Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4811 - Segment Metachronous Neoplasia: A Novel Approach to Measuring Endoscopist Incomplete Resection Rate
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LE
Lauren Eichenwald, MD (she/her/hers)
Dartmouth Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Lauren Eichenwald, MD1, Obaida Dairi, DO1, Joseph C. Anderson, MD2, Campbell Levy, MD1, Steven P. Bensen, MD1, Heiko Pohl, MD, MS1
1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Dartmouth College, Hanover, NH
Introduction: Incomplete polyp resection is a key contributor to post-colonoscopy colorectal cancer, but accurately measuring an endoscopist’s incomplete resection rate (IRR) remains challenging. We assessed whether segment metachronous neoplasia (SMN) can estimate IRR for endoscopists. If valid, results should mirror marginal biopsies of the resection site.
Methods: We randomly selected 500 patients undergoing colonoscopies by 5 endoscopists (100 each), who had at least one neoplastic polyp removed and completed surveillance colonoscopy within 6 months to 5 years. For 4 of 5 endoscopists, IRR had been previously assessed by marginal biopsies (IRR-Bx) in the Complete Adenoma Resection (CARE) study. We used the SMN rate at surveillance colonoscopy to estimate overall and individual IRR. In colon segments without prior neoplasia, detected polyps are either newly grown polyps or previously missed. In segments with prior polyp, recurrence may also indicate incomplete resection. Thus, the difference between neoplasia in segments with/without prior neoplasia can estimate IRR (Equation 1). The main analysis included all segments with any prior neoplastic polyp. We examined segments with one 6-19 mm prior polyp (non-pedunculated + pedunculated). Results were compared to CARE.
Results: At index colonoscopy 1165 polyps were detected in 765 of 3,000 segments. 160 segments contained a single 6-19 mm. At surveillance, a polyp was detected in 12.3% of segments without prior neoplasia and in 23.0% with a prior neoplastic polyp (median size 4 mm), resulting in an estimated IRR of 10.7% (95% conf. interval [CI] 8.7-13.2) (Table 1). Endoscopist-specific IRRs varied from 7.7% (CI 5.9-9.8) to 13.6% (CI 11.3-16.2). For segments with a single 6-19mm polyp, IRR was 5.9% (CI 2.9-11.0), ranging from 2.0% (CI 0.5-5.9) to 11.1 (CI 6.9-17.3) across endoscopists. IRR was higher for non-pedunculated (7.2%, CI 3.7-13.0) than for pedunculated (0.0%, CI 0.0-24.1). The endoscopist with the highest IRR had the highest IRR-Bx (CARE study).
Discussion: This is the first study to show that SMN can be used to estimate endoscopists’ historical IRR. Results align with prior assessments and validate this approach. The similar IRR for 6–19 mm non-pedunculated polyps (7% vs. CARE’s 10%) and the lack of recurrence after pedunculated polyp resection further validate this approach.
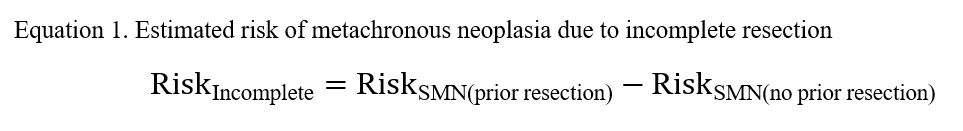
Figure: Equation 1. Estimated risk of metachronous neoplasia due to incomplete resection
