Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4848 - University Students Are Vulnerable to Food Insecurity and Social Determinants of Health Among Patients With Gastrointestinal Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark R. Baniqued, MD
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Mark R. Baniqued, MD1, Rhett Harmon, MD1, Alexandra Greb, MD2, Bita Shahrvini, MD2, Marc Kaneshiro, MD2, Wendy Ho, MD2, Guy A. Weiss, MD3, Jenny Sauk, MD2, Nirupama Bonthala, MD2, Jaden Nguyen, 2, Andrew Nguyen, 2, Jia Hui Hai, 2, Brendan Field, 2, Andrew Roney, MD2, Janelle Smith, MS, RD, CEDRD2, Neha D. Shah, MPH, RD, CNSC, CHES4, Xiaoxiao Yin, 2, Folasade May, MD, PhD, MPhil2, Simon Beaven, MD, PhD5, Berkeley Limketkai, MD, PhD2
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3University of California Los Angeles Medical Center, Los Angeles, CA; 4University of California San Francisco, San Francisco, CA; 5Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Social determinants of health (SDOH) significantly impact patients with gastrointestinal (GI) diseases, influencing outcomes and healthcare utilization. Food insecurity limits options and can worsen GI disorder symptoms by hindering nutritional therapy. This study examines the prevalence and risk factors of food insecurity and other SDOH among GI patients at a large academic medical center affiliated with a public university in an affluent neighborhood.
Methods: From August to November 2024, patients at a tertiary-care gastroenterology clinic were invited to complete a survey on food security and SDOH. Validated instruments were used, including the American Academy of Family Physicians SDOH Screening Tool, the United States Department of Agriculture’s Six-Item Short Form Food Security Survey Module, and the Malnutrition Screening Tool. Demographic data, including employment and student status, were collected from electronic medical records. Descriptive analyses assessed the prevalence of food insecurity and related SDOH risks. Multivariable linear regression models adjusted for confounders identified risk factors for food insecurity.
Results: This study included 118 GI patients (mean age 45.1 ± 17.6, 64.2% female, 77.6% white, 52.2% married, 76.9% with a college degree, and 7.8% students). Low or very low food security affected 11.1% of students and 7.4% of non-students (Table 1). A quarter of students indicated "sometimes" or "often" being "…worried that your food would run out before you got money to buy more" and "...the food you bought just didn’t last, and you didn’t have money to get more.” Malnutrition risk was more prevalent among students than non-students (44.4% vs. 18.3%, p=0.06). In multivariable models, being a student was associated with a significantly higher food insecurity score (+1.77, 95% CI 0.54-2.99, p< 0.01) (Table 2). Further examination of other SDOH variables showed students had a significantly higher prevalence of household utility insecurity risk (p< 0.001) and risks to personal safety (p< 0.001).
Discussion: Food insecurity was low among GI patients at our medical center. However, students experienced higher levels of food insecurity, limited access to utilities, and greater risks to personal safety compared to non-students. Even in affluent neighborhoods, university students are a vulnerable population in terms of food insecurity, malnutrition, and safety. Recognizing and addressing these disparities can lead to improved clinical outcomes for this group.
