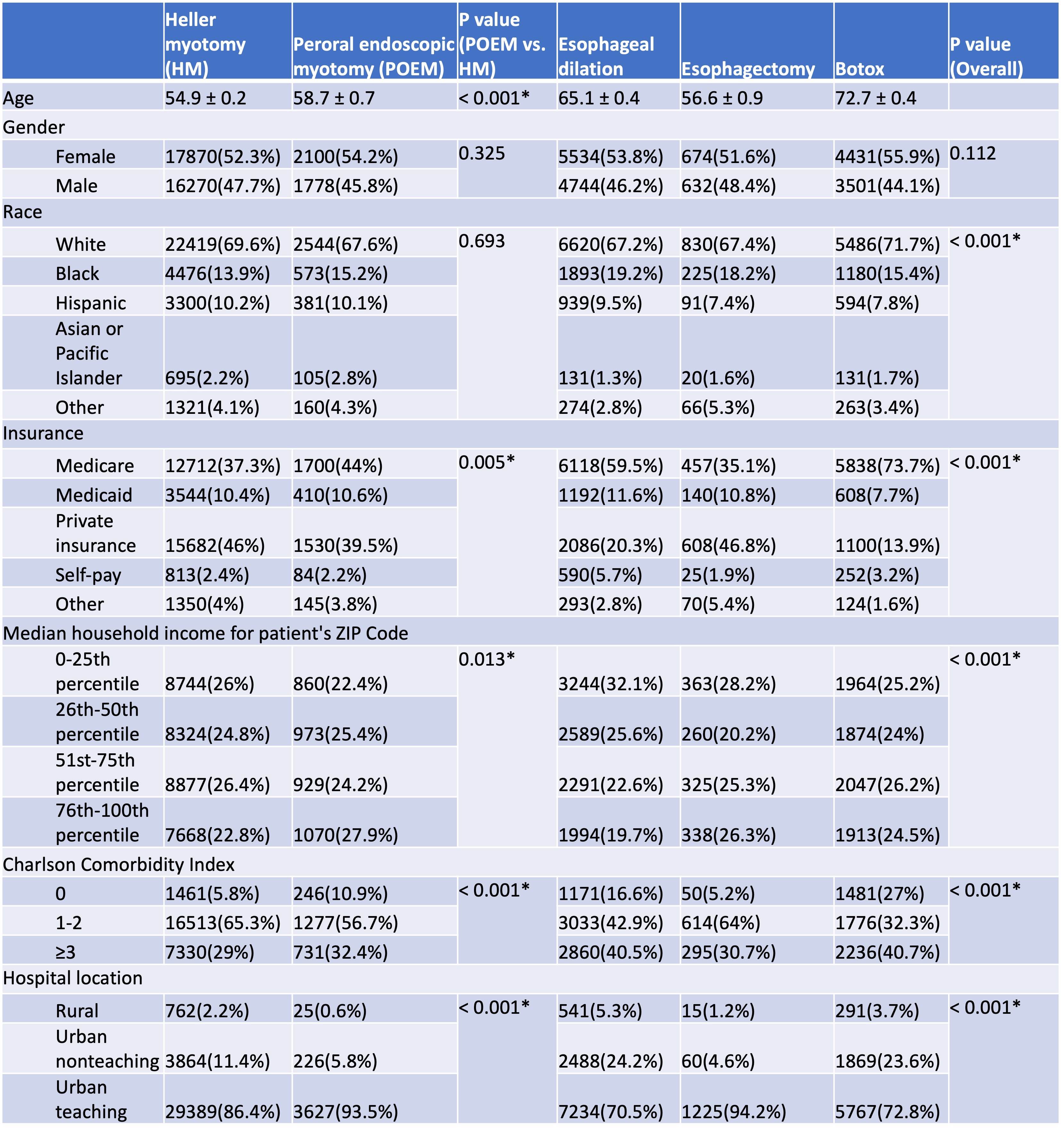
Figure: Socioeconomic characteristics of inpatients who received different procedures for achalasia treatment
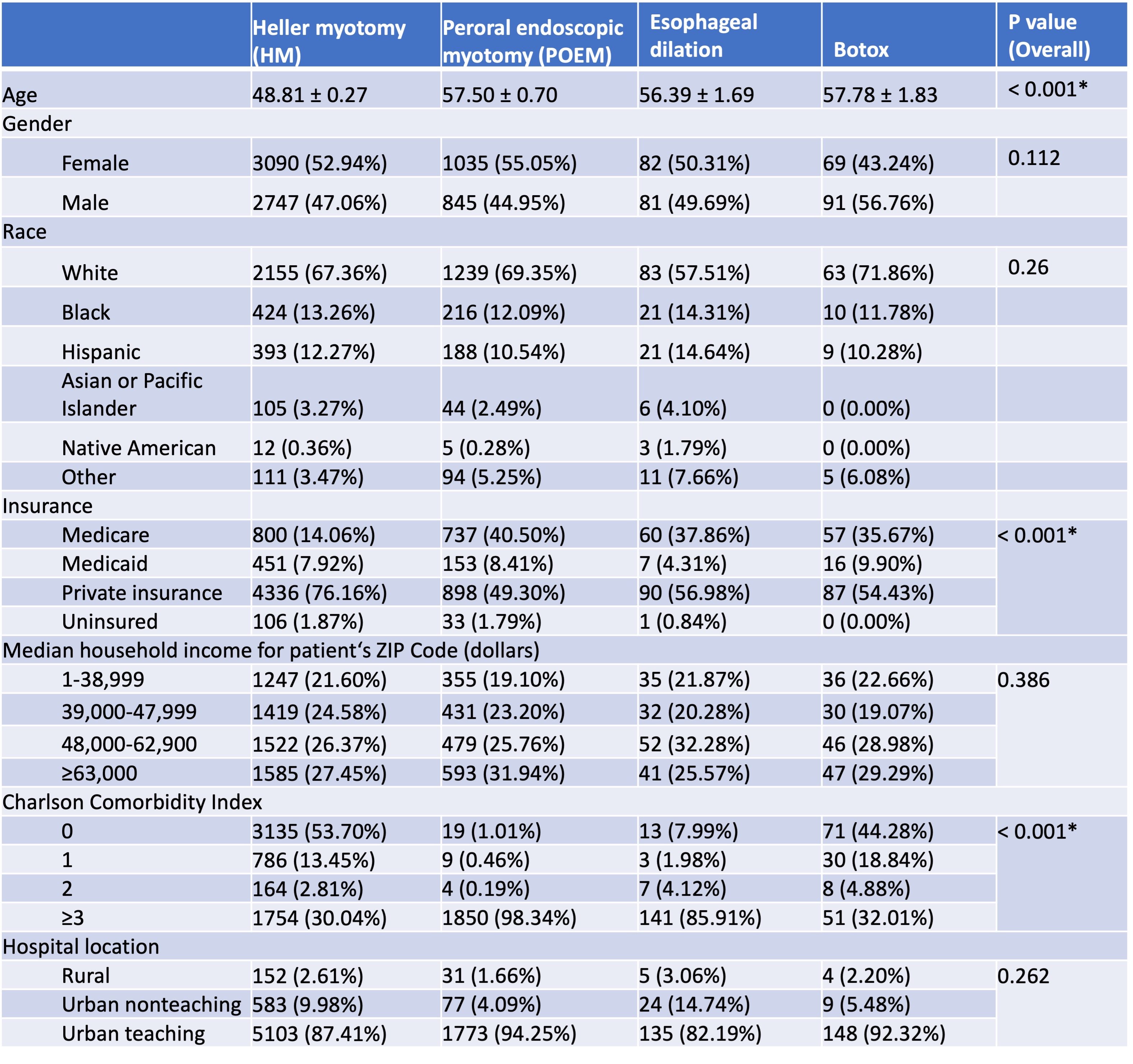
Figure: Socioeconomic characteristics of outpatients who received different procedures for achalasia treatment
Disclosures:
Lingyu Bao indicated no relevant financial relationships.
Changlin Gong indicated no relevant financial relationships.
Yichen Wang indicated no relevant financial relationships.
Brian Lacy: AbbVie – Grant/Research Support. Ardelyx – Consultant. Gemelli Biotech – Consultant. GSK – Consultant. Ironwood Pharmaceuticals – Consultant, Grant/Research Support.
Lingyu Bao, MD, PhD1, Changlin Gong, MD2, Yichen Wang, MD3, Brian E. Lacy, MD, PhD, FACG4. P4923 - Socioeconomic Factors Underlying Treatment Options for Achalasia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