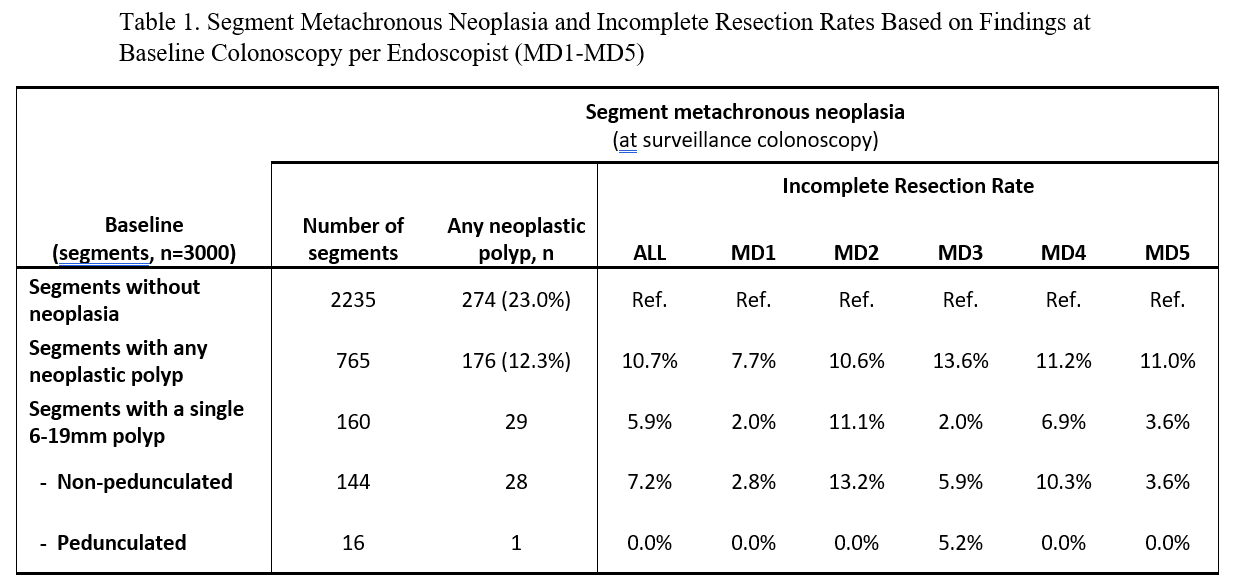
Figure: Table 1. Segment Metachronous Neoplasia and Incomplete Resection Rates Based on Findings at Baseline Colonoscopy per Endoscopist (MD1-MD5)
Disclosures:
Lauren Eichenwald indicated no relevant financial relationships.
Obaida Dairi indicated no relevant financial relationships.
Joseph Anderson indicated no relevant financial relationships.
Campbell Levy indicated no relevant financial relationships.
Steven Bensen indicated no relevant financial relationships.
Heiko Pohl indicated no relevant financial relationships.
Lauren Eichenwald, MD1, Obaida Dairi, DO1, Joseph C. Anderson, MD2, Campbell Levy, MD1, Steven P. Bensen, MD1, Heiko Pohl, MD, MS1. P4811 - Segment Metachronous Neoplasia: A Novel Approach to Measuring Endoscopist Incomplete Resection Rate, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Dartmouth Hitchcock Medical Center, Lebanon, NH; 2Dartmouth College, Hanover, NH
Introduction: Incomplete polyp resection is a key contributor to post-colonoscopy colorectal cancer, but accurately measuring an endoscopist’s incomplete resection rate (IRR) remains challenging. We assessed whether segment metachronous neoplasia (SMN) can estimate IRR for endoscopists. If valid, results should mirror marginal biopsies of the resection site.
Methods: We randomly selected 500 patients undergoing colonoscopies by 5 endoscopists (100 each), who had at least one neoplastic polyp removed and completed surveillance colonoscopy within 6 months to 5 years. For 4 of 5 endoscopists, IRR had been previously assessed by marginal biopsies (IRR-Bx) in the Complete Adenoma Resection (CARE) study. We used the SMN rate at surveillance colonoscopy to estimate overall and individual IRR. In colon segments without prior neoplasia, detected polyps are either newly grown polyps or previously missed. In segments with prior polyp, recurrence may also indicate incomplete resection. Thus, the difference between neoplasia in segments with/without prior neoplasia can estimate IRR (Equation 1). The main analysis included all segments with any prior neoplastic polyp. We examined segments with one 6-19 mm prior polyp (non-pedunculated + pedunculated). Results were compared to CARE.
Results: At index colonoscopy 1165 polyps were detected in 765 of 3,000 segments. 160 segments contained a single 6-19 mm. At surveillance, a polyp was detected in 12.3% of segments without prior neoplasia and in 23.0% with a prior neoplastic polyp (median size 4 mm), resulting in an estimated IRR of 10.7% (95% conf. interval [CI] 8.7-13.2) (Table 1). Endoscopist-specific IRRs varied from 7.7% (CI 5.9-9.8) to 13.6% (CI 11.3-16.2). For segments with a single 6-19mm polyp, IRR was 5.9% (CI 2.9-11.0), ranging from 2.0% (CI 0.5-5.9) to 11.1 (CI 6.9-17.3) across endoscopists. IRR was higher for non-pedunculated (7.2%, CI 3.7-13.0) than for pedunculated (0.0%, CI 0.0-24.1). The endoscopist with the highest IRR had the highest IRR-Bx (CARE study).