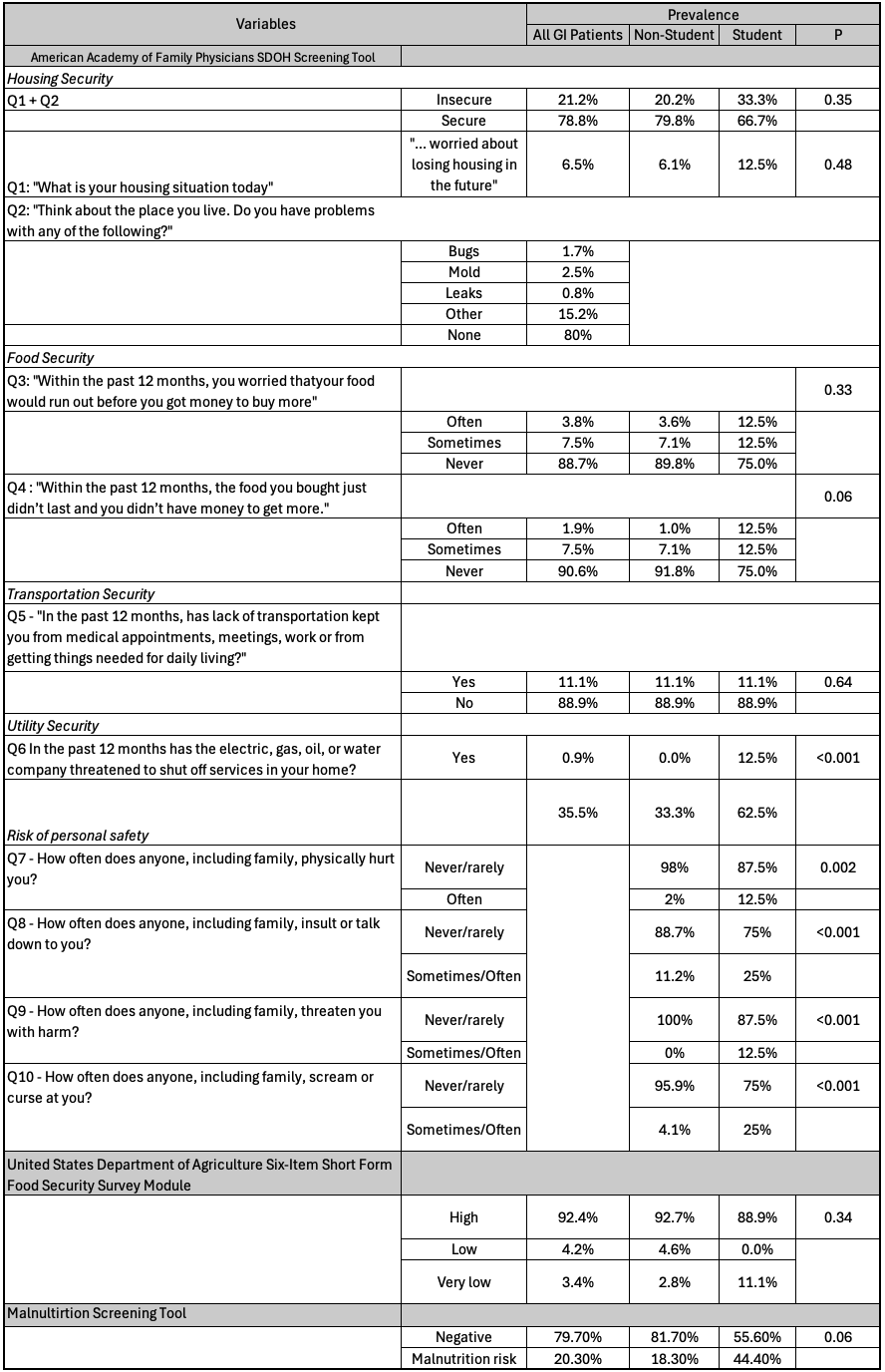
Figure: Patient survey responses to the American Academy of Family Physicians SDOH Screening tool, United States Department of Agriculture Six-Item Short Form Food Security Survey Module, and Malnutrition Screening Tool for all 118 GI patients and comparing non-students versus students.
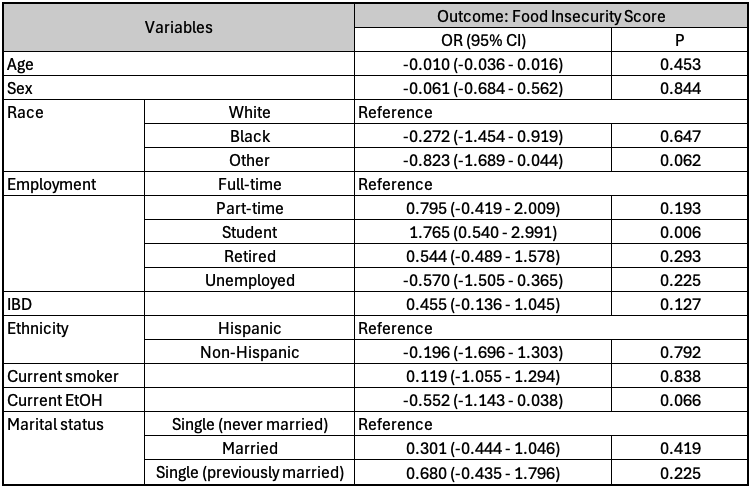
Figure: Multivariable linear regression analysis of the food insecurity score (a higher score indicates a greater risk of food insecurity) when adjusted for Age, Sex, Race, Employment, IBD, Ethnicity, Current Smoking Status, Current Alcohol (EtOH) use status, and Marital status.
