Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4812 - Endoscopic Management of Appendiceal Orifice Polyps: A 5-Case Series Supporting First-Line Conservative Approach
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mahmoud Barbarawi, MD (he/him/his)
DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine
McAllen, TX
Presenting Author(s)
Award: ACG Presidential Poster Award
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Prince Shah-Riar, MD3, Asif Zamir, MD, FACG4
1DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine, McAllen, TX; 2DHR Health, McAllen, TX; 3DHR Health, Edinburg, Tx, McAllen, TX; 4DHR Health Gastroenterology, Edinburg, TX
Introduction: Appendiceal orifice polyps pose a rare but challenging clinical entity (0.08–0.4% of colonoscopies) with limited evidence-based management guidelines. Traditionally, surgical referral has been favored due to risks of incomplete resection, retained neoplastic tissue, and post-polypectomy appendicitis. Recent studies report endoscopic feasibility with an ~80% success rate and 12% one-year recurrence but with a notable risk of appendicitis, challenging this paradigm. However, clinical guidelines remain limited. We present a 5-case series supporting traditional endoscopic techniques as effective 1st-line therapy.
Case Description/
Methods: We retrospectively reviewed 5 cases of appendiceal orifice polyps identified during screening colonoscopy (2019–2021) at a single tertiary center. Mean patient age was 62 years (range 50–79); 60% male; 80% Hispanic. Mean polyp size was 3.8 cm. All procedures were performed by an experienced endoscopist using high-definition colonoscopy. Submucosal injection (ORISE or Eleview) was followed by hot snare polypectomy, with piecemeal resection for lesions >2 cm and routine prophylactic clipping, and elective prophylactic appendectomy was recommended. Surveillance colonoscopy occurred at 3–12 months.
Results: Endoscopic resection succeeded in 4 of 5 cases (80%).
Case 1: 6 cm tubular adenoma, piecemeal resection; developed interval appendicitis; appendectomy showed residual adenoma.
Case 2: 3 cm sessile serrated adenoma, resected with no recurrence.