Discussion: This is the first study to show that SMN can be used to estimate endoscopists’ historical IRR. Results align with prior assessments and validate this approach. The similar IRR for 6–19 mm non-pedunculated polyps (7% vs. CARE’s 10%) and the lack of recurrence after pedunculated polyp resection further validate this approach.
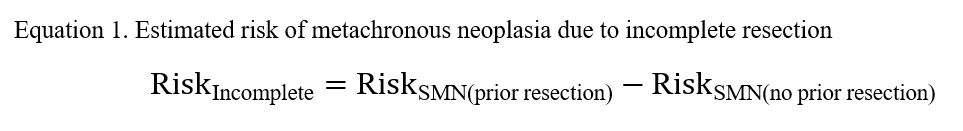
Figure: Equation 1. Estimated risk of metachronous neoplasia due to incomplete resection
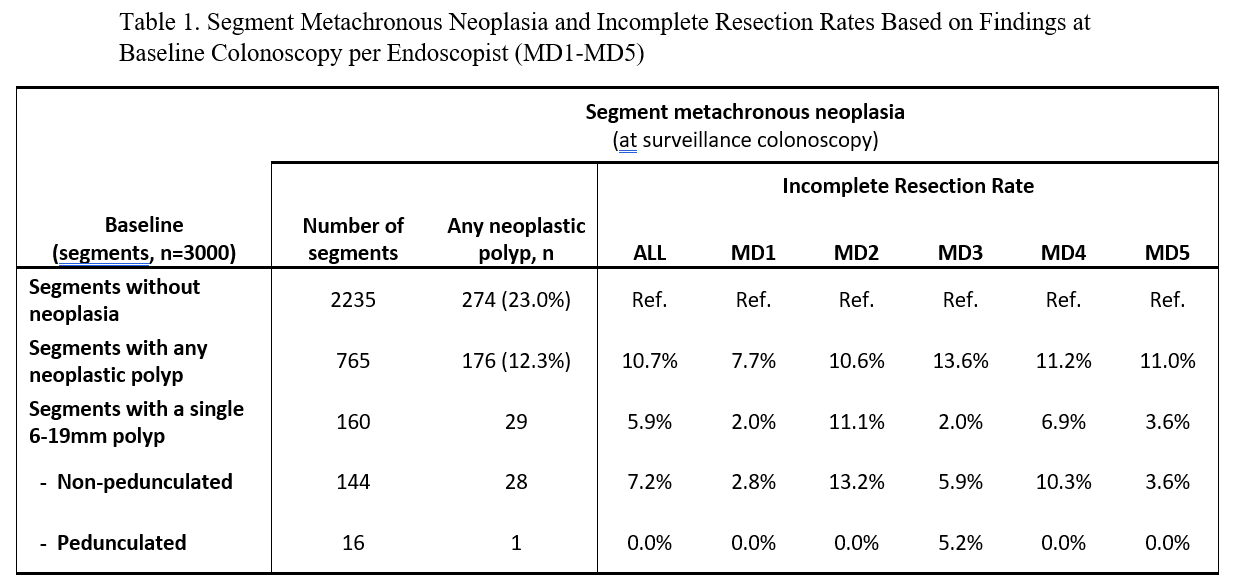
Figure: Table 1. Segment Metachronous Neoplasia and Incomplete Resection Rates Based on Findings at Baseline Colonoscopy per Endoscopist (MD1-MD5)
Disclosures:
Lauren Eichenwald indicated no relevant financial relationships.
Obaida Dairi indicated no relevant financial relationships.
Joseph Anderson indicated no relevant financial relationships.
Campbell Levy indicated no relevant financial relationships.
Steven Bensen indicated no relevant financial relationships.
Heiko Pohl indicated no relevant financial relationships.
Lauren Eichenwald, MD1, Obaida Dairi, DO1, Joseph C. Anderson, MD2, Campbell Levy, MD1, Steven P. Bensen, MD1, Heiko Pohl, MD, MS1. P4811 - Segment Metachronous Neoplasia: A Novel Approach to Measuring Endoscopist Incomplete Resection Rate, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
