Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4825 - Protein-Energy Malnutrition Is an Independent Predictor of Mortality in Variceal Upper Gastrointestinal Bleeding: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Angelin Raju, MD (she/her/hers)
Texas Health Resources HEB/ Denton
Bedford, TX
Presenting Author(s)
Angelin Raju, MD1, Anish Jomy, MBBS2, Arthur CHIDI. Igbo, MD, MPH3, Anunaya Aashish, MD1
1Texas Health Resources HEB/ Denton, Bedford, TX; 2Methodist Health System, Richardson, TX; 3Texas Health Resources HEB/Denton Internal Medicine Program, Lewisville, TX
Introduction: Protein-energy malnutrition (PEM) is a common comorbidity in patients with cirrhosis and is a known contributor to adverse clinical outcomes. However, its specific impact on outcomes in the setting of variceal upper gastrointestinal bleeding (VUGIB) remains understudied. This study investigates the association between PEM and in-hospital outcomes, including mortality, resource utilization, and complications in patients hospitalized with VUGIB.
Methods: A retrospective cohort study was conducted using the 2018-2022 National Inpatient Sample (NIS). Adults with a diagnosis of VUGIB were identified using ICD-10 codes. PEM was categorized as mild/moderate, severe, or unspecified. Survey-weighted multivariable logistic regression was performed to identify predictors of in-hospital mortality, adjusting for demographics, comorbidities (Elixhauser index), and clinical characteristics. Secondary outcomes included hospitalization charges, length of stay (LOS), complications and endoscopic intervention rates.
Results: Among 48,665 weighted hospitalizations for VUGIB, approximately 4,300 (8.8%) had concurrent PEM. Of these, 1,465 had mild/moderate PEM, 1,885 had severe PEM and 980 had unspecified PEM. PEM independently increased odds of in-hospital mortality (Adjusted Odds Ratio [AOR] 1.45, p=0.012), acute kidney injury (AOR 1.36, p=0.001), septic shock (AOR 2.14, p=0.005) and hospitalization charges (+$55,600, p< 0.001). Severe PEM conferred >4-fold increased odds of septic shock (OR 4.03, p< 0.001) and >2.5-fold odds of mortality (OR 2.59, p< 0.001). Unspecified PEM was also associated with increased mortality (OR 1.85, p=0.017). PEM was not significantly associated with hemorrhagic shock, LOS, race or likelihood of undergoing diagnostic/interventional endoscopy. Higher Elixhauser score (AOR 1.18, p< 0.001), weekend admission (AOR 1.25, p=0.034), and Self pay patients (AOR 1.8, p=0.002) were also associated with increased mortality. Female sex was protective against both mortality (AOR 0.68, p< 0.001) and AKI (AOR 0.74, p< 0.001).
Discussion: PEM is independently associated with increased in-hospital mortality, acute kidney injury, septic shock, and significantly higher hospitalization charges, in patients hospitalized with VUGIB. Severe PEM confers a particularly high risk for septic shock and mortality. These findings underscore the prognostic impact of nutritional status in VUGIB and support early identification and management of PEM to improve outcomes and reduce healthcare burden.
