Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4768 - Validation of a Colorectal Cancer Risk Prediction Tool Using 2 Large National Cohorts
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jennifer K. Maratt, MD, MS (she/her/hers)
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Award: ACG Outstanding Research Award in the Colorectal Cancer Prevention Category
Award: ACG Presidential Poster Award
Jennifer K. Maratt, MD, MS1, LaKeisha Boyd, MS1, Jason Browne, MD1, Nour Hamade, MD2, Yunpeng Yu, MS1, Kai Wang, PhD3, Mingyang Song, MD, ScD3, Charles Kahi, MD, MS1, Thomas Imperiale, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2The Queens Medical Center, Honolulu, HI; 3Harvard T.H. Chan School of Public Health, Boston, MA
Introduction: Despite development of several risk prediction models for colorectal cancer (CRC), their integration into practice is limited, in part due to limited validation data. We sought to validate the National Cancer Institute (NCI) CRC Risk Assessment Tool using two large, prospectively collected U.S. studies, the Nurses’ Health Study II (NHSII) and the Health Professionals Follow-Up Study (HPFS).
Methods: NHSII (females) and HPFS (males) participants who were >50 years of age and completed biennial study surveys were included. Excluded were those with history of IBD or CRC, those with no survey completed < 2 years of the year of study entry, and those with missing data for variables of interest. The NCI model was used to estimate 5-and 25-year CRC risk. Model calibration was measured by comparing the predicted CRC risk with the observed CRC risk by quintiles (Q), stratified by sex/cohort. Model discrimination was measured using the c-statistic, derived from a logistic regression model for each timeframe, with the odds of CRC quantified and compared by Q.
Results: A total of 87,706 individuals met eligibility criteria (HPFS=26,089; NHSII=61,617) with a median baseline year of eligibility as 2001 (IQR 1993-2005) and median age 50 (29.8% male, 96% White). During the follow-up period, 1,171 (1.34%) developed CRC or had a CRC-related death (Table 1). 5- and 25-year predicted and observed CRC risks across Qs are shown in Table 2. Despite fair discrimination (c-statistics ranging from 0.58 to 0.69), the NCI model was well-calibrated for both cohorts for relative and absolute risks for each timeframe (all omnibus p-values < 0.05). For both cohorts, the NCI model demonstrated a statistically significant and clinically important relationship between model-predicted and observed 5- and 25-year CRC risks (Table 2). For example, the 25-year absolute CRC risk for men increased from 1.50% (Q1) to 4.79% (Q5) with increasing odds when compared to Q1 (OR 1.53 for Q2 to 3.32 for Q5), while the absolute risk for women increased from 0.34% (Q1) to 0.72% (Q5), with ORs increasing from 1.13 (Q2) to 2.14 (Q5).
Discussion: The NCI CRC risk prediction model was well-calibrated and demonstrated the ability to estimate relative and absolute 5- and 25-year CRC risks for both cohorts. Applying this model in practice has the potential to improve the efficiency of CRC screening by using estimated risks to determine starting age and to choose between invasive and non-invasive screening.
