Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4772 - Long-Term Risk of Colorectal Cancer Following Cholecystectomy: A Nationwide Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Saqr Alsakarneh, MD, MS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Saqr Alsakarneh, MD, MS1, Osama Asad, MD2, Razan Aburumman, MD3, Yazan Sallam, MD2, Dushyant S. Dahiya, MD4, Mohammad Bilal, MD, FACG5, Nayantara Coelho-Prabhu, MBBS, FACG6, Aasma Shaukat, MD, MPH, FACG7
1Mayo Clinic, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Henry Ford Health, Detroit, MI; 4University of Kansas School of Medicine, Kansas City, KS; 5University of Colorado Anschutz Medical Campus, Denver, CO; 6Mayo Clinic, Rochester, MN; 7NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction: Cholecystectomy is among the most common abdominal surgeries in the U.S. and is known to alter bile acid physiology, potentially promoting mucosal inflammation and dysplasia. While associations with colonic disorders have been hypothesized, population-level data on long-term colorectal cancer (CRC) risk after cholecystectomy remain limited. We aimed to evaluate the association between cholecystectomy and incident CRC using a large national database.
Methods: We conducted a retrospective cohort study using the TriNetX research network between 2010 and 2024 to identify adult patients (≥18 years) with a history of cholecystectomy. These patients were matched 1:1 using propensity score matching with adult patients without a history of cholecystectomy, based on demographics, comorbidities, and risk factors for colorectal cancer (CRC) (Table 1). Patients with prior history of CRC were excluded from the analysis. The primary outcome was the risk of first diagnosis of CRC that occurred after the index event (cholecystectomy). Secondary outcomes assessed included colon cancer, rectal cancer, and subsite-specific cancers involving the right, transverse, and descending/sigmoid colon. Subgroup analyses were performed by gender and age categories. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: A total of 613,396 patients with a history of cholecystectomy (mean age 48.5±18.1; 68.1% female; 71.2% White) were matched to 613,396 controls (Table 1). CRC incidence was significantly higher in the cholecystectomy group (1.11% vs 0.61%; aHR: 2.16, 95% CI: 2.08–2.25; p< 0.001). Risk was elevated across all age groups, with the highest aHR in patients aged 18–45 (aHR: 2.31, 95% CI: 2.08–2.56). Males had a stronger association (aHR: 2.57) compared to females (aHR: 1.93). By subsite, the right colon showed the highest CRC risk (aHR: 3.04, 95% CI: 2.81–3.28) [Table 2].
Discussion: Our results provide real-world evidence that cholecystectomy could be an independent risk factor for CRC development. These findings suggest that clinicians should consider incorporating CRC risk assessment into the long-term follow-up of patients post-cholecystectomy, particularly those with additional risk factors.
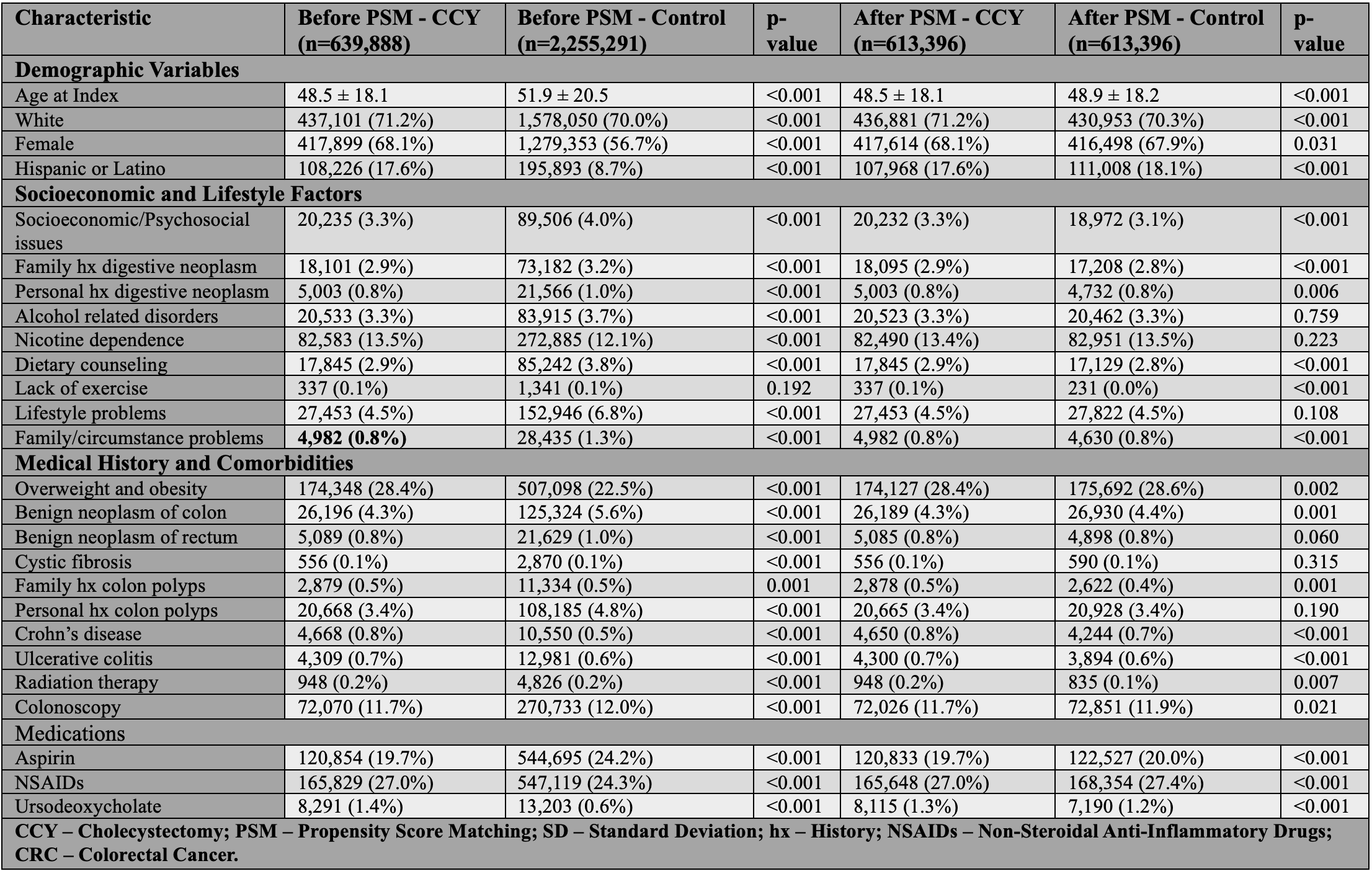
Figure: Table 1: Baseline Characteristics of Patients With and Without Prior Cholecystectomy Before and After Propensity Score Matching
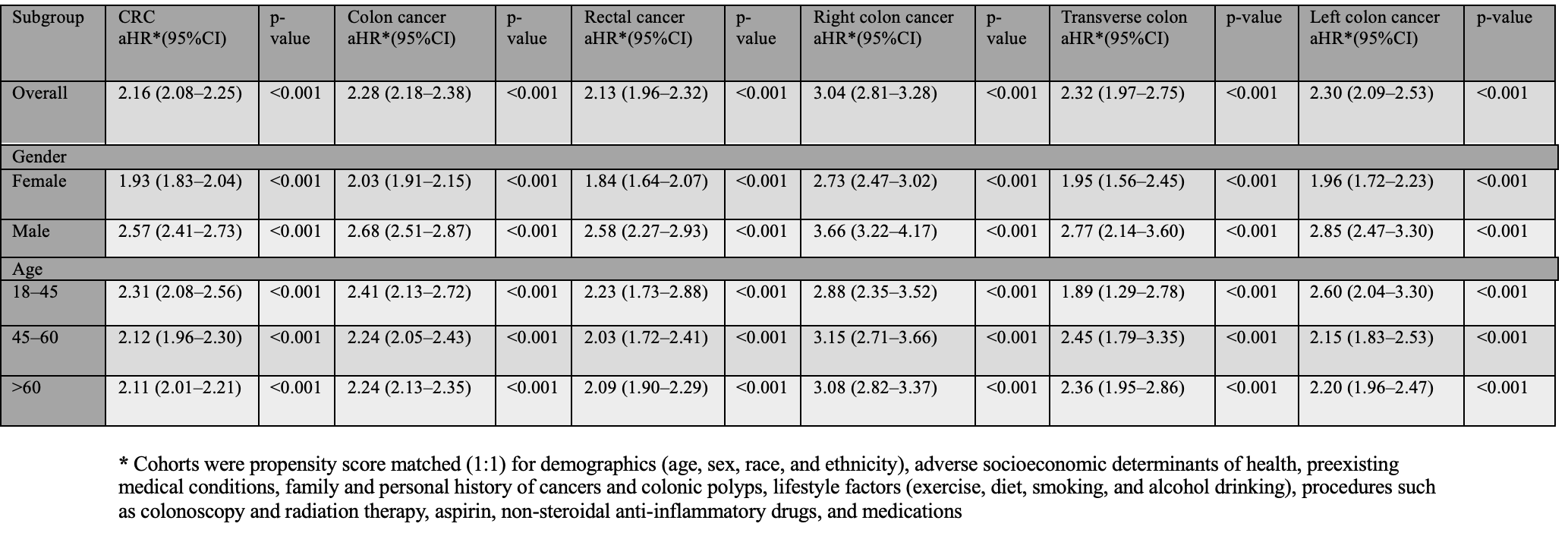
Figure: Table 2: Hazard Ratios for Colorectal Cancer Outcomes After Cholecystectomy Compared to Matched Controls – Subgroup Analysis by Gender and Age
* Cohorts were propensity score matched (1:1) for demographics (age, sex, race, and ethnicity), adverse socioeconomic determinants of health, preexisting medical conditions, family and personal history of cancers and colonic polyps, lifestyle factors (exercise, diet, smoking, and alcohol drinking), procedures such as colonoscopy and radiation therapy, aspirin, non-steroidal anti-inflammatory drugs, and IBD medications
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Osama Asad indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Yazan Sallam indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Nayantara Coelho-Prabhu indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
Saqr Alsakarneh, MD, MS1, Osama Asad, MD2, Razan Aburumman, MD3, Yazan Sallam, MD2, Dushyant S. Dahiya, MD4, Mohammad Bilal, MD, FACG5, Nayantara Coelho-Prabhu, MBBS, FACG6, Aasma Shaukat, MD, MPH, FACG7. P4772 - Long-Term Risk of Colorectal Cancer Following Cholecystectomy: A Nationwide Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Henry Ford Health, Detroit, MI; 4University of Kansas School of Medicine, Kansas City, KS; 5University of Colorado Anschutz Medical Campus, Denver, CO; 6Mayo Clinic, Rochester, MN; 7NYU Grossman School of Medicine, Division of Gastroenterology and Hepatology, New York, NY
