Tuesday Poster Session
Category: Diet, Nutrition, and Obesity
P4820 - Obesity and Gastroenterology: National Trends in Mortality and Demographics Among US Adults (1999–2022)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamed A. Ebrahim, MD (he/him/his)
Ascension Saint Joseph Hospital
Chicago, IL
Presenting Author(s)
Mohamed A. Ebrahim, MD1, Mohammad Adam, MD, MSc2, Kanwal Tagar, MD1, Bilal Makhdoom, MD3, Muhammad Sohaib Alvi, MBBS, MD1, Marwan Ahmed, MD4, Alizay Khan, MD1, Mogahid Farah, MD1
1Ascension Saint Joseph Hospital, Chicago, IL; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL; 4Parkview Medical Center, Pueblo, CO
Introduction: Obesity is a global health epidemic, driving the prevalence of chronic diseases such as diabetes, cardiovascular disorders, and cancer. Its impact on the gastrointestinal (GI) system is profound, contributing to conditions like metabolic dysfunction-associated steatotic liver disease (MASLD), gastroesophageal reflux disease (GERD), and colorectal cancer. The rising rates of obesity present escalating challenges for healthcare systems.
Methods: We analyzed mortality linked to obesity and gastrointestinal diseases in adults ≥25 years using CDC-WONDER data from 1999–2022. Obesity was identified using ICD-10 codes E66.0–E66.2, E66.8, and E66.9; gastrointestinal diseases using K00–K92. Age-adjusted mortality rates (AAMR) were based on the 2000 U.S. standard population. Temporal trends were assessed via Joinpoint regression. Mortality was stratified by age, race/ethnicity, gender, urbanization, and geographic region.
Results: Between 1999 and 2022, there were 61,927,317 deaths in the US, with 4,900,955 (7.91%) GI-related and 831,822 (1.34%) obesity-related. A total of 67,042 deaths were linked to both obesity and GI diseases as underlying causes, with an overall age-adjusted mortality rate (AAMR) of 1.22. Age stratification showed the lowest mortality rate in young adults (25–44) at 0.50, rising to 1.58 in middle-aged adults (45–64), and peaking at 2.26 in those aged 65 and older. Gender analysis showed females had an AAMR of 1.20, while males had a slightly higher rate of 1.23. Racial and ethnic disparities were evident: non-Hispanic White individuals had the highest AAMR at 1.29, followed by non-Hispanic Black individuals at 1.25, and Hispanic/Latino individuals at 1.13. Rural areas had a higher AAMR (1.42) compared to urban areas (1.06). Regionally, the West had the highest AAMR at 1.54, followed by the Midwest (1.24), South (1.18), and Northeast (0.90). States with the highest AAMR included Vermont (2.8), Oklahoma (2.4), Wyoming (1.96), Minnesota (1.83), and Colorado (1.83).
Discussion: Males, Non-Hispanic Whites, and the elderly exhibited higher mortality rates, with rural areas having higher AAMR than urban areas. Regionally, the West recorded the highest mortality rates, with notable state-level variations, including Vermont and Oklahoma leading. These findings highlight the growing impact of obesity on GI-related mortality, emphasizing the need for targeted prevention and intervention strategies in high-risk populations.
