Tuesday Poster Session
Category: Esophagus
P4917 - Trends in Proton Pump Inhibitor Utilization and Cost in the United States: A Six-Year Analysis of MEPS Data (2017–2022)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Anirudha Chatterjee, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Anirudha Chatterjee, MD, Hari Movva, MD
University of Texas Medical Branch, Galveston, TX
Introduction: Proton pump inhibitors (PPIs) are among the most prescribed medications in the United States. While effective for acid-related disorders, long-term PPI use has raised concerns about overuse, cost, and potential adverse effects. Understanding recent trends in prescribing and cost burden can inform deprescribing efforts and health policy. This study analyzes six years of nationally representative data to assess trends in PPI prescription volume, total costs, and out-of-pocket (OOP) expenses.
Methods: We analyzed public-use data from the Medical Expenditure Panel Survey (MEPS) for 2017–2022. Prescription-level data were extracted from each year’s prescribed medicines file. Records were filtered for all PPI medications (dexlansoprazole, esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole) using generic and brand names. Total cost was defined using the MEPS-imputed variable summing all payment sources; OOP cost was defined as the amount paid by self or family. For each year, we calculated total prescription counts, average total cost per prescription, and average OOP cost.
Results: Between 2017 and 2022, a total of 1,737,845 PPI prescriptions were recorded. Prescription volume peaked in 2018 (319,109) and declined to 232,418 in 2022 (−27.2%). Average total cost per prescription decreased from $86.75 in 2017 to $41.51 in 2022 (−52.2%). OOP costs declined more modestly, from $8.75 to $7.41 (−15.3%). While prescription counts fell after 2021, total costs rebounded from a low of $36.89 in 2021 to $41.51 in 2022.
Discussion: These findings suggest a reversal of the previously documented upward trend in PPI prescribing and expenditures seen through 2017. The decline in volume may reflect greater awareness of PPI overuse, stewardship initiatives, and alignment with AGA recommendations to reassess and deprescribe when no clear indication exists. The marked drop in average prescription costs likely reflects greater use of generics and over-the-counter formulations, along with payer-driven cost controls. In contrast, the smaller decline in OOP costs suggests patient financial burden remains—especially for those requiring long-term therapy. These trends underscore the need to optimize PPI use, reduce unnecessary long-term therapy, and lower healthcare costs, consistent with AGA best practices. Future studies should assess how these trends affect clinical outcomes and prescribing appropriateness.
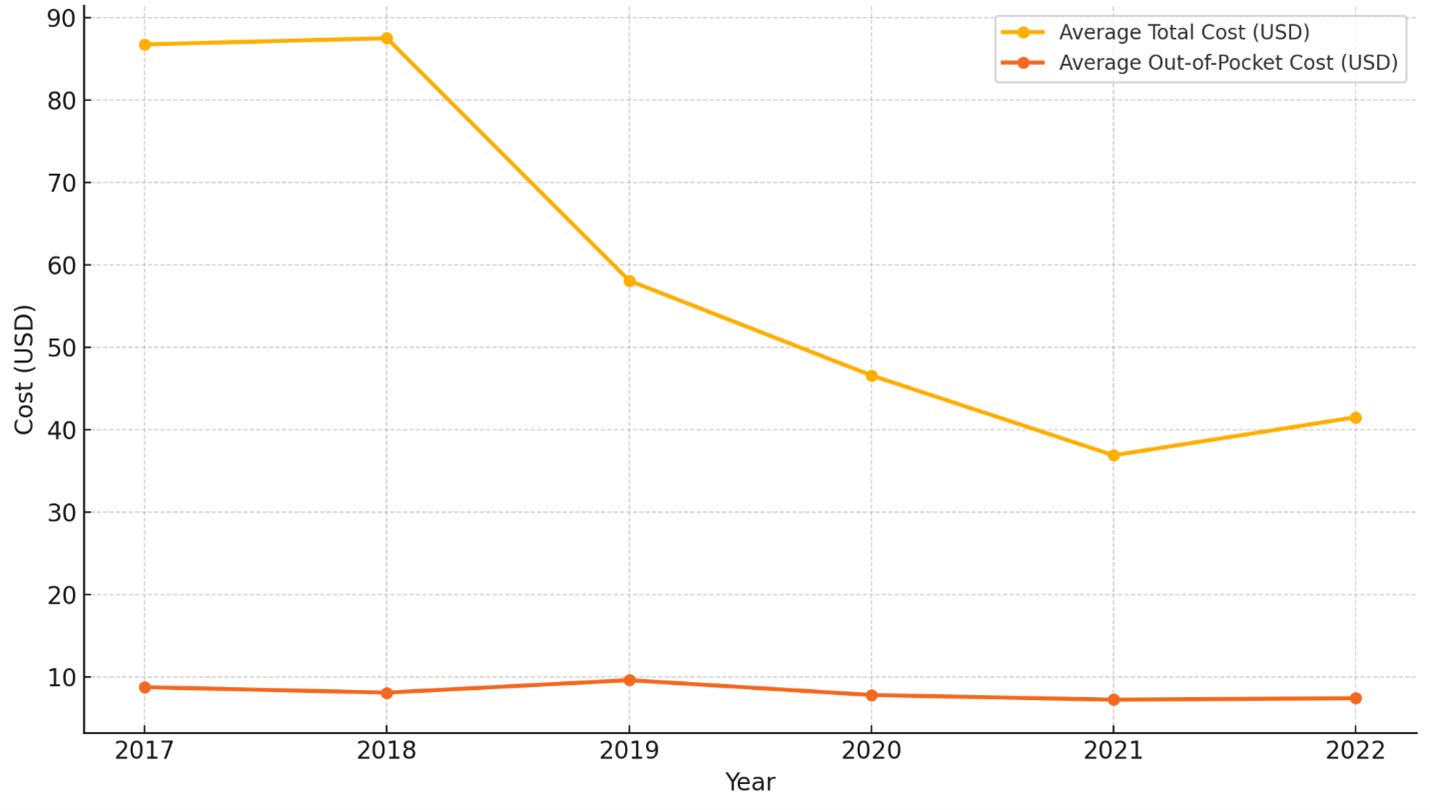
Figure: Trends in Average Total and Out-of-Pocket Costs for PPI Prescriptions from 2017 – 2022