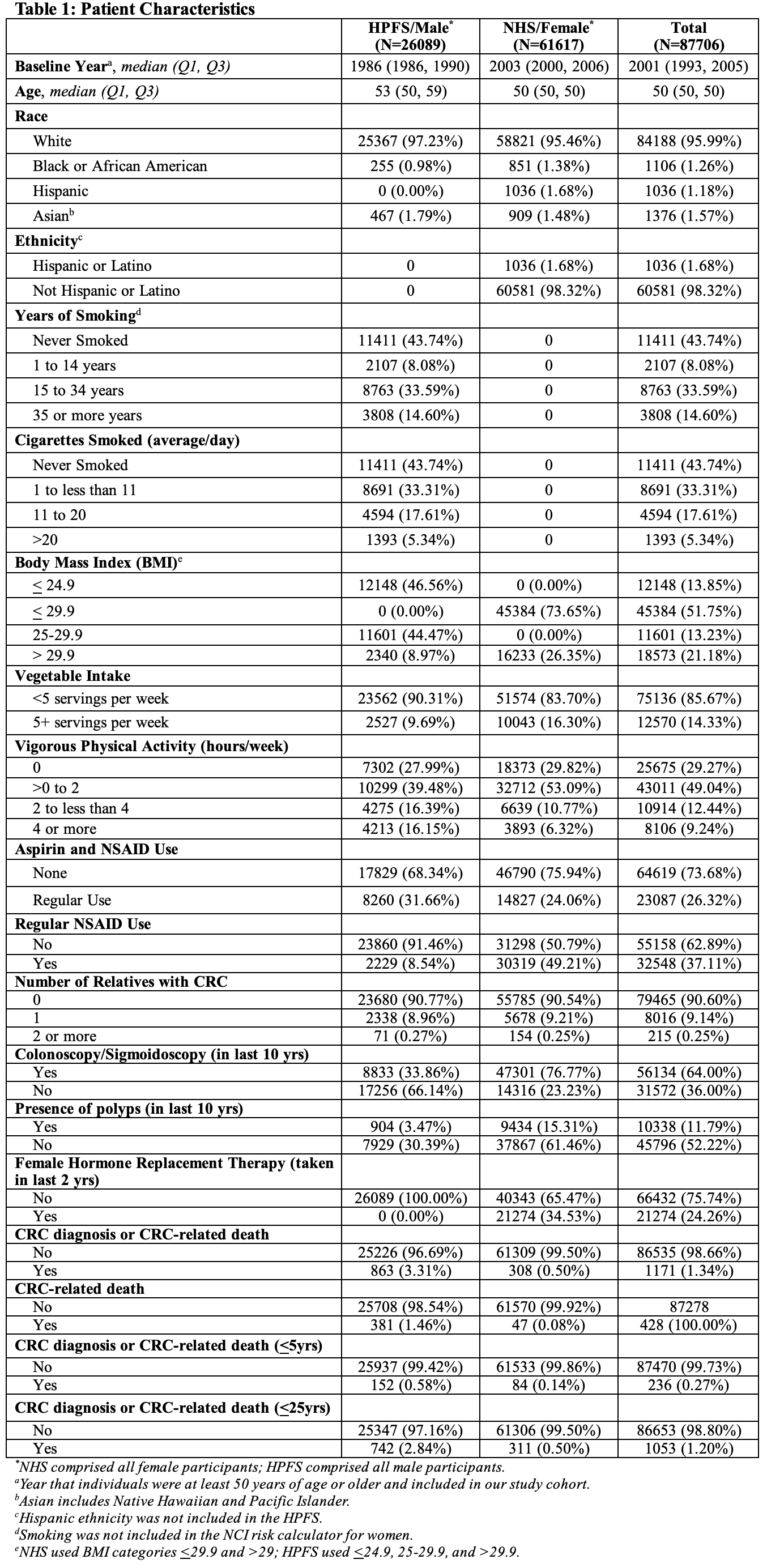
Figure: Patient Characteristics
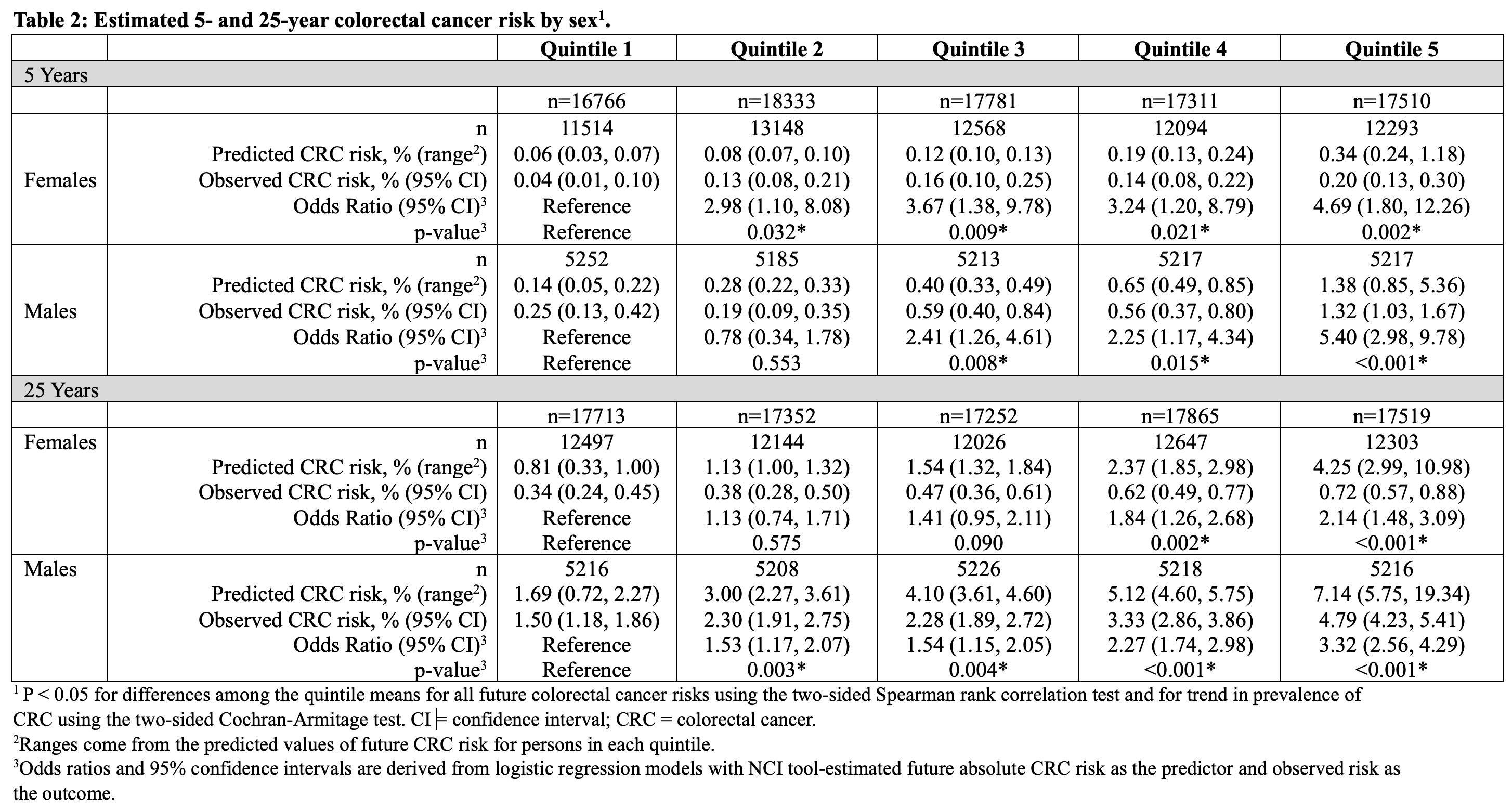
Figure: Estimated 5- and 25-year colorectal cancer risk by sex
Disclosures:
Jennifer Maratt indicated no relevant financial relationships.
LaKeisha Boyd indicated no relevant financial relationships.
Jason Browne indicated no relevant financial relationships.
Nour Hamade indicated no relevant financial relationships.
Yunpeng Yu indicated no relevant financial relationships.
Kai Wang indicated no relevant financial relationships.
Mingyang Song indicated no relevant financial relationships.
Charles Kahi indicated no relevant financial relationships.
Thomas Imperiale: Cook Medical – Consultant. Exact Sciences – Advisor or Review Panel Member, Consultant. Exact Sciences Corp – Grant/Research Support.
