Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4840 - Minimally Invasive Solutions for Obesity: A Real-World Comparison of Endoscopic and Laparoscopic Sleeve Procedures
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Osman, MD, MSCI Candidate
Washington University School of Medicine in St. Louis
Ballwin, MO
Presenting Author(s)
Ali Osman, MD, MSCI Candidate1, Ahmed Dirweesh, MD2, Stuart K. Amateau, MD, PhD2
1Washington University School of Medicine in St. Louis, Ballwin, MO; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Endoscopic Sleeve Gastroplasty (ESG) and Laparoscopic Sleeve Gastrectomy (LSG) are both established interventions for the treatment of morbid obesity. While LSG remains more commonly performed, ESG has gained attention as a minimally invasive alternative. However, comparative real-world data on their safety and metabolic outcomes are limited.
Objective:
To compare the safety and metabolic efficacy of ESG and LSG using a propensity score–matched real-world cohort derived from a federated electronic health record database.
Methods: Adults (≥18 years) with morbid obesity (ICD-10: E66.01) who underwent ESG (HCPCS: C9784) or LSG (CPT: 43775) were identified from the TriNetX Global Collaborative Network. A 1:1 propensity score–matched analysis was conducted based on age, sex, race, and comorbidities. The primary safety endpoint was a composite of gastrointestinal bleeding, gastric ulcer with hemorrhage, perforation, postoperative infection, severe malnutrition, and vomiting. Metabolic efficacy outcomes included 1-year changes in BMI, weight, HbA1c, lipids, and blood pressure. Statistical analyses included risk differences, Kaplan-Meier survival analysis, and comparisons of mean changes in laboratory and vital sign parameters.
Results: After matching, 62 patients were included in each group. ESG was associated with a significantly lower incidence of the composite safety outcome compared to LSG (0% vs. < 17.2%, p = 0.001). However, due to TriNetX’s data obfuscation policy, the exact number of events in the LSG group is not disclosed when fewer than 10 events are present; thus, the reported 17.2% represents an upper-bound estimate
Event-free survival did not differ significantly between groups (p = 0.36). Both ESG and LSG led to meaningful improvements in BMI, HbA1c, and blood pressure. ESG showed greater reductions in total cholesterol (−7.1% vs. −2.2%) and LDL (−12.2% vs. −1.9%), while LSG resulted in more pronounced reductions in total body weight (−21.3% vs. −14.8%) and triglycerides (−24.8% vs. +9.9%)
Discussion: In this matched real-world cohort, ESG demonstrated superior short-term safety and comparable metabolic improvements to LSG, with distinct effects on lipid profiles. ESG may represent a safer, less invasive alternative to LSG for appropriately selected patients with morbid obesity.
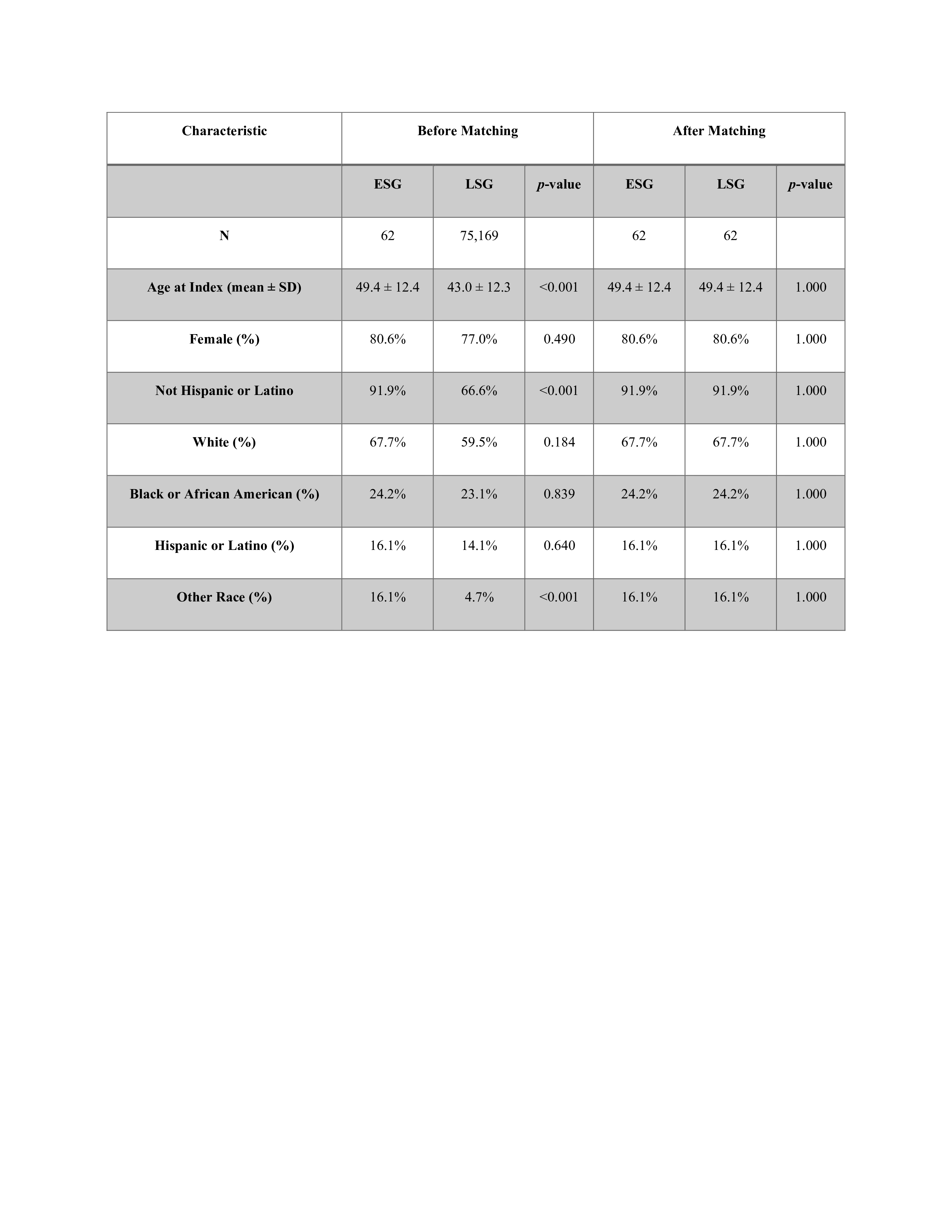
Figure: Table 1. Baseline characteristics of ESG and LSG groups before and after matching.

Figure: Fig-1 Comparison of Metabolic parameters Before and After ESG/LSG.