Introduction: Cholecystectomy is among the most common abdominal surgeries in the U.S. and is known to alter bile acid physiology, potentially promoting mucosal inflammation and dysplasia. While associations with colonic disorders have been hypothesized, population-level data on long-term colorectal cancer (CRC) risk after cholecystectomy remain limited. We aimed to evaluate the association between cholecystectomy and incident CRC using a large national database.
Methods: We conducted a retrospective cohort study using the TriNetX research network between 2010 and 2024 to identify adult patients (≥18 years) with a history of cholecystectomy. These patients were matched 1:1 using propensity score matching with adult patients without a history of cholecystectomy, based on demographics, comorbidities, and risk factors for colorectal cancer (CRC) (Table 1). Patients with prior history of CRC were excluded from the analysis. The primary outcome was the risk of first diagnosis of CRC that occurred after the index event (cholecystectomy). Secondary outcomes assessed included colon cancer, rectal cancer, and subsite-specific cancers involving the right, transverse, and descending/sigmoid colon. Subgroup analyses were performed by gender and age categories. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: A total of 613,396 patients with a history of cholecystectomy (mean age 48.5±18.1; 68.1% female; 71.2% White) were matched to 613,396 controls (Table 1). CRC incidence was significantly higher in the cholecystectomy group (1.11% vs 0.61%; aHR: 2.16, 95% CI: 2.08–2.25; p< 0.001). Risk was elevated across all age groups, with the highest aHR in patients aged 18–45 (aHR: 2.31, 95% CI: 2.08–2.56). Males had a stronger association (aHR: 2.57) compared to females (aHR: 1.93). By subsite, the right colon showed the highest CRC risk (aHR: 3.04, 95% CI: 2.81–3.28) [Table 2].