Disclosures:
Mark Baniqued indicated no relevant financial relationships.
Rhett Harmon indicated no relevant financial relationships.
Alexandra Greb indicated no relevant financial relationships.
Bita Shahrvini indicated no relevant financial relationships.
Marc Kaneshiro indicated no relevant financial relationships.
Wendy Ho indicated no relevant financial relationships.
Guy Weiss: Guidepoint – Consultant. Regeneron – Consultant.
Jenny Sauk indicated no relevant financial relationships.
Nirupama Bonthala indicated no relevant financial relationships.
Jaden Nguyen indicated no relevant financial relationships.
Andrew Nguyen indicated no relevant financial relationships.
Jia Hui Hai indicated no relevant financial relationships.
Brendan Field indicated no relevant financial relationships.
Andrew Roney indicated no relevant financial relationships.
Janelle Smith indicated no relevant financial relationships.
Neha Shah: GI on Demand – Consultant.
Xiaoxiao Yin indicated no relevant financial relationships.
Folasade May indicated no relevant financial relationships.
Simon Beaven: Alnylam – Speakers Bureau.
Berkeley Limketkai indicated no relevant financial relationships.
Mark R. Baniqued, MD1, Rhett Harmon, MD1, Alexandra Greb, MD2, Bita Shahrvini, MD2, Marc Kaneshiro, MD2, Wendy Ho, MD2, Guy A. Weiss, MD3, Jenny Sauk, MD2, Nirupama Bonthala, MD2, Jaden Nguyen, 2, Andrew Nguyen, 2, Jia Hui Hai, 2, Brendan Field, 2, Andrew Roney, MD2, Janelle Smith, MS, RD, CEDRD2, Neha D. Shah, MPH, RD, CNSC, CHES4, Xiaoxiao Yin, 2, Folasade May, MD, PhD, MPhil2, Simon Beaven, MD, PhD5, Berkeley Limketkai, MD, PhD2. P4848 - University Students Are Vulnerable to Food Insecurity and Social Determinants of Health Among Patients With Gastrointestinal Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3University of California Los Angeles Medical Center, Los Angeles, CA; 4University of California San Francisco, San Francisco, CA; 5Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Social determinants of health (SDOH) significantly impact patients with gastrointestinal (GI) diseases, influencing outcomes and healthcare utilization. Food insecurity limits options and can worsen GI disorder symptoms by hindering nutritional therapy. This study examines the prevalence and risk factors of food insecurity and other SDOH among GI patients at a large academic medical center affiliated with a public university in an affluent neighborhood.
Methods: From August to November 2024, patients at a tertiary-care gastroenterology clinic were invited to complete a survey on food security and SDOH. Validated instruments were used, including the American Academy of Family Physicians SDOH Screening Tool, the United States Department of Agriculture’s Six-Item Short Form Food Security Survey Module, and the Malnutrition Screening Tool. Demographic data, including employment and student status, were collected from electronic medical records. Descriptive analyses assessed the prevalence of food insecurity and related SDOH risks. Multivariable linear regression models adjusted for confounders identified risk factors for food insecurity.
Results: This study included 118 GI patients (mean age 45.1 ± 17.6, 64.2% female, 77.6% white, 52.2% married, 76.9% with a college degree, and 7.8% students). Low or very low food security affected 11.1% of students and 7.4% of non-students (Table 1). A quarter of students indicated "sometimes" or "often" being "…worried that your food would run out before you got money to buy more" and "...the food you bought just didn’t last, and you didn’t have money to get more.” Malnutrition risk was more prevalent among students than non-students (44.4% vs. 18.3%, p=0.06). In multivariable models, being a student was associated with a significantly higher food insecurity score (+1.77, 95% CI 0.54-2.99, p< 0.01) (Table 2). Further examination of other SDOH variables showed students had a significantly higher prevalence of household utility insecurity risk (p< 0.001) and risks to personal safety (p< 0.001).
