Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4809 - The Financial Divide: Insurance Coverage and Its Impact on Colorectal Cancer Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Manasa Ginjupalli, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Manasa Ginjupalli, MD1, Jayalekshmi Jayakumar, MD2, Anuj Sharma, MD1, Sweta Lohani, MD1, Hamsika Moparty, MD3, Chaula Desai, MD1, Vikash Kumar, MD4, Kalimullah Quadri, MD2
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Rutgers New Jersey Medical School, Brooklyn, NY; 4Creighton University School of Medicine, Phoenix, AZ
Introduction: Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality worldwide. Access to healthcare, which is often influenced by insurance status, plays a critical role in timely diagnosis, treatment, and outcomes in patients with CRC. Uninsured or underinsured individuals may face barriers to receiving optimal care like screening colonoscopies, potentially leading to increased incidence and worse outcomes during hospitalizations. This study aims to evaluate the impact of insurance status on prevalence of CRC.
Methods: We used the National Inpatient Sample database from 2016 to 2020 to identify adult hospitalizations with CRC. The primary payer was categorized as Medicare, Medicaid, private insurance, and others. National admission estimates were calculated using sample weights, and mortality and morbidity outcomes were analyzed based on payer type. Multivariate regression analysis was performed to assess the association between insurance type and incidence of CRC and its outcomes, adjusting for age, gender, hospital characteristics, comorbidities, risk factors and the Charlson Comorbidity Index.
Results: A total of 1,390,475 CRC-related hospitalizations were identified, with a mean patient age of 66.57 years. Of these, 48.2% were female. The majority of hospitalizations were covered by Medicare (57%), followed by private insurance (28%), Medicaid (10%), and other payers (4.5%) (p< 0.001). In terms of race/ethnicity, White patients accounted for 70% of CRC hospitalizations, followed by Black (14%) and Hispanic (9%) patients (p< 0.001). Geographically, 40% of CRC admissions were from the southern United States, with 70% occurring in urban teaching hospitals
The prevalence of CRC hospitalizations was significantly higher among patients with Medicaid and private insurance compared to those with Medicare [Table 1]. Similarly, mortality outcomes revealed higher mortality rates among hospitalizations with Medicaid and private insurance compared to Medicare. Multivariate regression analysis confirmed these associations, indicating that insurance type is an independent predictor of mortality in CRC hospitalizations [Table 2].
Discussion: Insurance status significantly impacts the incidence and mortality of CRC hospitalizations. Patients with Medicaid and private insurance experience higher mortality rates compared to those with Medicare, highlighting disparities in access to care and outcomes.
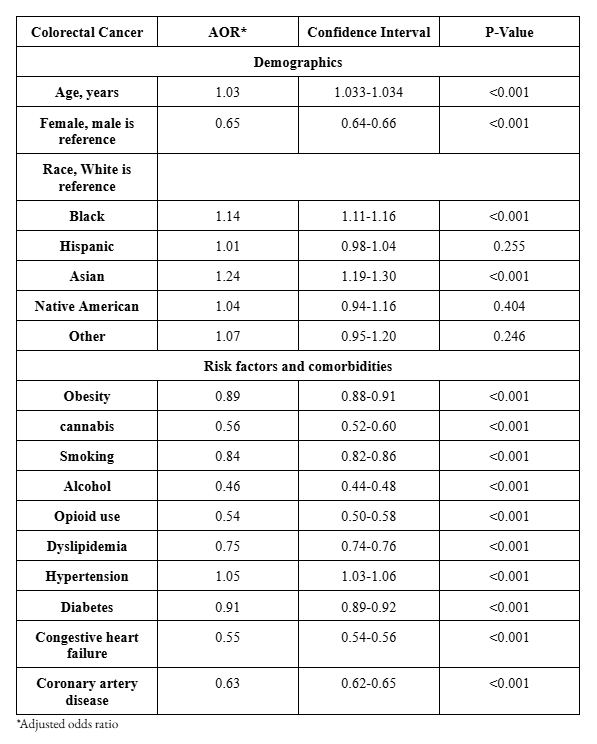
Figure:
Table 1 -Prevalence and Mortality outcomes of colorectal cancer hospitalizations stratified by payer type
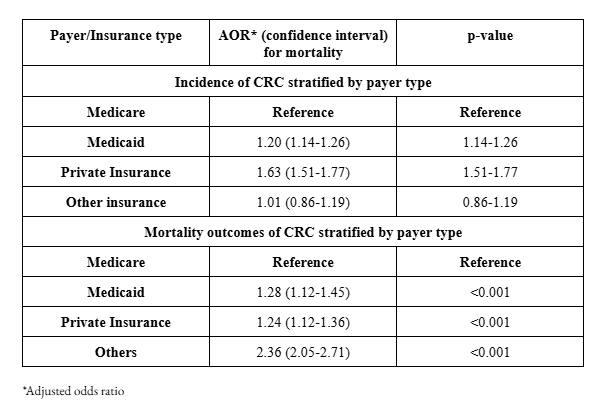
Figure:
Table 2 - Adjusted odds ratio of association between colorectal cancer and primary payer (Insurance)
Disclosures:
Manasa Ginjupalli indicated no relevant financial relationships.
Jayalekshmi Jayakumar indicated no relevant financial relationships.
Anuj Sharma indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Hamsika Moparty indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Kalimullah Quadri indicated no relevant financial relationships.