Discussion: Our results provide real-world evidence that cholecystectomy could be an independent risk factor for CRC development. These findings suggest that clinicians should consider incorporating CRC risk assessment into the long-term follow-up of patients post-cholecystectomy, particularly those with additional risk factors.
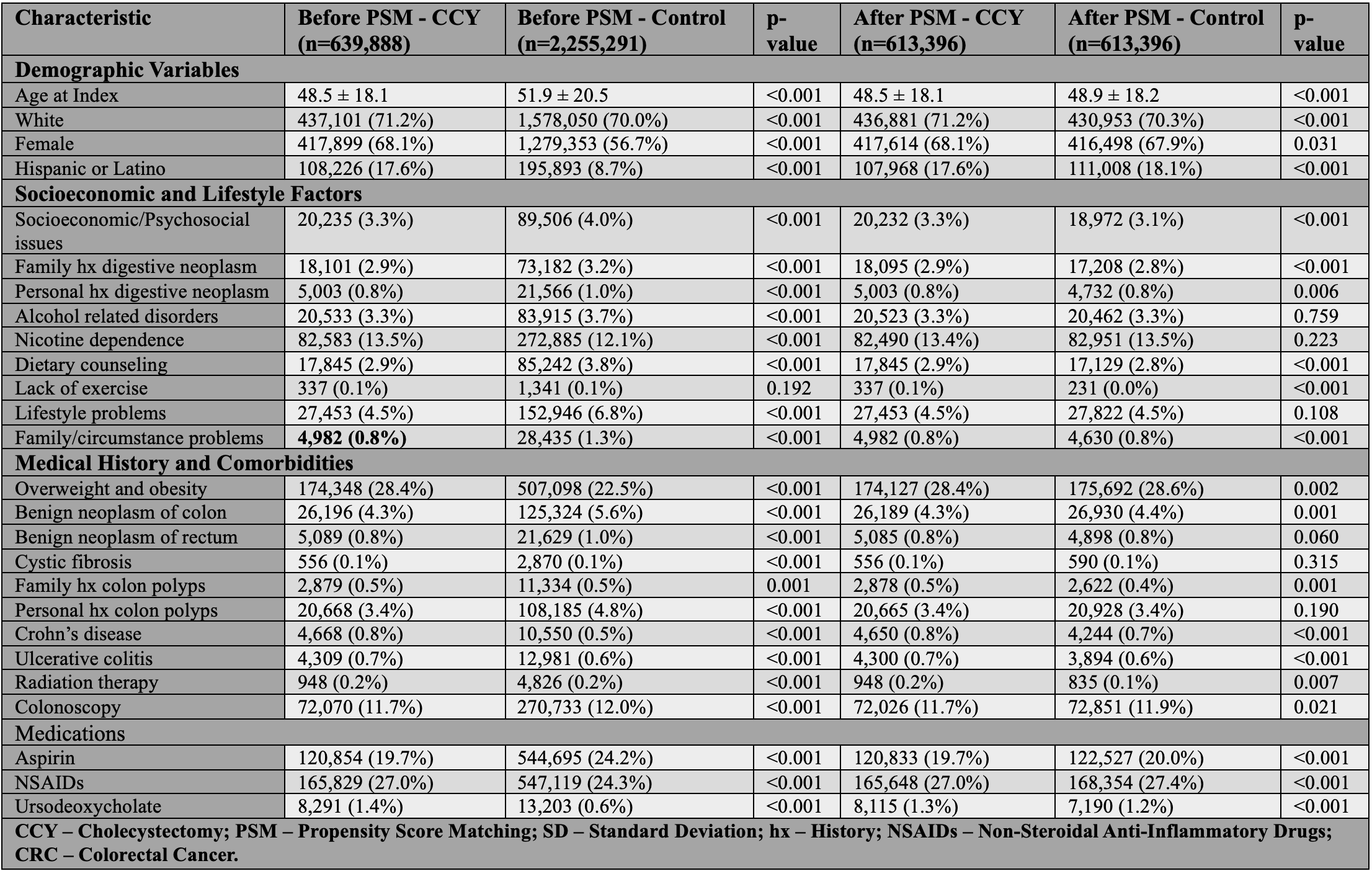
Figure: Table 1: Baseline Characteristics of Patients With and Without Prior Cholecystectomy Before and After Propensity Score Matching
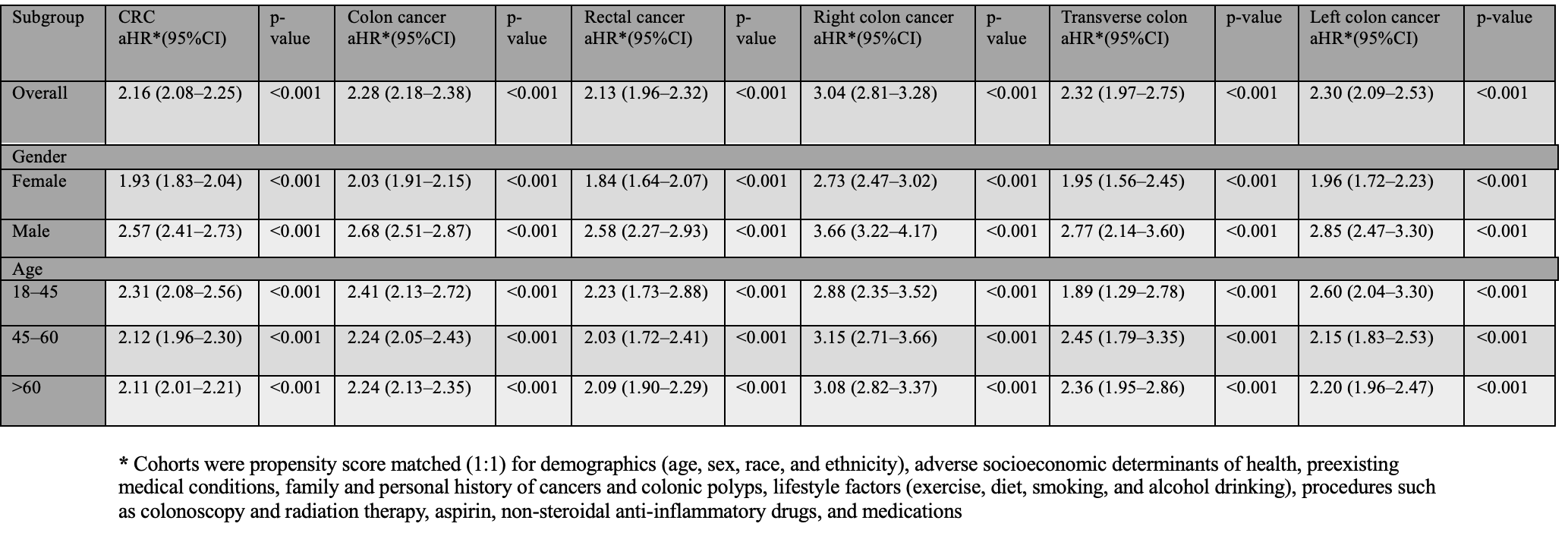
Figure: Table 2: Hazard Ratios for Colorectal Cancer Outcomes After Cholecystectomy Compared to Matched Controls – Subgroup Analysis by Gender and Age
* Cohorts were propensity score matched (1:1) for demographics (age, sex, race, and ethnicity), adverse socioeconomic determinants of health, preexisting medical conditions, family and personal history of cancers and colonic polyps, lifestyle factors (exercise, diet, smoking, and alcohol drinking), procedures such as colonoscopy and radiation therapy, aspirin, non-steroidal anti-inflammatory drugs, and IBD medications
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Osama Asad indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Yazan Sallam indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Nayantara Coelho-Prabhu indicated no relevant financial relationships.
Aasma Shaukat: Freenome inc – Consultant.
Saqr Alsakarneh, MD, MS1, Osama Asad, MD2, Razan Aburumman, MD3, Yazan Sallam, MD2, Dushyant S. Dahiya, MD4, Mohammad Bilal, MD, FACG5, Nayantara Coelho-Prabhu, MBBS, FACG6, Aasma Shaukat, MD, MPH, FACG7. P4772 - Long-Term Risk of Colorectal Cancer Following Cholecystectomy: A Nationwide Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
