Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4853 - Retained Fundic Shelf After Bariatric Surgery: Identification of Disease, Presentation, and Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nakul Bhardwaj, DO, MPH (he/him/his)
University of Utah
Salt Lake City, UT
Presenting Author(s)
Nakul Bhardwaj, DO, MPH1, Meeta Bhardwaj, DO, MPH2, Mina Awadallah, MD, MSc1, John Erikson Yap, MD, MBA, FACG3
1University of Utah, Salt Lake City, UT; 2Cleveland Clinic Foundation, Cleveland, OH; 3University of Utah Health, Salt Lake City, UT
Introduction: A retained fundic shelf is a recognized anatomical variant following sleeve gastrectomy, defined as incomplete resection of the gastric fundus during surgery. This residual segment, typically located near the gastroesophageal junction, can be identified on imaging or upper endoscopy. Although sometimes asymptomatic, a retained fundus may promote food pooling and delayed gastric emptying, contributing to worsened gastroesophageal reflux disease (GERD), impaired satiety, and weight regain. These symptoms may be resistant to medical management and ultimately necessitate revisional surgery, which carries greater risk than primary procedures. As the prevalence of obesity continues to rise and more patients undergo metabolic and bariatric surgery, gastroenterologists will increasingly encounter altered post-surgical anatomy during endoscopy. Awareness of these anatomic variants, including the retained fundic shelf, is essential for accurate diagnosis, symptom attribution, and treatment planning. We present a case of a patient who underwent metabolic and bariatric surgery with such complication.
Case Description/
Methods: A 50-year-old woman with sarcoidosis and obesity underwent laparoscopic Roux-en-Y gastric bypass in 2002. Months later, she developed intolerable postprandial epigastric pain and underwent reversal to sleeve gastrectomy with lysis of adhesions. Her symptoms improved for several years but recurred with acute-on-chronic epigastric pain, dysphagia to solids, and the sensation of pills or food lodging in her upper abdomen. Pain typically began 30 minutes after eating and sometimes occurred at night. A CT scan for sarcoidosis surveillance revealed a paraesophageal hernia with the staple line of the sleeve above the diaphragm and mild sleeve angulation. EGD revealed LA Grade B esophagitis and a large intragastric outpouching with retained food, consistent with a retained fundic shelf. Upper GI series confirmed contrast pooling near the gastroesophageal junction, consistent with a diverticulum-like structure.
Discussion: This case emphasizes the need to recognize a retained fundic shelf as a cause of refractory symptoms following metabolic and bariatric surgery. The residual segment may impair satiety signals, worsen GERD, and compromise long-term surgical efficacy. Familiarity with this variant supports accurate endoscopic interpretation and informs potential revision strategies, such as completion fundectomy.
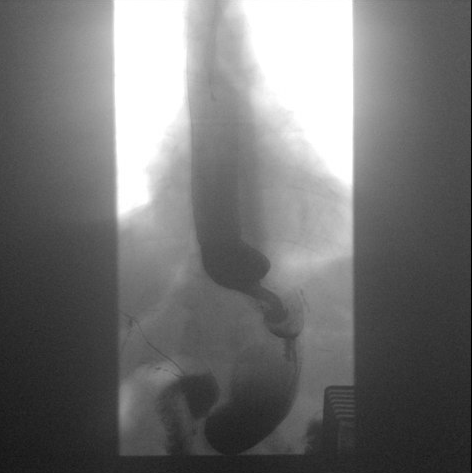
Figure: Endoscopic view of the gastric inlet demonstrating a prominent, slightly dependent gastric fundus (“retained fundic shelf”) with an adjacent diverticulum. Such anatomical finding may contribute to symptoms such as reflux or poor emptying.
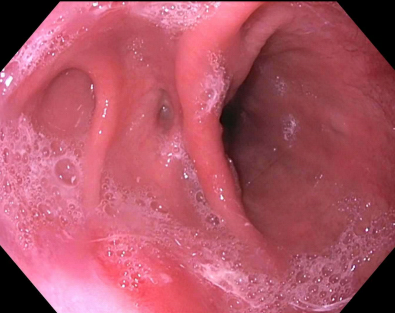
Figure: Retained fundic shelf identified on upper GI series following sleeve gastrectomy. This finding appears as a significant outpouching near the gastroesophageal junction. It is often associated with persistent symptoms like dysphagia, reflux, or the need for revision surgery.
Disclosures:
Nakul Bhardwaj indicated no relevant financial relationships.