Manasa Ginjupalli, MD1, Jayalekshmi Jayakumar, MD2, Anuj Sharma, MD1, Sweta Lohani, MD1, Hamsika Moparty, MD3, Chaula Desai, MD1, Vikash Kumar, MD4, Kalimullah Quadri, MD2. P4809 - The Financial Divide: Insurance Coverage and Its Impact on Colorectal Cancer Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Rutgers New Jersey Medical School, Brooklyn, NY; 4Creighton University School of Medicine, Phoenix, AZ
Introduction: Colorectal cancer (CRC) remains a leading cause of cancer-related morbidity and mortality worldwide. Access to healthcare, which is often influenced by insurance status, plays a critical role in timely diagnosis, treatment, and outcomes in patients with CRC. Uninsured or underinsured individuals may face barriers to receiving optimal care like screening colonoscopies, potentially leading to increased incidence and worse outcomes during hospitalizations. This study aims to evaluate the impact of insurance status on prevalence of CRC.
Methods: We used the National Inpatient Sample database from 2016 to 2020 to identify adult hospitalizations with CRC. The primary payer was categorized as Medicare, Medicaid, private insurance, and others. National admission estimates were calculated using sample weights, and mortality and morbidity outcomes were analyzed based on payer type. Multivariate regression analysis was performed to assess the association between insurance type and incidence of CRC and its outcomes, adjusting for age, gender, hospital characteristics, comorbidities, risk factors and the Charlson Comorbidity Index.
Results: A total of 1,390,475 CRC-related hospitalizations were identified, with a mean patient age of 66.57 years. Of these, 48.2% were female. The majority of hospitalizations were covered by Medicare (57%), followed by private insurance (28%), Medicaid (10%), and other payers (4.5%) (p< 0.001). In terms of race/ethnicity, White patients accounted for 70% of CRC hospitalizations, followed by Black (14%) and Hispanic (9%) patients (p< 0.001). Geographically, 40% of CRC admissions were from the southern United States, with 70% occurring in urban teaching hospitals
The prevalence of CRC hospitalizations was significantly higher among patients with Medicaid and private insurance compared to those with Medicare [Table 1]. Similarly, mortality outcomes revealed higher mortality rates among hospitalizations with Medicaid and private insurance compared to Medicare. Multivariate regression analysis confirmed these associations, indicating that insurance type is an independent predictor of mortality in CRC hospitalizations [Table 2].
Discussion: Insurance status significantly impacts the incidence and mortality of CRC hospitalizations. Patients with Medicaid and private insurance experience higher mortality rates compared to those with Medicare, highlighting disparities in access to care and outcomes.
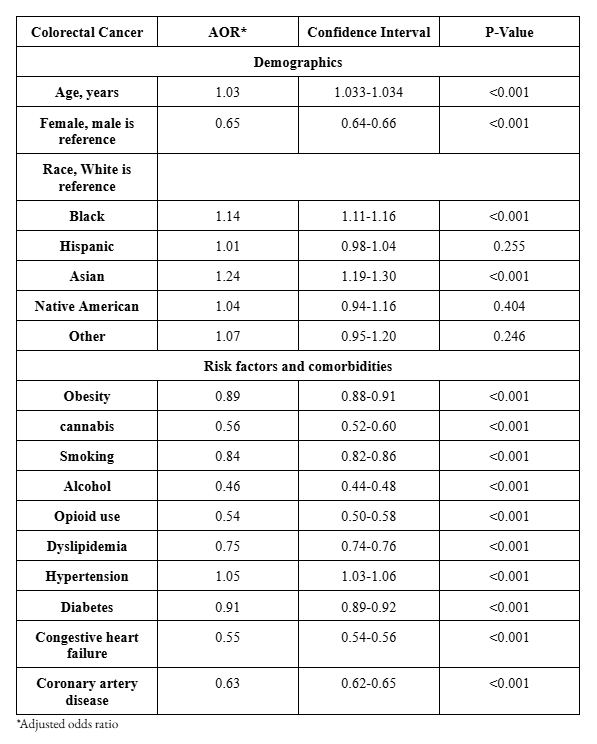
Figure:
Table 1 -Prevalence and Mortality outcomes of colorectal cancer hospitalizations stratified by payer type
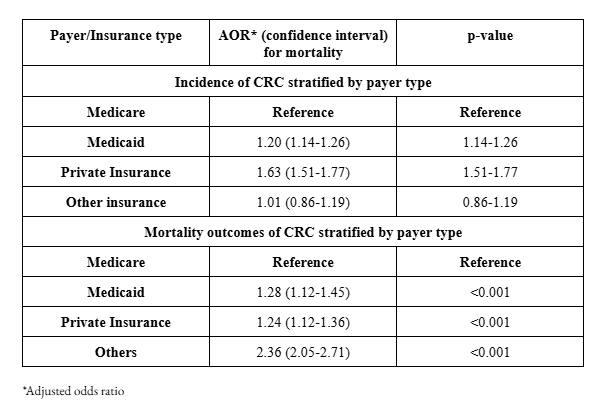
Figure:
Table 2 - Adjusted odds ratio of association between colorectal cancer and primary payer (Insurance)
Disclosures:
Manasa Ginjupalli indicated no relevant financial relationships.
Jayalekshmi Jayakumar indicated no relevant financial relationships.
Anuj Sharma indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Hamsika Moparty indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Kalimullah Quadri indicated no relevant financial relationships.
Manasa Ginjupalli, MD1, Jayalekshmi Jayakumar, MD2, Anuj Sharma, MD1, Sweta Lohani, MD1, Hamsika Moparty, MD3, Chaula Desai, MD1, Vikash Kumar, MD4, Kalimullah Quadri, MD2. P4809 - The Financial Divide: Insurance Coverage and Its Impact on Colorectal Cancer Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
