Tuesday Poster Session
Category: Esophagus
P4898 - Long-Term Safety and Efficacy of LINX Magnetic Sphincter Augmentation for GERD: Systematic Review and Meta-analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ifrah Fatima, MD
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Mohamed Ahmed, MD1, Pallavi Jonnalagadda, BSE2, Azha Fatima, MBBS3, Fateen Shareef, MBBS4, Osama Asad, MD1, Sreeni Jonnalagadda, MD5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Washington University School of Medicine in St. Louis, Saint Louis, MO; 3Kamineni Institute of Medical Sciences, Hyderabad, Telangana, India; 4Deccan College of Medical Sciences, Hyderabad, Telangana, India; 5Saint Luke's Health System of Kansas City, Kansas City, MO
Introduction: Magnetic sphincter augmentation (MSA) is an increasingly utilized surgical option for patients with gastroesophageal reflux disease (GERD). The device consists of a series of titanium beads with magnetic cores that serve to augment the barrier function of the lower esophageal sphincter while also allowing for expansion to accommodate a swallowed bolus. Postoperative dysphagia remains the most common complaint by patients after MSA that is often managed by endoscopic balloon dilation.
Methods: Six databases (Pubmed, Scopus, Embase, Medline, Web of Science, CCRCT) were screened from inception up until Jan 2025. The search utilized relevant keywords and MeSH terms to include studies that evaluated outcomes after MSA placement. Outcomes of interest included post operative dysphagia, freedom from proton pump inhibitors (PPI), rates of device removal. Standard meta-analysis methodology was followed using the random-effects model, and heterogeneity was assessed by I2 statistics.
Results: A total of 7 studies were included in the final analysis. Six studies (n = 1589) reported freedom from daily PPIs at ≥ 10 months. Pooled incidence was 0.89 (95 % CI 0.86-0.92; I² = 56 %), indicating that about 9 in 10 patients discontinued antisecretory medication long-term.
Six studies (n=1589) reported postoperative dysphagia requiring endoscopic dilation. Incidence varied widely (0 – 43 %). The pooled estimate was 0.07 (95 % CI 0.02-0.22; I² = 93 %). All seven studies reported device removal (n = 1733). The pooled explantation rate was low at 0.03 (95 % CI 0.02-0.07) but heterogeneity remained substantial (I² = 85 %), driven by a single dilation-focused cohort. Sub-analysis excluding that outlier (Fletcher 2022) reduced I² to 49 % and the rate to 0.02 (95 % CI 0.01-0.04).
Discussion: Our meta-analysis demonstrated significant and durable PPI freedom in about 90% of GERD patients treated with MSA. Device failure requiring explantation remains uncommon at 2-3%. Dysphagia is a significant side effect necessitating dilation in about 7% patients. Effective endoscopic dilation remains an area to be explored. Further large scale RCTs are needed for a more comprehensive understanding of risk prediction and effective treatment options for dysphagia.