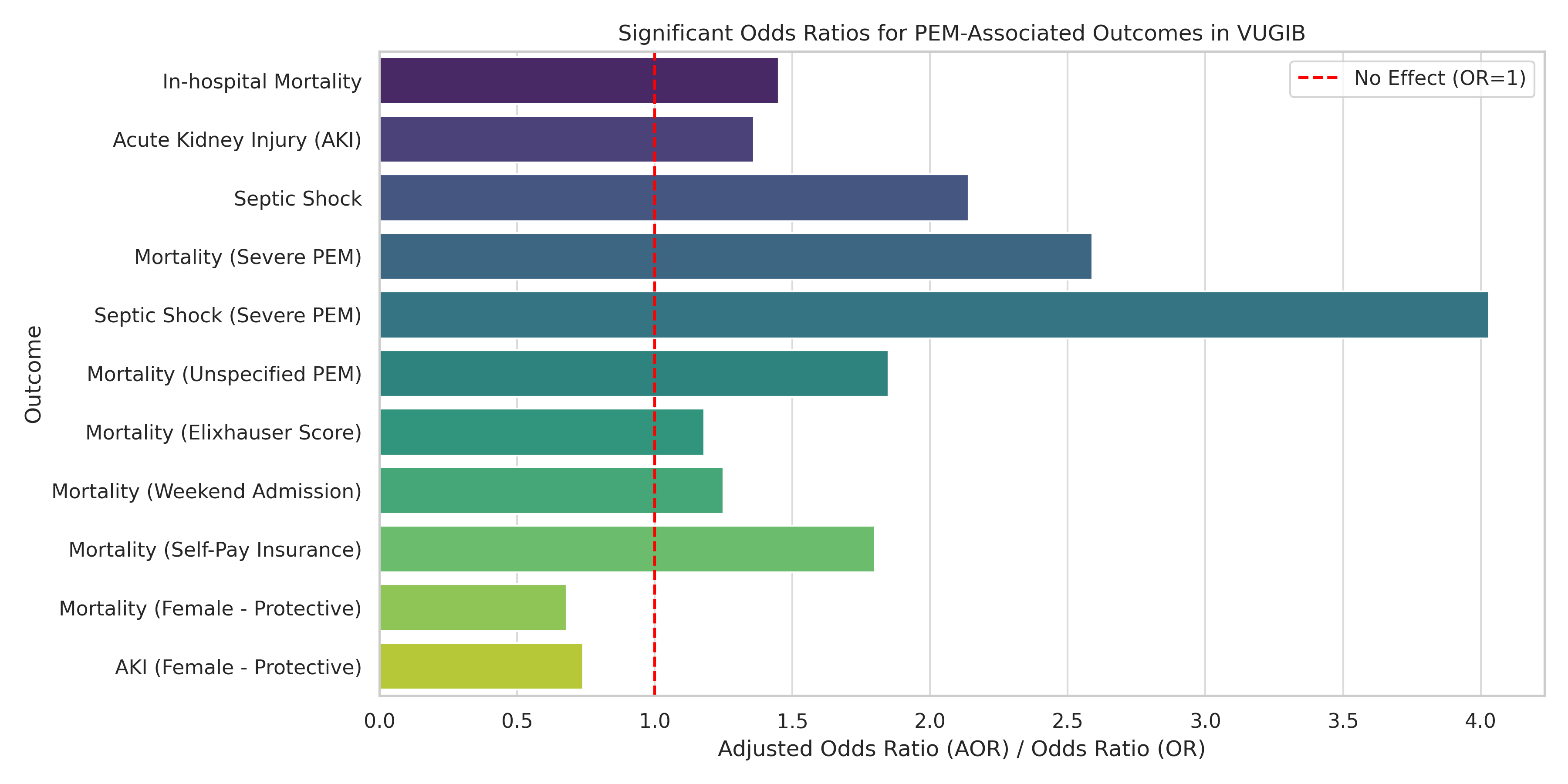
Figure: Significant Odds Ratios for PEM-Associated Outcomes in VUGIB
Disclosures:
Angelin Raju indicated no relevant financial relationships.
Anish Jomy indicated no relevant financial relationships.
Arthur Igbo indicated no relevant financial relationships.
Anunaya Aashish indicated no relevant financial relationships.
Angelin Raju, MD1, Anish Jomy, MBBS2, Arthur CHIDI. Igbo, MD, MPH3, Anunaya Aashish, MD1. P4825 - Protein-Energy Malnutrition Is an Independent Predictor of Mortality in Variceal Upper Gastrointestinal Bleeding: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Texas Health Resources HEB/ Denton, Bedford, TX; 2Methodist Health System, Richardson, TX; 3Texas Health Resources HEB/Denton Internal Medicine Program, Lewisville, TX
Introduction: Protein-energy malnutrition (PEM) is a common comorbidity in patients with cirrhosis and is a known contributor to adverse clinical outcomes. However, its specific impact on outcomes in the setting of variceal upper gastrointestinal bleeding (VUGIB) remains understudied. This study investigates the association between PEM and in-hospital outcomes, including mortality, resource utilization, and complications in patients hospitalized with VUGIB.
Methods: A retrospective cohort study was conducted using the 2018-2022 National Inpatient Sample (NIS). Adults with a diagnosis of VUGIB were identified using ICD-10 codes. PEM was categorized as mild/moderate, severe, or unspecified. Survey-weighted multivariable logistic regression was performed to identify predictors of in-hospital mortality, adjusting for demographics, comorbidities (Elixhauser index), and clinical characteristics. Secondary outcomes included hospitalization charges, length of stay (LOS), complications and endoscopic intervention rates.
Results: Among 48,665 weighted hospitalizations for VUGIB, approximately 4,300 (8.8%) had concurrent PEM. Of these, 1,465 had mild/moderate PEM, 1,885 had severe PEM and 980 had unspecified PEM. PEM independently increased odds of in-hospital mortality (Adjusted Odds Ratio [AOR] 1.45, p=0.012), acute kidney injury (AOR 1.36, p=0.001), septic shock (AOR 2.14, p=0.005) and hospitalization charges (+$55,600, p< 0.001). Severe PEM conferred >4-fold increased odds of septic shock (OR 4.03, p< 0.001) and >2.5-fold odds of mortality (OR 2.59, p< 0.001). Unspecified PEM was also associated with increased mortality (OR 1.85, p=0.017). PEM was not significantly associated with hemorrhagic shock, LOS, race or likelihood of undergoing diagnostic/interventional endoscopy. Higher Elixhauser score (AOR 1.18, p< 0.001), weekend admission (AOR 1.25, p=0.034), and Self pay patients (AOR 1.8, p=0.002) were also associated with increased mortality. Female sex was protective against both mortality (AOR 0.68, p< 0.001) and AKI (AOR 0.74, p< 0.001).