Jennifer K. Maratt, MD, MS1, LaKeisha Boyd, MS1, Jason Browne, MD1, Nour Hamade, MD2, Yunpeng Yu, MS1, Kai Wang, PhD3, Mingyang Song, MD, ScD3, Charles Kahi, MD, MS1, Thomas Imperiale, MD1. P4768 - Validation of a Colorectal Cancer Risk Prediction Tool Using 2 Large National Cohorts, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Award: ACG Presidential Poster Award
Jennifer K. Maratt, MD, MS1, LaKeisha Boyd, MS1, Jason Browne, MD1, Nour Hamade, MD2, Yunpeng Yu, MS1, Kai Wang, PhD3, Mingyang Song, MD, ScD3, Charles Kahi, MD, MS1, Thomas Imperiale, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2The Queens Medical Center, Honolulu, HI; 3Harvard T.H. Chan School of Public Health, Boston, MA
Introduction: Despite development of several risk prediction models for colorectal cancer (CRC), their integration into practice is limited, in part due to limited validation data. We sought to validate the National Cancer Institute (NCI) CRC Risk Assessment Tool using two large, prospectively collected U.S. studies, the Nurses’ Health Study II (NHSII) and the Health Professionals Follow-Up Study (HPFS).
Methods: NHSII (females) and HPFS (males) participants who were >50 years of age and completed biennial study surveys were included. Excluded were those with history of IBD or CRC, those with no survey completed < 2 years of the year of study entry, and those with missing data for variables of interest. The NCI model was used to estimate 5-and 25-year CRC risk. Model calibration was measured by comparing the predicted CRC risk with the observed CRC risk by quintiles (Q), stratified by sex/cohort. Model discrimination was measured using the c-statistic, derived from a logistic regression model for each timeframe, with the odds of CRC quantified and compared by Q.
Results: A total of 87,706 individuals met eligibility criteria (HPFS=26,089; NHSII=61,617) with a median baseline year of eligibility as 2001 (IQR 1993-2005) and median age 50 (29.8% male, 96% White). During the follow-up period, 1,171 (1.34%) developed CRC or had a CRC-related death (Table 1). 5- and 25-year predicted and observed CRC risks across Qs are shown in Table 2. Despite fair discrimination (c-statistics ranging from 0.58 to 0.69), the NCI model was well-calibrated for both cohorts for relative and absolute risks for each timeframe (all omnibus p-values < 0.05). For both cohorts, the NCI model demonstrated a statistically significant and clinically important relationship between model-predicted and observed 5- and 25-year CRC risks (Table 2). For example, the 25-year absolute CRC risk for men increased from 1.50% (Q1) to 4.79% (Q5) with increasing odds when compared to Q1 (OR 1.53 for Q2 to 3.32 for Q5), while the absolute risk for women increased from 0.34% (Q1) to 0.72% (Q5), with ORs increasing from 1.13 (Q2) to 2.14 (Q5).
Discussion: The NCI CRC risk prediction model was well-calibrated and demonstrated the ability to estimate relative and absolute 5- and 25-year CRC risks for both cohorts. Applying this model in practice has the potential to improve the efficiency of CRC screening by using estimated risks to determine starting age and to choose between invasive and non-invasive screening.