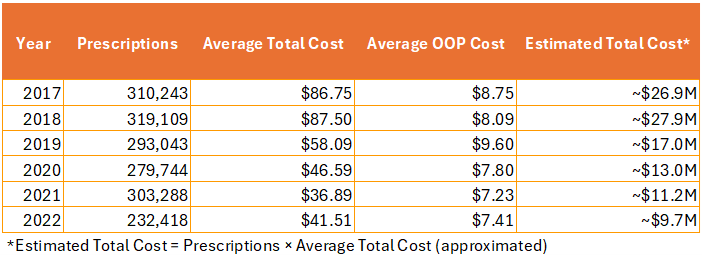
Figure: Estimated Total Cost for PPI Prescriptions from 2017 – 2022
Disclosures:
Anirudha Chatterjee indicated no relevant financial relationships.
Hari Movva indicated no relevant financial relationships.
Anirudha Chatterjee, MD, Hari Movva, MD. P4917 - Trends in Proton Pump Inhibitor Utilization and Cost in the United States: A Six-Year Analysis of MEPS Data (2017–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Medical Branch, Galveston, TX
Introduction: Proton pump inhibitors (PPIs) are among the most prescribed medications in the United States. While effective for acid-related disorders, long-term PPI use has raised concerns about overuse, cost, and potential adverse effects. Understanding recent trends in prescribing and cost burden can inform deprescribing efforts and health policy. This study analyzes six years of nationally representative data to assess trends in PPI prescription volume, total costs, and out-of-pocket (OOP) expenses.
Methods: We analyzed public-use data from the Medical Expenditure Panel Survey (MEPS) for 2017–2022. Prescription-level data were extracted from each year’s prescribed medicines file. Records were filtered for all PPI medications (dexlansoprazole, esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole) using generic and brand names. Total cost was defined using the MEPS-imputed variable summing all payment sources; OOP cost was defined as the amount paid by self or family. For each year, we calculated total prescription counts, average total cost per prescription, and average OOP cost.
Results: Between 2017 and 2022, a total of 1,737,845 PPI prescriptions were recorded. Prescription volume peaked in 2018 (319,109) and declined to 232,418 in 2022 (−27.2%). Average total cost per prescription decreased from $86.75 in 2017 to $41.51 in 2022 (−52.2%). OOP costs declined more modestly, from $8.75 to $7.41 (−15.3%). While prescription counts fell after 2021, total costs rebounded from a low of $36.89 in 2021 to $41.51 in 2022.
Discussion: These findings suggest a reversal of the previously documented upward trend in PPI prescribing and expenditures seen through 2017. The decline in volume may reflect greater awareness of PPI overuse, stewardship initiatives, and alignment with AGA recommendations to reassess and deprescribe when no clear indication exists. The marked drop in average prescription costs likely reflects greater use of generics and over-the-counter formulations, along with payer-driven cost controls. In contrast, the smaller decline in OOP costs suggests patient financial burden remains—especially for those requiring long-term therapy. These trends underscore the need to optimize PPI use, reduce unnecessary long-term therapy, and lower healthcare costs, consistent with AGA best practices. Future studies should assess how these trends affect clinical outcomes and prescribing appropriateness.