Discussion: PEM is independently associated with increased in-hospital mortality, acute kidney injury, septic shock, and significantly higher hospitalization charges, in patients hospitalized with VUGIB. Severe PEM confers a particularly high risk for septic shock and mortality. These findings underscore the prognostic impact of nutritional status in VUGIB and support early identification and management of PEM to improve outcomes and reduce healthcare burden.
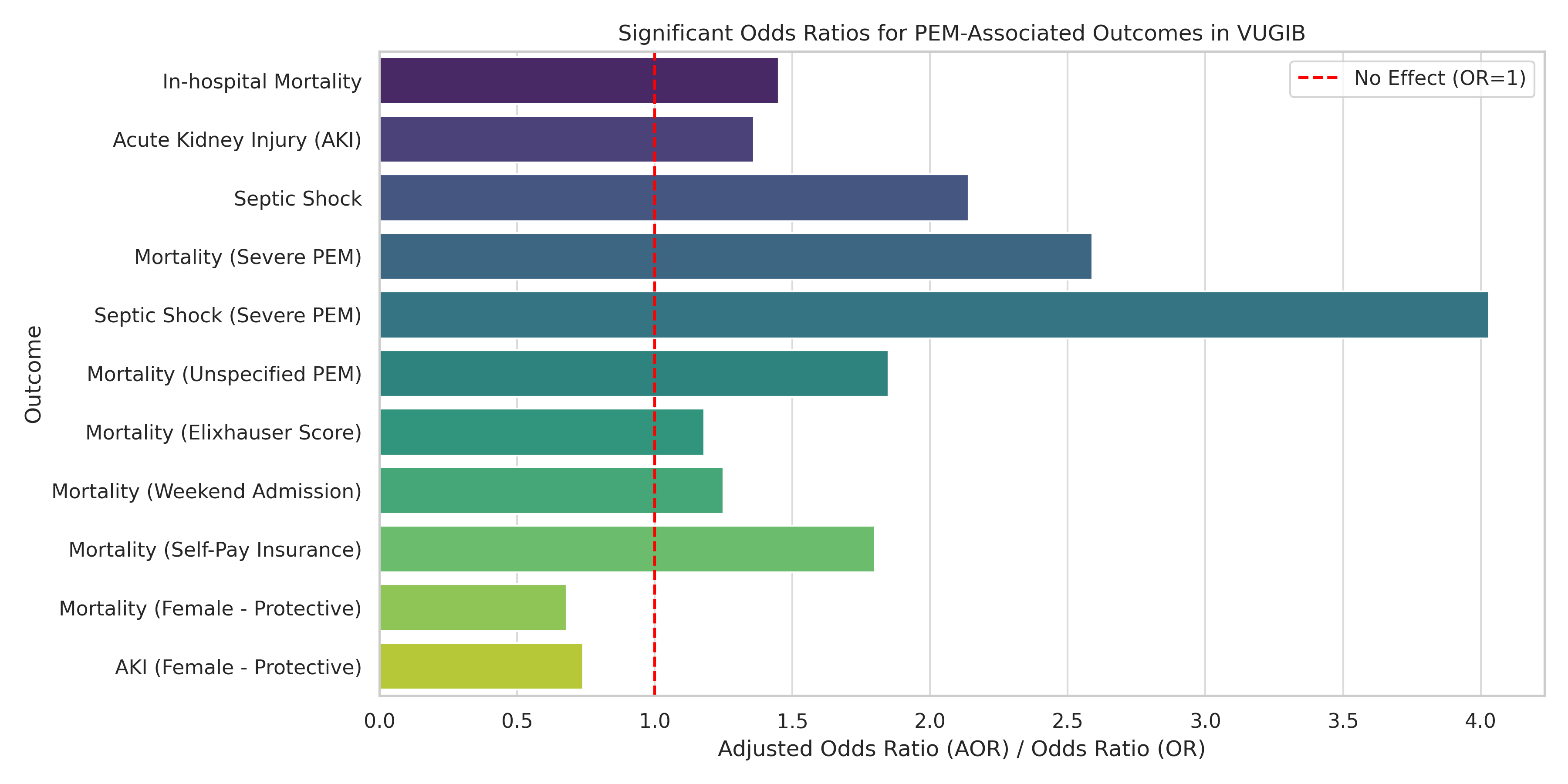
Figure: Significant Odds Ratios for PEM-Associated Outcomes in VUGIB
Disclosures:
Angelin Raju indicated no relevant financial relationships.
Anish Jomy indicated no relevant financial relationships.
Arthur Igbo indicated no relevant financial relationships.
Anunaya Aashish indicated no relevant financial relationships.
Angelin Raju, MD1, Anish Jomy, MBBS2, Arthur CHIDI. Igbo, MD, MPH3, Anunaya Aashish, MD1. P4825 - Protein-Energy Malnutrition Is an Independent Predictor of Mortality in Variceal Upper Gastrointestinal Bleeding: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