Discussion: Food insecurity was low among GI patients at our medical center. However, students experienced higher levels of food insecurity, limited access to utilities, and greater risks to personal safety compared to non-students. Even in affluent neighborhoods, university students are a vulnerable population in terms of food insecurity, malnutrition, and safety. Recognizing and addressing these disparities can lead to improved clinical outcomes for this group.
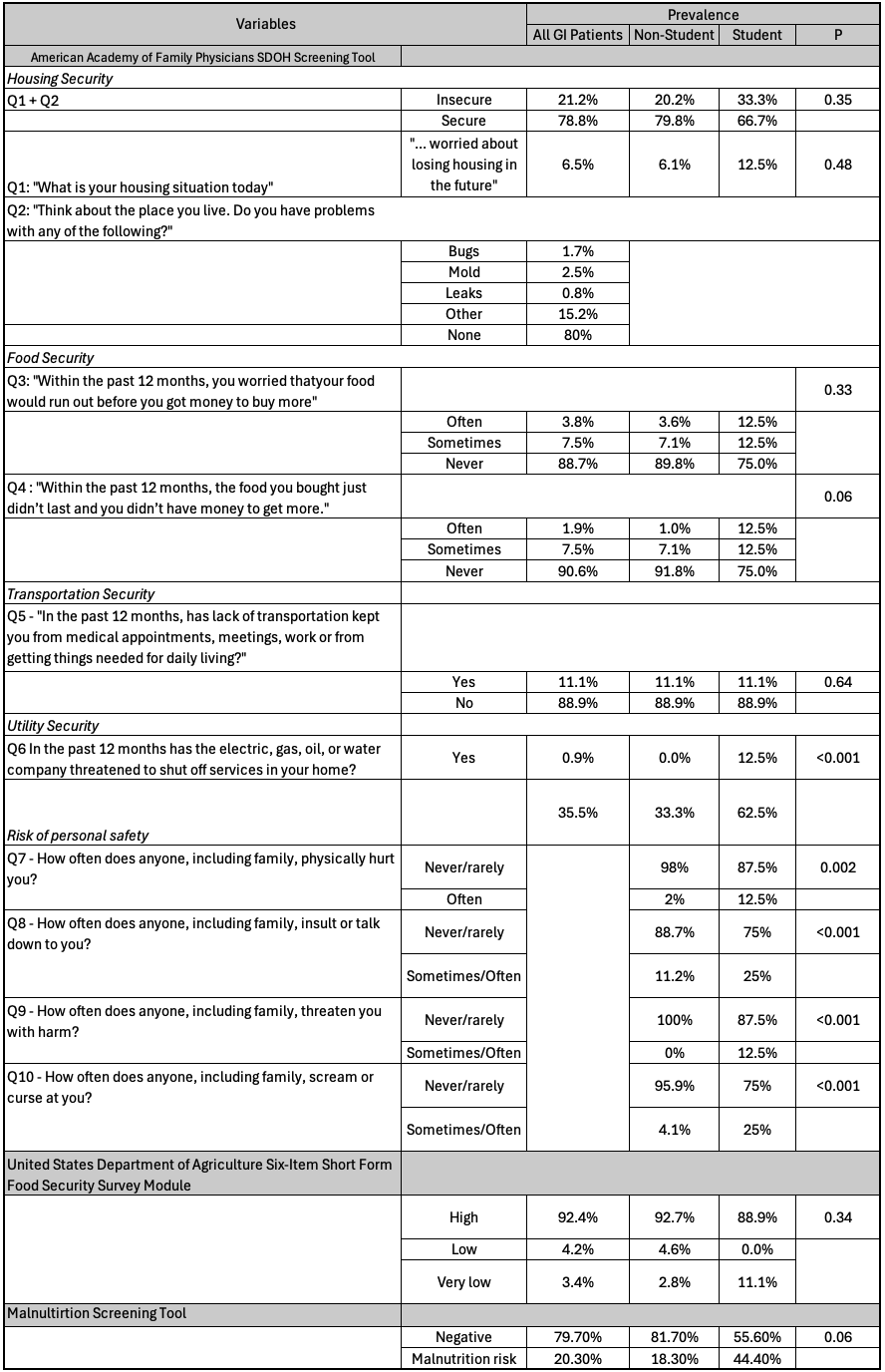
Figure: Patient survey responses to the American Academy of Family Physicians SDOH Screening tool, United States Department of Agriculture Six-Item Short Form Food Security Survey Module, and Malnutrition Screening Tool for all 118 GI patients and comparing non-students versus students.