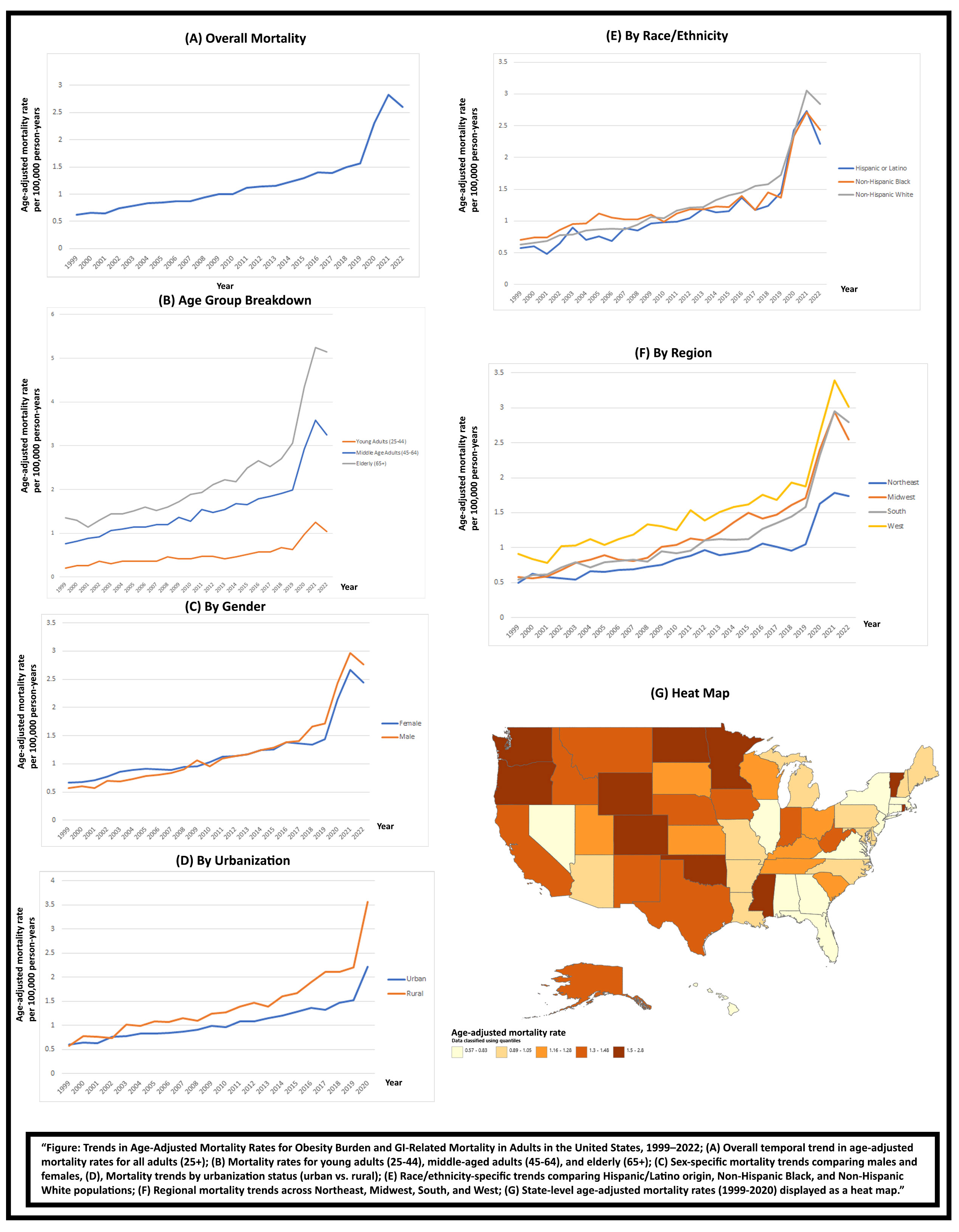
Figure: Trends in Age-Adjusted Mortality Rates for Obesity Burden and GI-Related Mortality in Adults in the United States
Disclosures:
Mohamed Ebrahim indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Kanwal Tagar indicated no relevant financial relationships.
Bilal Makhdoom indicated no relevant financial relationships.
Muhammad Sohaib Alvi indicated no relevant financial relationships.
Marwan Ahmed indicated no relevant financial relationships.
Alizay Khan indicated no relevant financial relationships.
Mogahid Farah indicated no relevant financial relationships.
Mohamed A. Ebrahim, MD1, Mohammad Adam, MD, MSc2, Kanwal Tagar, MD1, Bilal Makhdoom, MD3, Muhammad Sohaib Alvi, MBBS, MD1, Marwan Ahmed, MD4, Alizay Khan, MD1, Mogahid Farah, MD1. P4820 - Obesity and Gastroenterology: National Trends in Mortality and Demographics Among US Adults (1999–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Ascension Saint Joseph Hospital, Chicago, IL; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL; 4Parkview Medical Center, Pueblo, CO
Introduction: Obesity is a global health epidemic, driving the prevalence of chronic diseases such as diabetes, cardiovascular disorders, and cancer. Its impact on the gastrointestinal (GI) system is profound, contributing to conditions like metabolic dysfunction-associated steatotic liver disease (MASLD), gastroesophageal reflux disease (GERD), and colorectal cancer. The rising rates of obesity present escalating challenges for healthcare systems.
Methods: We analyzed mortality linked to obesity and gastrointestinal diseases in adults ≥25 years using CDC-WONDER data from 1999–2022. Obesity was identified using ICD-10 codes E66.0–E66.2, E66.8, and E66.9; gastrointestinal diseases using K00–K92. Age-adjusted mortality rates (AAMR) were based on the 2000 U.S. standard population. Temporal trends were assessed via Joinpoint regression. Mortality was stratified by age, race/ethnicity, gender, urbanization, and geographic region.
Results: Between 1999 and 2022, there were 61,927,317 deaths in the US, with 4,900,955 (7.91%) GI-related and 831,822 (1.34%) obesity-related. A total of 67,042 deaths were linked to both obesity and GI diseases as underlying causes, with an overall age-adjusted mortality rate (AAMR) of 1.22. Age stratification showed the lowest mortality rate in young adults (25–44) at 0.50, rising to 1.58 in middle-aged adults (45–64), and peaking at 2.26 in those aged 65 and older. Gender analysis showed females had an AAMR of 1.20, while males had a slightly higher rate of 1.23. Racial and ethnic disparities were evident: non-Hispanic White individuals had the highest AAMR at 1.29, followed by non-Hispanic Black individuals at 1.25, and Hispanic/Latino individuals at 1.13. Rural areas had a higher AAMR (1.42) compared to urban areas (1.06). Regionally, the West had the highest AAMR at 1.54, followed by the Midwest (1.24), South (1.18), and Northeast (0.90). States with the highest AAMR included Vermont (2.8), Oklahoma (2.4), Wyoming (1.96), Minnesota (1.83), and Colorado (1.83).