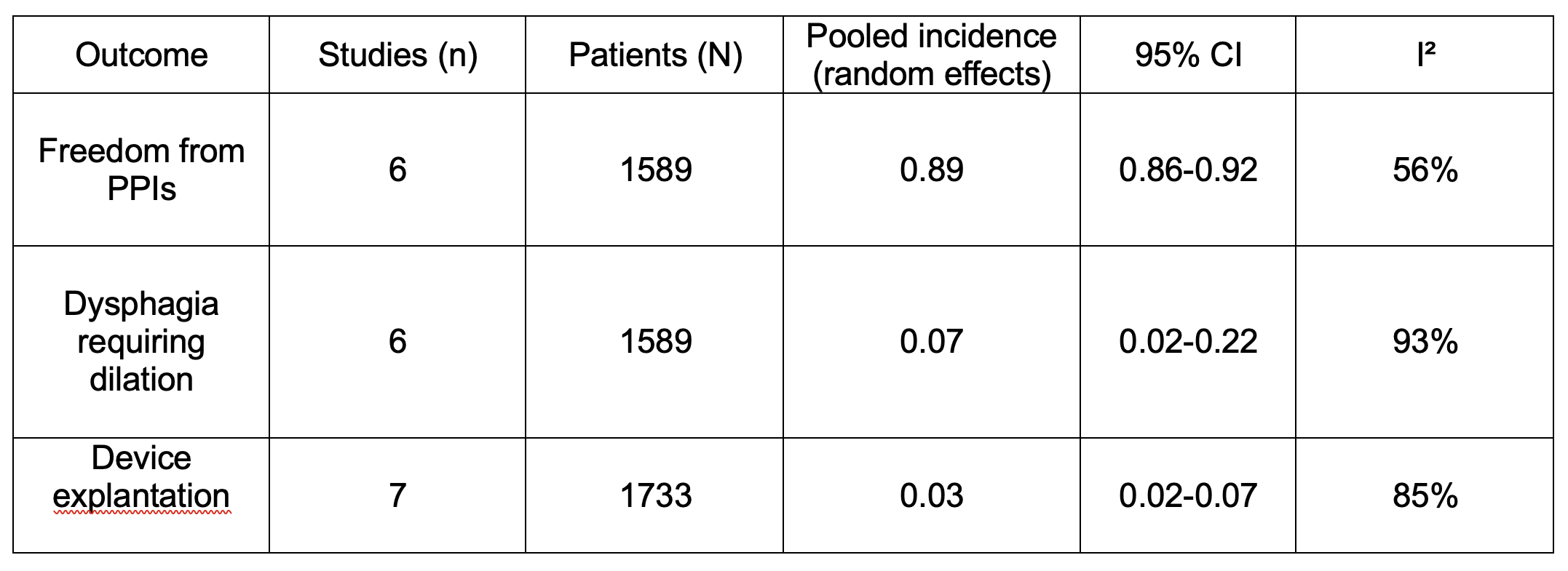
Figure: Table-1: Summary of pooled rates
Disclosures:
Ifrah Fatima indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Pallavi Jonnalagadda indicated no relevant financial relationships.
Azha Fatima indicated no relevant financial relationships.
Fateen Shareef indicated no relevant financial relationships.
Osama Asad indicated no relevant financial relationships.
Sreeni Jonnalagadda indicated no relevant financial relationships.
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Mohamed Ahmed, MD1, Pallavi Jonnalagadda, BSE2, Azha Fatima, MBBS3, Fateen Shareef, MBBS4, Osama Asad, MD1, Sreeni Jonnalagadda, MD5. P4898 - Long-Term Safety and Efficacy of LINX Magnetic Sphincter Augmentation for GERD: Systematic Review and Meta-analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Washington University School of Medicine in St. Louis, Saint Louis, MO; 3Kamineni Institute of Medical Sciences, Hyderabad, Telangana, India; 4Deccan College of Medical Sciences, Hyderabad, Telangana, India; 5Saint Luke's Health System of Kansas City, Kansas City, MO
Introduction: Magnetic sphincter augmentation (MSA) is an increasingly utilized surgical option for patients with gastroesophageal reflux disease (GERD). The device consists of a series of titanium beads with magnetic cores that serve to augment the barrier function of the lower esophageal sphincter while also allowing for expansion to accommodate a swallowed bolus. Postoperative dysphagia remains the most common complaint by patients after MSA that is often managed by endoscopic balloon dilation.
Methods: Six databases (Pubmed, Scopus, Embase, Medline, Web of Science, CCRCT) were screened from inception up until Jan 2025. The search utilized relevant keywords and MeSH terms to include studies that evaluated outcomes after MSA placement. Outcomes of interest included post operative dysphagia, freedom from proton pump inhibitors (PPI), rates of device removal. Standard meta-analysis methodology was followed using the random-effects model, and heterogeneity was assessed by I2 statistics.
Results: A total of 7 studies were included in the final analysis. Six studies (n = 1589) reported freedom from daily PPIs at ≥ 10 months. Pooled incidence was 0.89 (95 % CI 0.86-0.92; I² = 56 %), indicating that about 9 in 10 patients discontinued antisecretory medication long-term.
Six studies (n=1589) reported postoperative dysphagia requiring endoscopic dilation. Incidence varied widely (0 – 43 %). The pooled estimate was 0.07 (95 % CI 0.02-0.22; I² = 93 %). All seven studies reported device removal (n = 1733). The pooled explantation rate was low at 0.03 (95 % CI 0.02-0.07) but heterogeneity remained substantial (I² = 85 %), driven by a single dilation-focused cohort. Sub-analysis excluding that outlier (Fletcher 2022) reduced I² to 49 % and the rate to 0.02 (95 % CI 0.01-0.04).