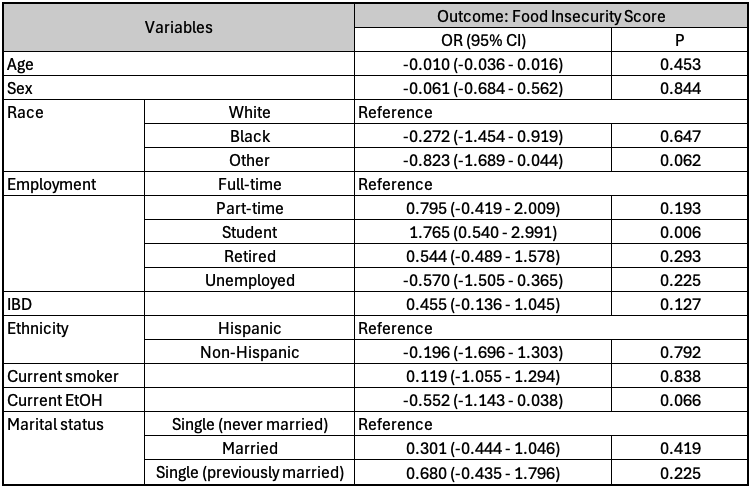
Figure: Multivariable linear regression analysis of the food insecurity score (a higher score indicates a greater risk of food insecurity) when adjusted for Age, Sex, Race, Employment, IBD, Ethnicity, Current Smoking Status, Current Alcohol (EtOH) use status, and Marital status.
Disclosures:
Mark Baniqued indicated no relevant financial relationships.
Rhett Harmon indicated no relevant financial relationships.
Alexandra Greb indicated no relevant financial relationships.
Bita Shahrvini indicated no relevant financial relationships.
Marc Kaneshiro indicated no relevant financial relationships.
Wendy Ho indicated no relevant financial relationships.
Guy Weiss: Guidepoint – Consultant. Regeneron – Consultant.
Jenny Sauk indicated no relevant financial relationships.
Nirupama Bonthala indicated no relevant financial relationships.
Jaden Nguyen indicated no relevant financial relationships.
Andrew Nguyen indicated no relevant financial relationships.
Jia Hui Hai indicated no relevant financial relationships.
Brendan Field indicated no relevant financial relationships.
Andrew Roney indicated no relevant financial relationships.
Janelle Smith indicated no relevant financial relationships.
Neha Shah: GI on Demand – Consultant.
Xiaoxiao Yin indicated no relevant financial relationships.
Folasade May indicated no relevant financial relationships.
Simon Beaven: Alnylam – Speakers Bureau.
Berkeley Limketkai indicated no relevant financial relationships.
Mark R. Baniqued, MD1, Rhett Harmon, MD1, Alexandra Greb, MD2, Bita Shahrvini, MD2, Marc Kaneshiro, MD2, Wendy Ho, MD2, Guy A. Weiss, MD3, Jenny Sauk, MD2, Nirupama Bonthala, MD2, Jaden Nguyen, 2, Andrew Nguyen, 2, Jia Hui Hai, 2, Brendan Field, 2, Andrew Roney, MD2, Janelle Smith, MS, RD, CEDRD2, Neha D. Shah, MPH, RD, CNSC, CHES4, Xiaoxiao Yin, 2, Folasade May, MD, PhD, MPhil2, Simon Beaven, MD, PhD5, Berkeley Limketkai, MD, PhD2. P4848 - University Students Are Vulnerable to Food Insecurity and Social Determinants of Health Among Patients With Gastrointestinal Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