Discussion: Males, Non-Hispanic Whites, and the elderly exhibited higher mortality rates, with rural areas having higher AAMR than urban areas. Regionally, the West recorded the highest mortality rates, with notable state-level variations, including Vermont and Oklahoma leading. These findings highlight the growing impact of obesity on GI-related mortality, emphasizing the need for targeted prevention and intervention strategies in high-risk populations.
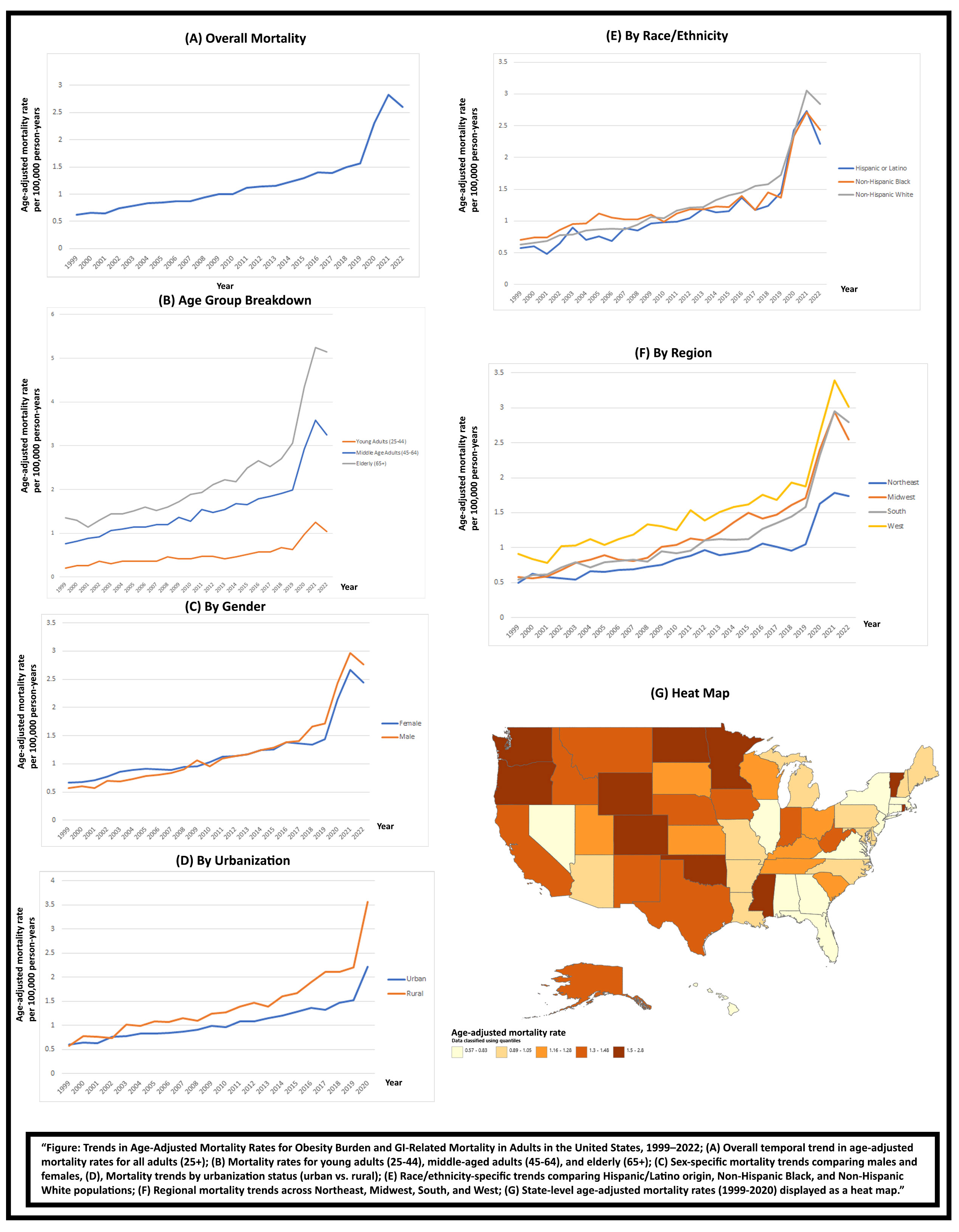
Figure: Trends in Age-Adjusted Mortality Rates for Obesity Burden and GI-Related Mortality in Adults in the United States
Disclosures:
Mohamed Ebrahim indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Kanwal Tagar indicated no relevant financial relationships.
Bilal Makhdoom indicated no relevant financial relationships.
Muhammad Sohaib Alvi indicated no relevant financial relationships.
Marwan Ahmed indicated no relevant financial relationships.
Alizay Khan indicated no relevant financial relationships.
Mogahid Farah indicated no relevant financial relationships.
Mohamed A. Ebrahim, MD1, Mohammad Adam, MD, MSc2, Kanwal Tagar, MD1, Bilal Makhdoom, MD3, Muhammad Sohaib Alvi, MBBS, MD1, Marwan Ahmed, MD4, Alizay Khan, MD1, Mogahid Farah, MD1. P4820 - Obesity and Gastroenterology: National Trends in Mortality and Demographics Among US Adults (1999–2022), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