Discussion: Our meta-analysis demonstrated significant and durable PPI freedom in about 90% of GERD patients treated with MSA. Device failure requiring explantation remains uncommon at 2-3%. Dysphagia is a significant side effect necessitating dilation in about 7% patients. Effective endoscopic dilation remains an area to be explored. Further large scale RCTs are needed for a more comprehensive understanding of risk prediction and effective treatment options for dysphagia.
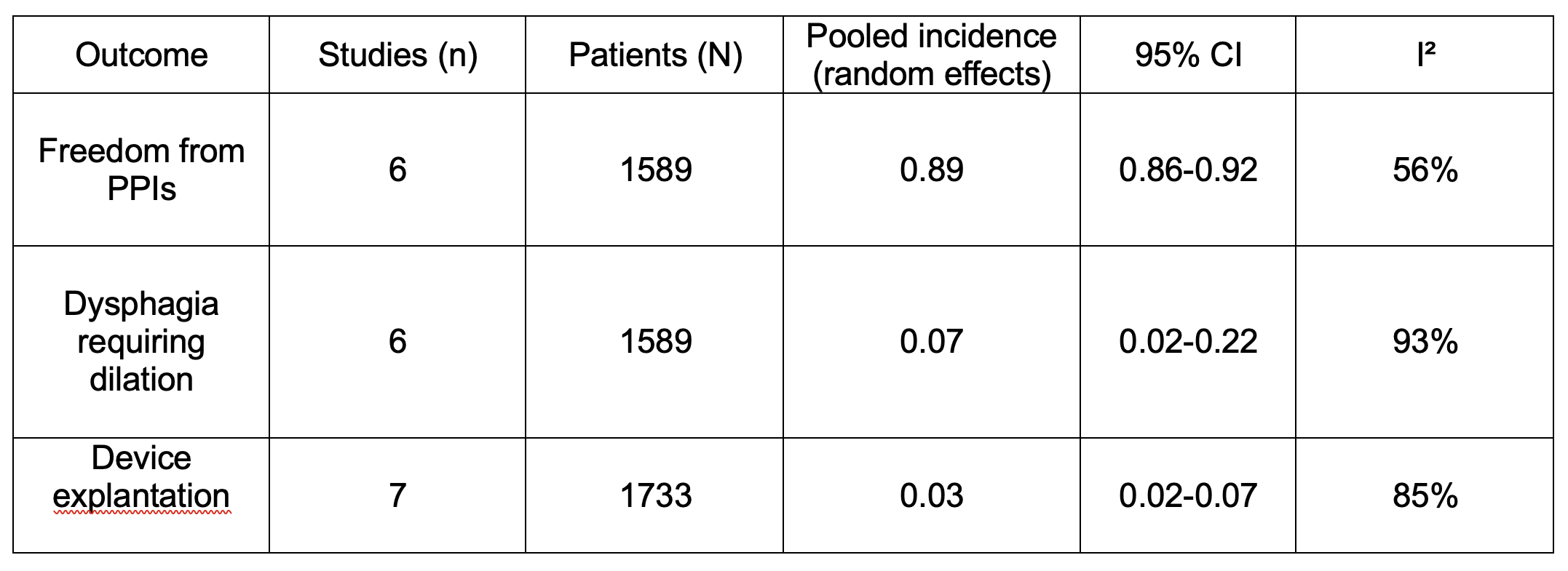
Figure: Table-1: Summary of pooled rates
Disclosures:
Ifrah Fatima indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Pallavi Jonnalagadda indicated no relevant financial relationships.
Azha Fatima indicated no relevant financial relationships.
Fateen Shareef indicated no relevant financial relationships.
Osama Asad indicated no relevant financial relationships.
Sreeni Jonnalagadda indicated no relevant financial relationships.
Ifrah Fatima, MD1, Mir Zulqarnain, DO1, Mohamed Ahmed, MD1, Pallavi Jonnalagadda, BSE2, Azha Fatima, MBBS3, Fateen Shareef, MBBS4, Osama Asad, MD1, Sreeni Jonnalagadda, MD5. P4898 - Long-Term Safety and Efficacy of LINX Magnetic Sphincter Augmentation for GERD: Systematic Review and Meta-analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