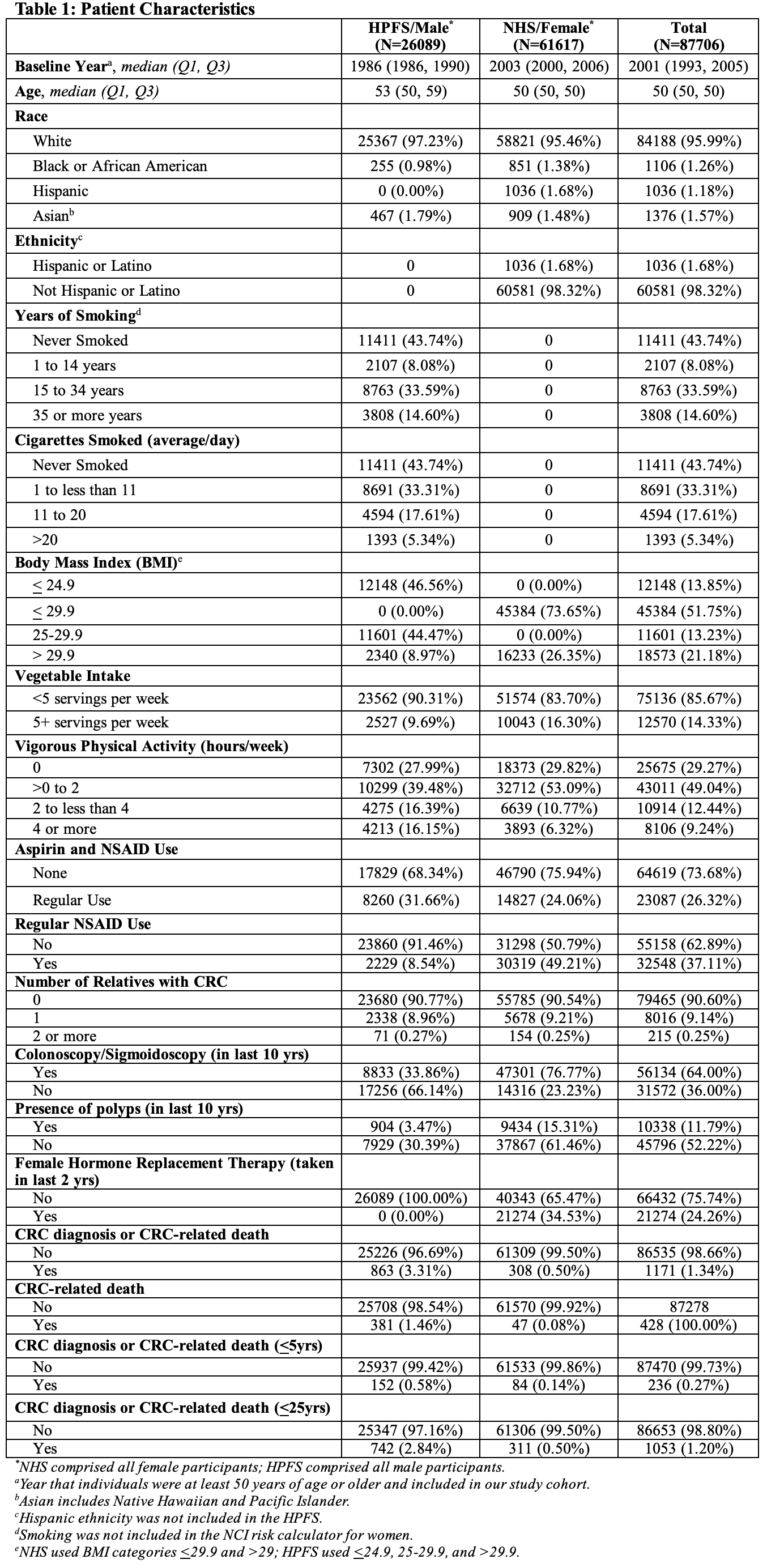
Figure: Patient Characteristics
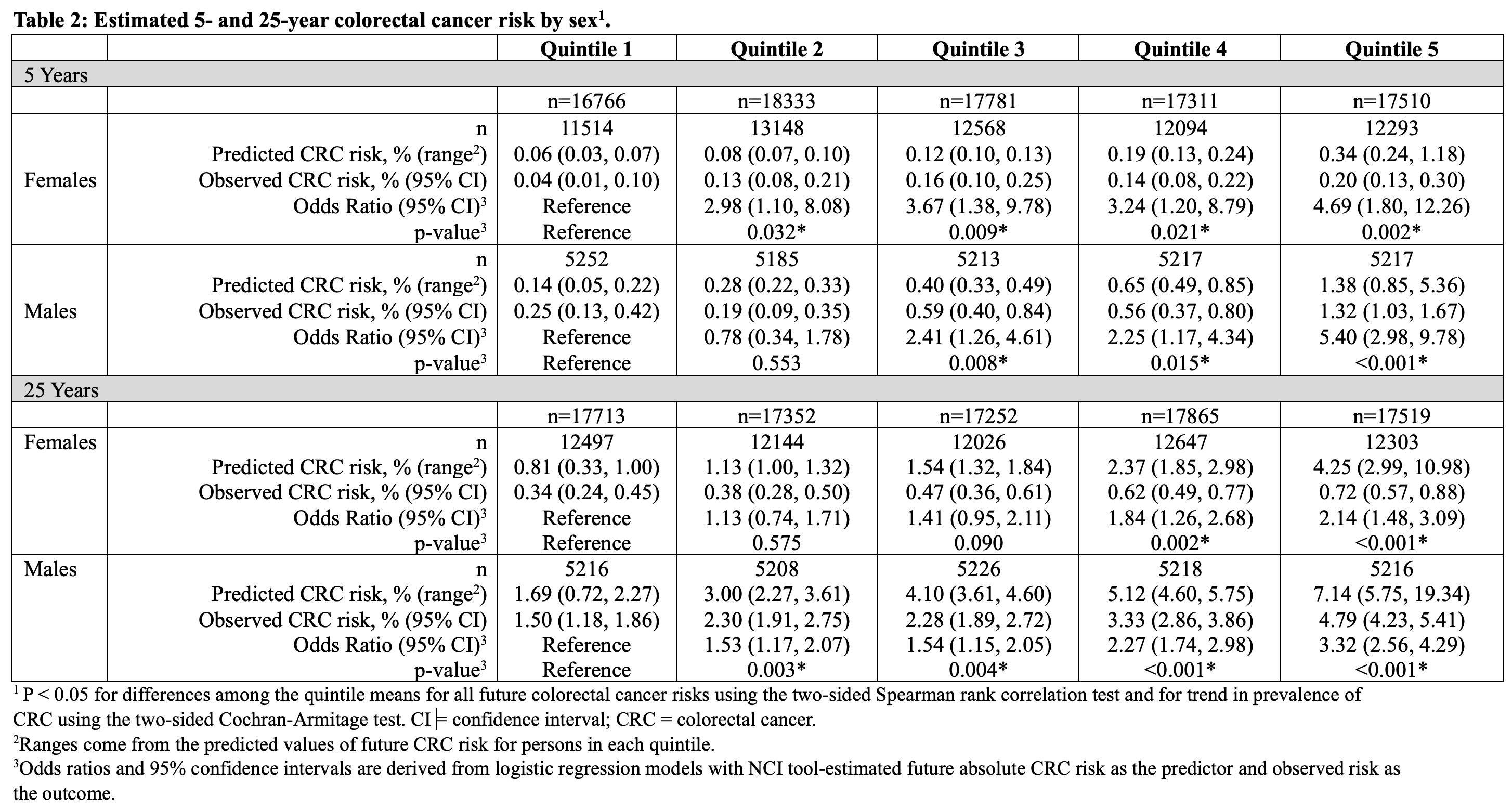
Figure: Estimated 5- and 25-year colorectal cancer risk by sex
Disclosures:
Jennifer Maratt indicated no relevant financial relationships.
LaKeisha Boyd indicated no relevant financial relationships.
Jason Browne indicated no relevant financial relationships.
Nour Hamade indicated no relevant financial relationships.
Yunpeng Yu indicated no relevant financial relationships.
Kai Wang indicated no relevant financial relationships.
Mingyang Song indicated no relevant financial relationships.
Charles Kahi indicated no relevant financial relationships.
Thomas Imperiale: Cook Medical – Consultant. Exact Sciences – Advisor or Review Panel Member, Consultant. Exact Sciences Corp – Grant/Research Support.
Jennifer K. Maratt, MD, MS1, LaKeisha Boyd, MS1, Jason Browne, MD1, Nour Hamade, MD2, Yunpeng Yu, MS1, Kai Wang, PhD3, Mingyang Song, MD, ScD3, Charles Kahi, MD, MS1, Thomas Imperiale, MD1. P4768 - Validation of a Colorectal Cancer Risk Prediction Tool Using 2 Large National Cohorts, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.