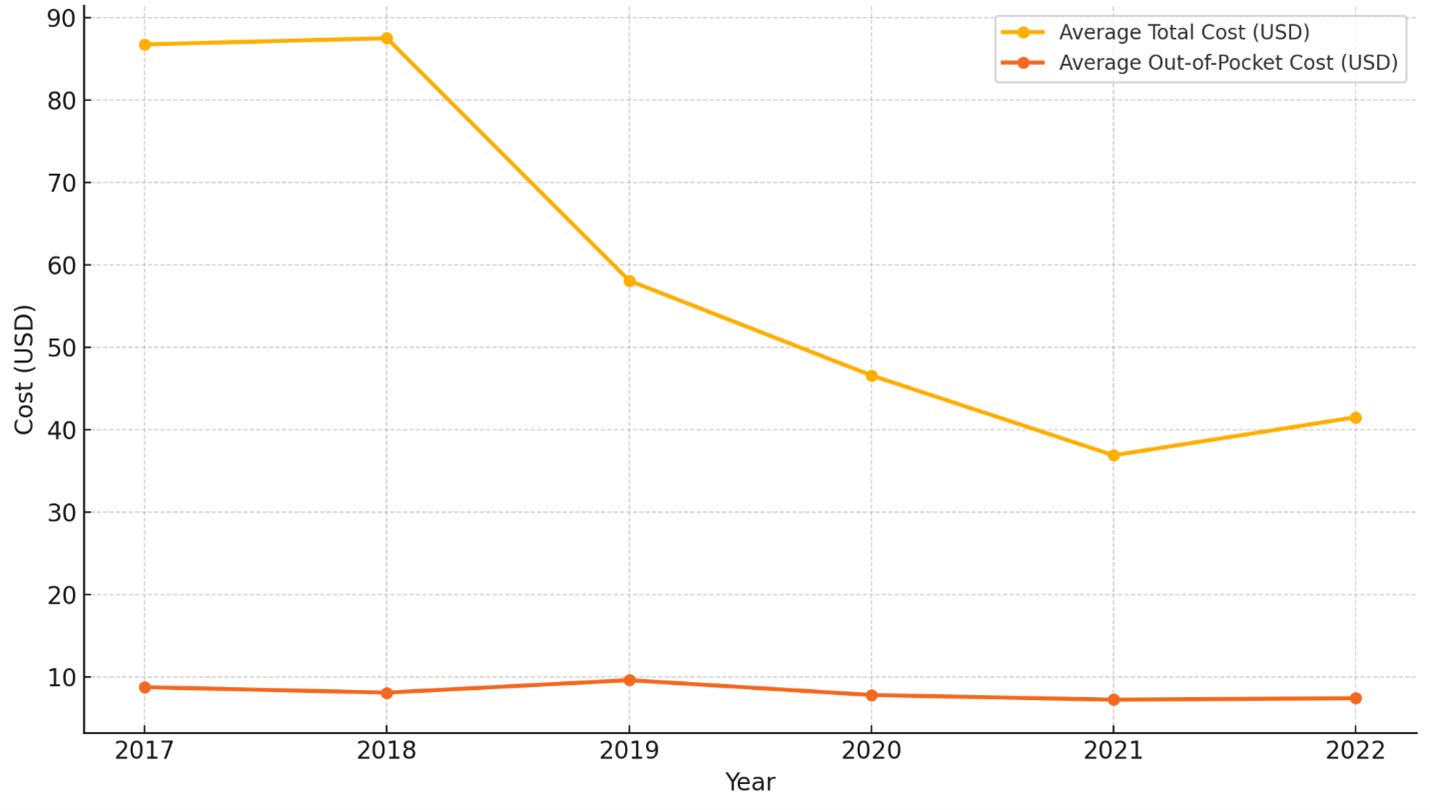
Figure: Trends in Average Total and Out-of-Pocket Costs for PPI Prescriptions from 2017 – 2022
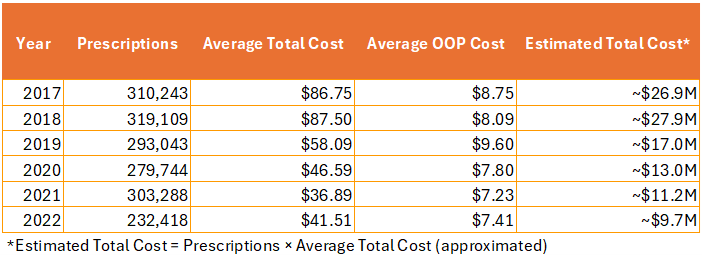
Figure: Estimated Total Cost for PPI Prescriptions from 2017 – 2022
Disclosures:
Anirudha Chatterjee indicated no relevant financial relationships.
Hari Movva indicated no relevant financial relationships.
Anirudha Chatterjee, MD, Hari Movva, MD. P4917 - Trends in Proton Pump Inhibitor Utilization and Cost in the United States: A Six-Year Analysis of MEPS Data (2017–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