Case 3: 2 cm pedunculated tubular adenoma, resected with long-term negative surveillance.
Case 4: 4 cm tubulovillous adenoma, complete resection, no recurrence.
Case 5: 4 cm sessile serrated adenoma, inadequate lift; referred for appendectomy.
Histology revealed 2 tubular adenomas, 2 sessile serrated adenomas, and 1 tubulovillous adenoma; no high-grade dysplasia or malignancy. Mean follow-up was 18 months; no local recurrence occurred in successful endoscopic cases. No intraprocedural complications occurred; one delayed appendicitis was noted.
Discussion: Endoscopic resection is a safe and effective 1st-line option for appendiceal orifice polyps, achieving 80% success and 0% recurrence with proper technique. Inability to achieve adequate lift remains a contraindication. We propose an algorithm prioritizing endoscopic resection when elevation and complete margins are feasible, reserving surgery for complex/non-lifting lesions. This approach minimizes morbidity, warranting further validation through prospective studies.
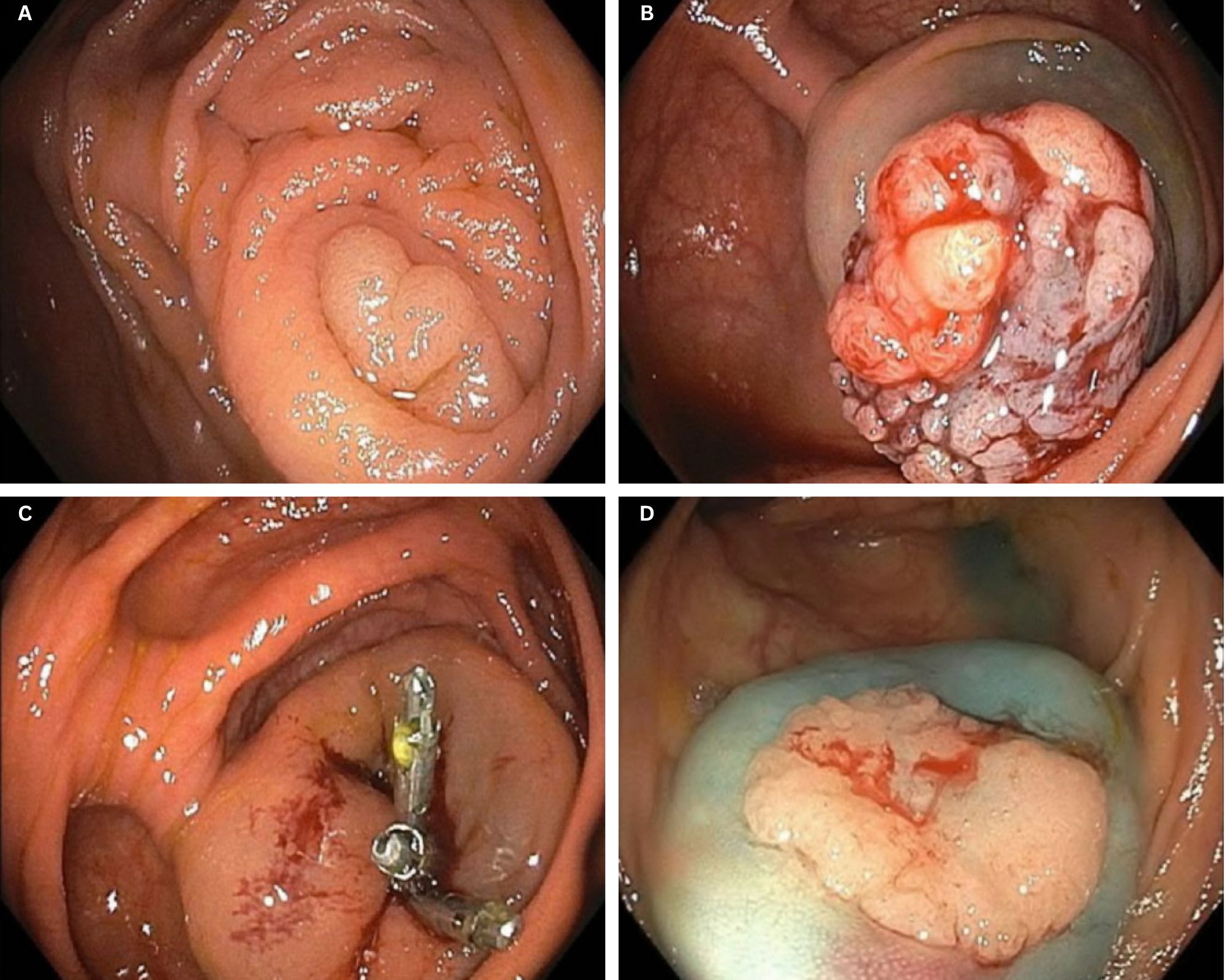
Figure: Figure A: Case 1 – Polyp arising from the appendiceal orifice.
Figure B: Case 1 – Polyp elevating from the orifice after submucosal injection with Eleview.
Figure C: Case 1 – Post-polypectomy site at appendiceal orifice with prophylactic endoclips in place.
Figure D: Case 2 – Sessile polyp at the appendiceal orifice.
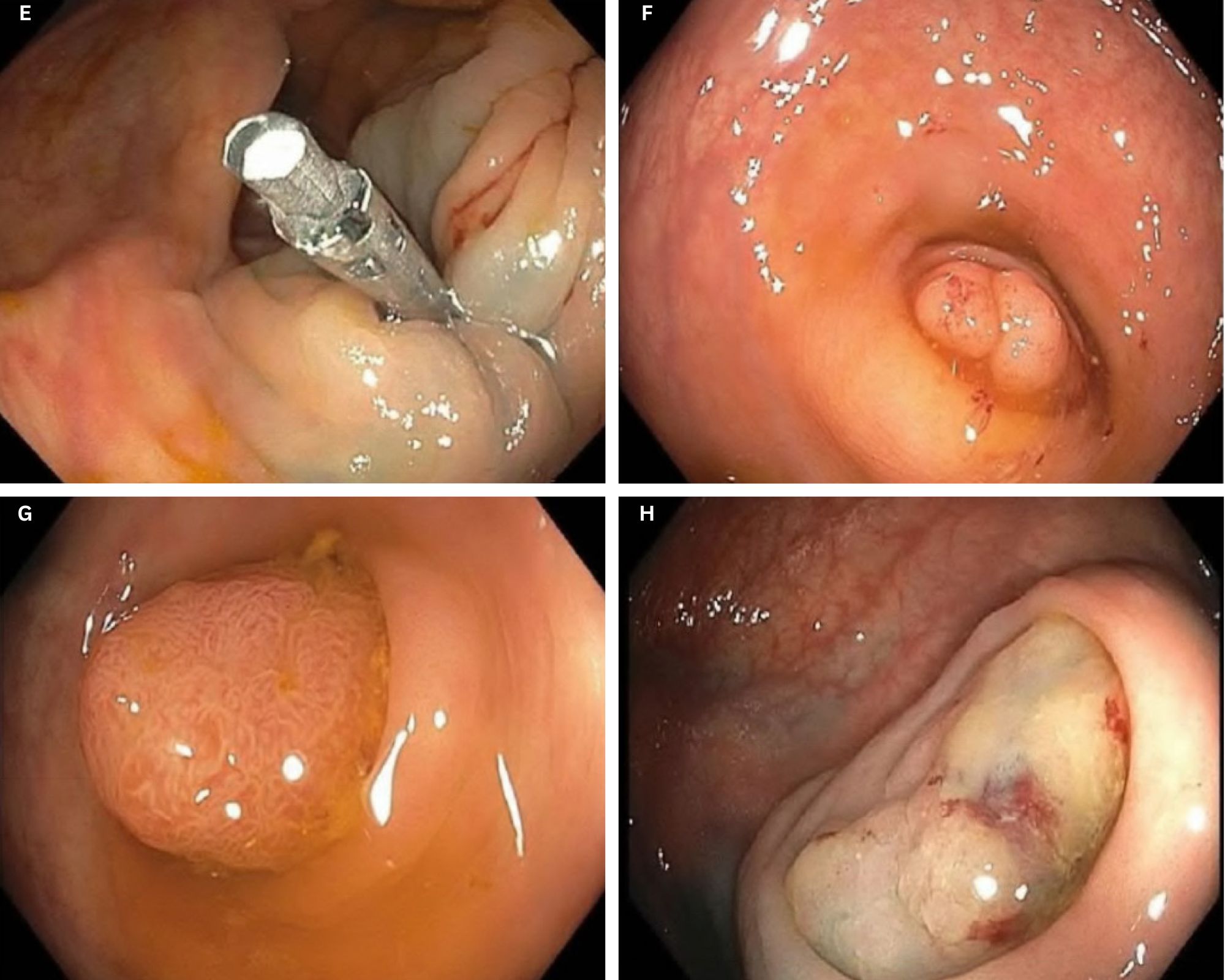
Figure: Figure E: Case 2 – Post-polypectomy site at appendiceal orifice with endoclips in place.
Figure F: Case 3 – Polyp arising from the appendiceal orifice.
Figure G: Case 4 – Sessile polyp at the appendiceal orifice.
Figure H: Case 5 – Flat polyp at the appendiceal orifice.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Rishika Trivedi indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Prince Shah-Riar, MD3, Asif Zamir, MD, FACG4. P4812 - Endoscopic Management of Appendiceal Orifice Polyps: A 5-Case Series Supporting First-Line Conservative Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Prince Shah-Riar, MD3, Asif Zamir, MD, FACG4
1DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine, McAllen, TX; 2DHR Health, McAllen, TX; 3DHR Health, Edinburg, Tx, McAllen, TX; 4DHR Health Gastroenterology, Edinburg, TX
Introduction: Appendiceal orifice polyps pose a rare but challenging clinical entity (0.08–0.4% of colonoscopies) with limited evidence-based management guidelines. Traditionally, surgical referral has been favored due to risks of incomplete resection, retained neoplastic tissue, and post-polypectomy appendicitis. Recent studies report endoscopic feasibility with an ~80% success rate and 12% one-year recurrence but with a notable risk of appendicitis, challenging this paradigm. However, clinical guidelines remain limited. We present a 5-case series supporting traditional endoscopic techniques as effective 1st-line therapy.
Case Description/
Methods: We retrospectively reviewed 5 cases of appendiceal orifice polyps identified during screening colonoscopy (2019–2021) at a single tertiary center. Mean patient age was 62 years (range 50–79); 60% male; 80% Hispanic. Mean polyp size was 3.8 cm. All procedures were performed by an experienced endoscopist using high-definition colonoscopy. Submucosal injection (ORISE or Eleview) was followed by hot snare polypectomy, with piecemeal resection for lesions >2 cm and routine prophylactic clipping, and elective prophylactic appendectomy was recommended. Surveillance colonoscopy occurred at 3–12 months.
Results: Endoscopic resection succeeded in 4 of 5 cases (80%).
Case 1: 6 cm tubular adenoma, piecemeal resection; developed interval appendicitis; appendectomy showed residual adenoma.
Case 2: 3 cm sessile serrated adenoma, resected with no recurrence.
Case 3: 2 cm pedunculated tubular adenoma, resected with long-term negative surveillance.
Case 4: 4 cm tubulovillous adenoma, complete resection, no recurrence.
Case 5: 4 cm sessile serrated adenoma, inadequate lift; referred for appendectomy.
Histology revealed 2 tubular adenomas, 2 sessile serrated adenomas, and 1 tubulovillous adenoma; no high-grade dysplasia or malignancy. Mean follow-up was 18 months; no local recurrence occurred in successful endoscopic cases. No intraprocedural complications occurred; one delayed appendicitis was noted.