Disclosures:
Ali Osman indicated no relevant financial relationships.
Ahmed Dirweesh indicated no relevant financial relationships.
Stuart Amateau: BSC – Consultant. Cook – Consultant. Endo-Therapeutics – Consultant. Merit – Consultant. Olympus – Advisor or Review Panel Member, Consultant. Provation – Advisory Committee/Board Member. Steris – Consultant.
Ali Osman, MD, MSCI Candidate1, Ahmed Dirweesh, MD2, Stuart K. Amateau, MD, PhD2. P4840 - Minimally Invasive Solutions for Obesity: A Real-World Comparison of Endoscopic and Laparoscopic Sleeve Procedures, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Washington University School of Medicine in St. Louis, Ballwin, MO; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Endoscopic Sleeve Gastroplasty (ESG) and Laparoscopic Sleeve Gastrectomy (LSG) are both established interventions for the treatment of morbid obesity. While LSG remains more commonly performed, ESG has gained attention as a minimally invasive alternative. However, comparative real-world data on their safety and metabolic outcomes are limited.
Objective:
To compare the safety and metabolic efficacy of ESG and LSG using a propensity score–matched real-world cohort derived from a federated electronic health record database.
Methods: Adults (≥18 years) with morbid obesity (ICD-10: E66.01) who underwent ESG (HCPCS: C9784) or LSG (CPT: 43775) were identified from the TriNetX Global Collaborative Network. A 1:1 propensity score–matched analysis was conducted based on age, sex, race, and comorbidities. The primary safety endpoint was a composite of gastrointestinal bleeding, gastric ulcer with hemorrhage, perforation, postoperative infection, severe malnutrition, and vomiting. Metabolic efficacy outcomes included 1-year changes in BMI, weight, HbA1c, lipids, and blood pressure. Statistical analyses included risk differences, Kaplan-Meier survival analysis, and comparisons of mean changes in laboratory and vital sign parameters.
Results: After matching, 62 patients were included in each group. ESG was associated with a significantly lower incidence of the composite safety outcome compared to LSG (0% vs. < 17.2%, p = 0.001). However, due to TriNetX’s data obfuscation policy, the exact number of events in the LSG group is not disclosed when fewer than 10 events are present; thus, the reported 17.2% represents an upper-bound estimate
Event-free survival did not differ significantly between groups (p = 0.36). Both ESG and LSG led to meaningful improvements in BMI, HbA1c, and blood pressure. ESG showed greater reductions in total cholesterol (−7.1% vs. −2.2%) and LDL (−12.2% vs. −1.9%), while LSG resulted in more pronounced reductions in total body weight (−21.3% vs. −14.8%) and triglycerides (−24.8% vs. +9.9%)
Discussion: In this matched real-world cohort, ESG demonstrated superior short-term safety and comparable metabolic improvements to LSG, with distinct effects on lipid profiles. ESG may represent a safer, less invasive alternative to LSG for appropriately selected patients with morbid obesity.