Meeta Bhardwaj indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Nakul Bhardwaj, DO, MPH1, Meeta Bhardwaj, DO, MPH2, Mina Awadallah, MD, MSc1, John Erikson Yap, MD, MBA, FACG3. P4853 - Retained Fundic Shelf After Bariatric Surgery: Identification of Disease, Presentation, and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2Cleveland Clinic Foundation, Cleveland, OH; 3University of Utah Health, Salt Lake City, UT
Introduction: A retained fundic shelf is a recognized anatomical variant following sleeve gastrectomy, defined as incomplete resection of the gastric fundus during surgery. This residual segment, typically located near the gastroesophageal junction, can be identified on imaging or upper endoscopy. Although sometimes asymptomatic, a retained fundus may promote food pooling and delayed gastric emptying, contributing to worsened gastroesophageal reflux disease (GERD), impaired satiety, and weight regain. These symptoms may be resistant to medical management and ultimately necessitate revisional surgery, which carries greater risk than primary procedures. As the prevalence of obesity continues to rise and more patients undergo metabolic and bariatric surgery, gastroenterologists will increasingly encounter altered post-surgical anatomy during endoscopy. Awareness of these anatomic variants, including the retained fundic shelf, is essential for accurate diagnosis, symptom attribution, and treatment planning. We present a case of a patient who underwent metabolic and bariatric surgery with such complication.
Case Description/
Methods: A 50-year-old woman with sarcoidosis and obesity underwent laparoscopic Roux-en-Y gastric bypass in 2002. Months later, she developed intolerable postprandial epigastric pain and underwent reversal to sleeve gastrectomy with lysis of adhesions. Her symptoms improved for several years but recurred with acute-on-chronic epigastric pain, dysphagia to solids, and the sensation of pills or food lodging in her upper abdomen. Pain typically began 30 minutes after eating and sometimes occurred at night. A CT scan for sarcoidosis surveillance revealed a paraesophageal hernia with the staple line of the sleeve above the diaphragm and mild sleeve angulation. EGD revealed LA Grade B esophagitis and a large intragastric outpouching with retained food, consistent with a retained fundic shelf. Upper GI series confirmed contrast pooling near the gastroesophageal junction, consistent with a diverticulum-like structure.
Discussion: This case emphasizes the need to recognize a retained fundic shelf as a cause of refractory symptoms following metabolic and bariatric surgery. The residual segment may impair satiety signals, worsen GERD, and compromise long-term surgical efficacy. Familiarity with this variant supports accurate endoscopic interpretation and informs potential revision strategies, such as completion fundectomy.
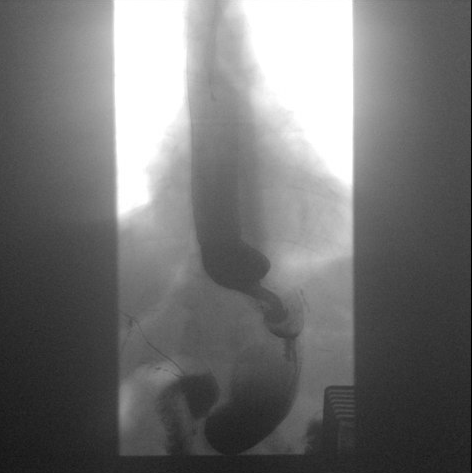
Figure: Endoscopic view of the gastric inlet demonstrating a prominent, slightly dependent gastric fundus (“retained fundic shelf”) with an adjacent diverticulum. Such anatomical finding may contribute to symptoms such as reflux or poor emptying.
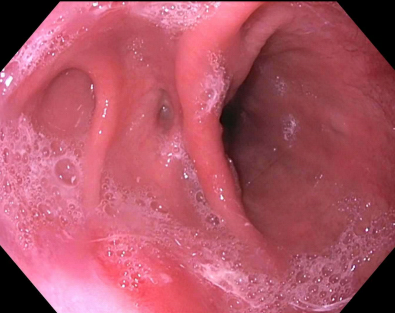
Figure: Retained fundic shelf identified on upper GI series following sleeve gastrectomy. This finding appears as a significant outpouching near the gastroesophageal junction. It is often associated with persistent symptoms like dysphagia, reflux, or the need for revision surgery.
Disclosures:
Nakul Bhardwaj indicated no relevant financial relationships.
Meeta Bhardwaj indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Nakul Bhardwaj, DO, MPH1, Meeta Bhardwaj, DO, MPH2, Mina Awadallah, MD, MSc1, John Erikson Yap, MD, MBA, FACG3. P4853 - Retained Fundic Shelf After Bariatric Surgery: Identification of Disease, Presentation, and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