Discussion: Endoscopic resection is a safe and effective 1st-line option for appendiceal orifice polyps, achieving 80% success and 0% recurrence with proper technique. Inability to achieve adequate lift remains a contraindication. We propose an algorithm prioritizing endoscopic resection when elevation and complete margins are feasible, reserving surgery for complex/non-lifting lesions. This approach minimizes morbidity, warranting further validation through prospective studies.
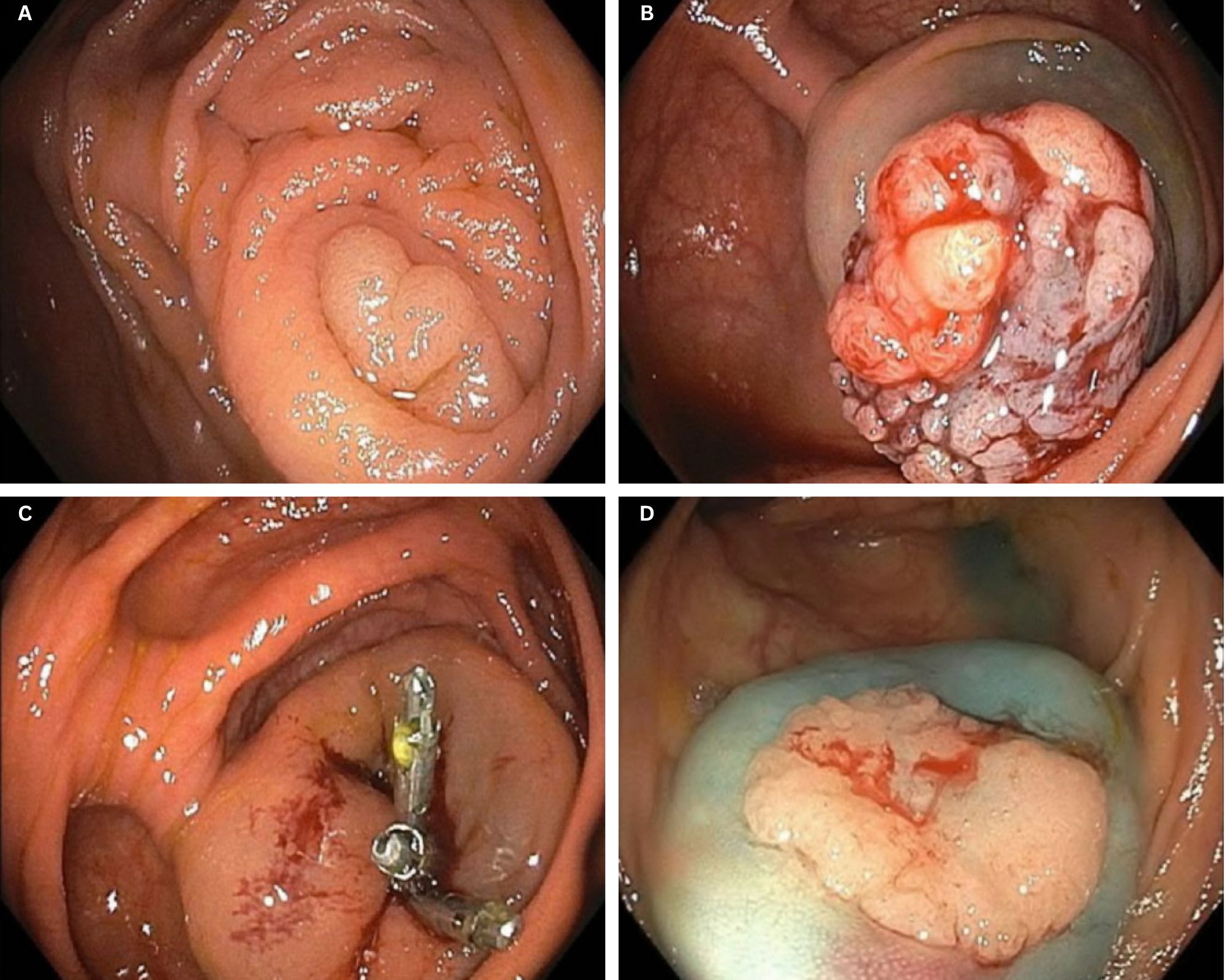
Figure: Figure A: Case 1 – Polyp arising from the appendiceal orifice.
Figure B: Case 1 – Polyp elevating from the orifice after submucosal injection with Eleview.
Figure C: Case 1 – Post-polypectomy site at appendiceal orifice with prophylactic endoclips in place.