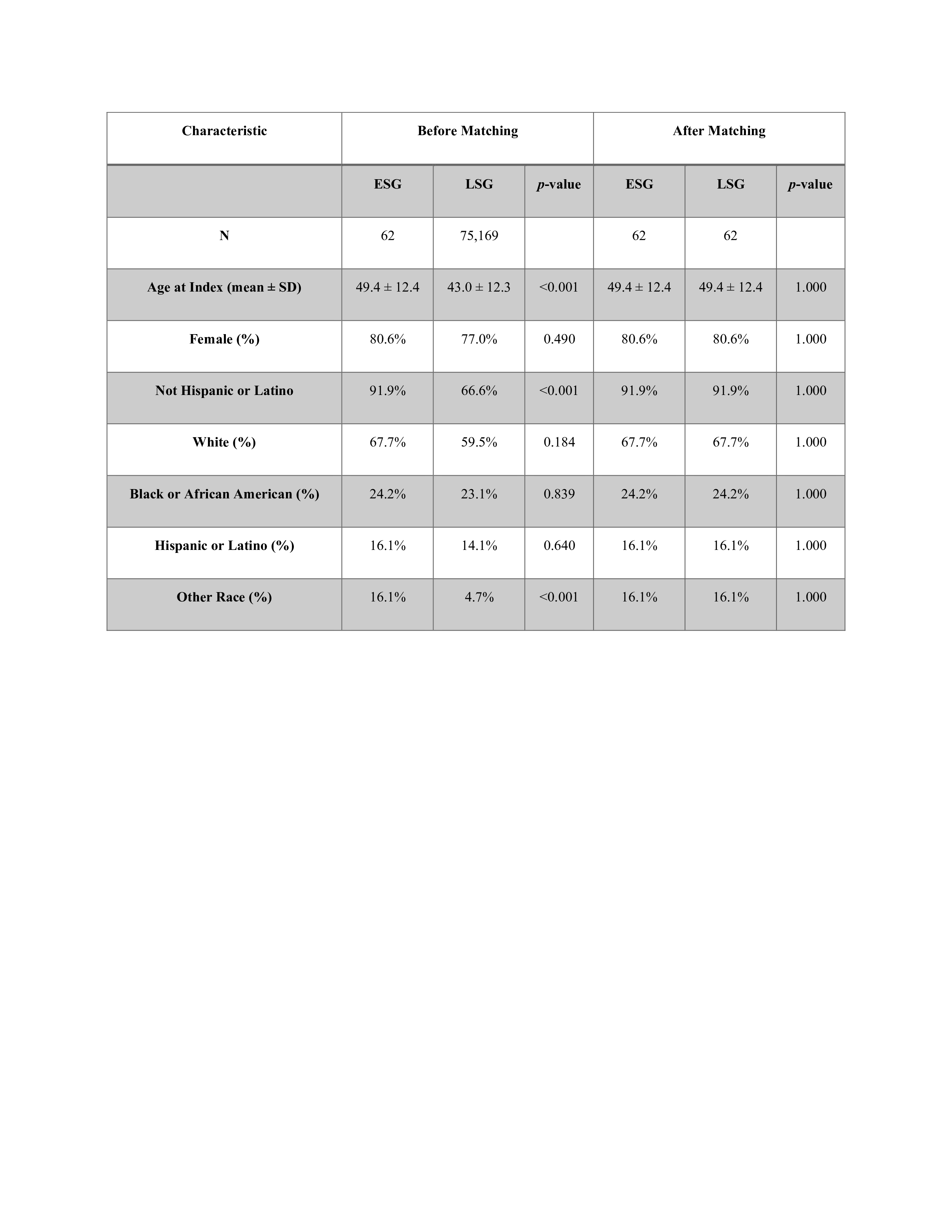
Figure: Table 1. Baseline characteristics of ESG and LSG groups before and after matching.

Figure: Fig-1 Comparison of Metabolic parameters Before and After ESG/LSG.
Disclosures:
Ali Osman indicated no relevant financial relationships.
Ahmed Dirweesh indicated no relevant financial relationships.
Stuart Amateau: BSC – Consultant. Cook – Consultant. Endo-Therapeutics – Consultant. Merit – Consultant. Olympus – Advisor or Review Panel Member, Consultant. Provation – Advisory Committee/Board Member. Steris – Consultant.
Ali Osman, MD, MSCI Candidate1, Ahmed Dirweesh, MD2, Stuart K. Amateau, MD, PhD2. P4840 - Minimally Invasive Solutions for Obesity: A Real-World Comparison of Endoscopic and Laparoscopic Sleeve Procedures, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