Figure D: Case 2 – Sessile polyp at the appendiceal orifice.
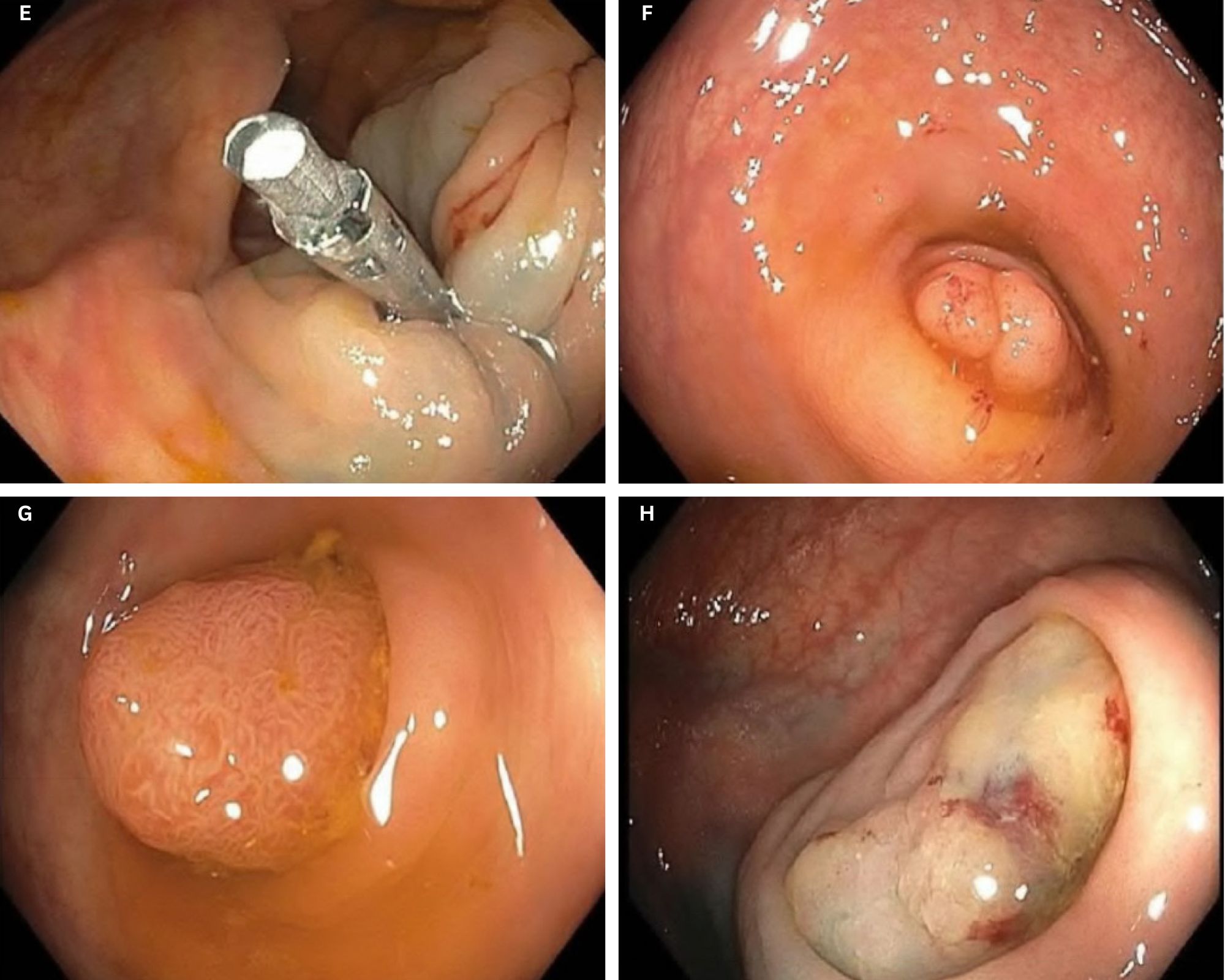
Figure: Figure E: Case 2 – Post-polypectomy site at appendiceal orifice with endoclips in place.
Figure F: Case 3 – Polyp arising from the appendiceal orifice.
Figure G: Case 4 – Sessile polyp at the appendiceal orifice.
Figure H: Case 5 – Flat polyp at the appendiceal orifice.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Rishika Trivedi indicated no relevant financial relationships.
Prince Shah-Riar indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Rishika Trivedi, MD2, Prince Shah-Riar, MD3, Asif Zamir, MD, FACG4. P4812 - Endoscopic Management of Appendiceal Orifice Polyps: A 5-Case Series Supporting First-Line Conservative Approach, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

