Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4754 - Reducing Delays in Colonoscopy and EGD Access Through Real-Time Virtual Scheduling: A Quality Improvement Initiative
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fariha Hasan, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Fariha Hasan, MD1, Maryanna Schweininger, DO1, Ahmed Z. Shahzad, 2, Alexis Sieber, MD, BA3, Houston R. Ward, BS4, Tanay-Veer Gandhi, BA5, Krystal Hunter, PhD, MBA1, Christina Tofani, MD, FACG2, Anthony Infantolino, MD6, Rachel Frank, MD7
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper Medical School of Rowan University, Philadelphia, PA; 4Cooper Medical School of Rowan University, Bound Brook, NJ; 5Cooper Medical School of Rowan University, Morganville, NJ; 6MD Anderson Cooper Digestive Health, Mt Laurel, NJ; 7Cooper University Hospital, Philadelphia, PA
Introduction: Timely endoscopic access is critical for preventing colorectal cancer. However, scheduling inefficiencies persist as a significant barrier and contribute to prolonged wait times. At our institution, patients were scheduled for endoscopy through telephone calls, often resulting in miscommunication, or no-shows. To address this, we implemented a quality improvement intervention using a virtual scheduler embedded in the gastroenterology clinic. This study evaluated its impact on procedure completion rates.
Methods: Pre-Intervention:
We performed a retrospective chart review of all patients who were scheduled for a colonoscopy or EGD between February and May, 2024 at an underserved tertiary care center. During this period, standard scheduling procedures were used without the aid of a real-time scheduler.
Post-Intervention:
Beginning August 5, 2024, a virtual scheduler was introduced at the clinic to assist patients in booking their colonoscopy or EGD appointments prior to leaving the office. All patients scheduled were prospectively followed.
Results: A total of 658 patients were evenly divided between the pre- and post-intervention groups (328 vs. 330). While demographic characteristics such as sex, race, and language were similar across groups, there were statistically significant differences in age and income. Implementation of the virtual scheduler significantly reduced time from procedure scheduling to completion (mean: 65.9 vs. 55.8 days, p = 0.018) and time from procedure ordering to completion (mean: 79.3 vs. 56.1 days, p < 0.001). Despite improvements in timeliness, overall procedure completion rates remained comparable between the pre- and post-intervention groups (69.8% vs. 70.9%, p = 0.759).
Although contact rates and willingness to complete follow-up surveys were comparable (p = 0.127 and p = 0.744), post-intervention patients reported more barriers, including life demands (29.0% vs. 10.4%, p = 0.001), health-related concerns (18.0% vs. 3.1%, p = 0.001), time constraints for bowel preparation (p = 0.007), and cost-related barriers (23.2% vs. 11.1%, p = 0.028).
Discussion: The implementation of a virtual scheduler significantly reduced delays in scheduling and overall time to procedure, highlighting its effectiveness as a patient navigation tool. However, social and financial barriers persist, underscoring the need for multi-level interventions to further enhance procedure completion in vulnerable populations.
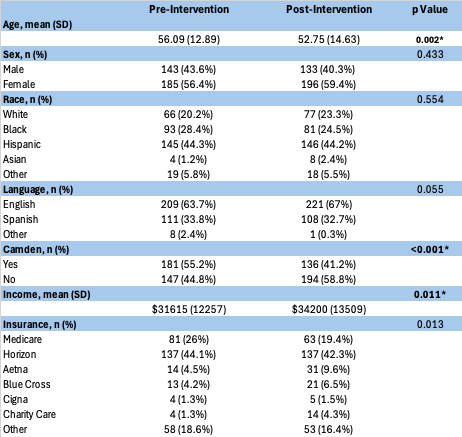
Figure: Table 1: Demographics between pre- and post intervention group
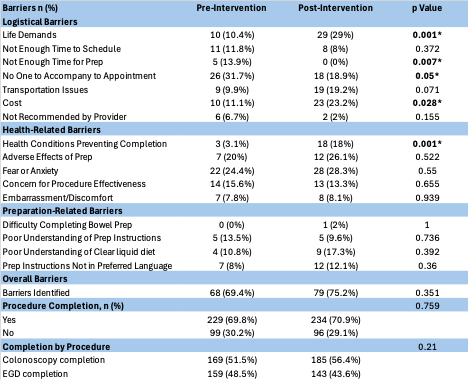
Figure: Table 2: Barriers between pre-and post intervention group
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Ahmed Shahzad indicated no relevant financial relationships.
Alexis Sieber indicated no relevant financial relationships.
Houston Ward: McKesson Corp. – Stock-publicly held company(excluding mutual/index funds).
Tanay-Veer Gandhi indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Christina Tofani indicated no relevant financial relationships.
Anthony Infantolino indicated no relevant financial relationships.
Rachel Frank indicated no relevant financial relationships.
Fariha Hasan, MD1, Maryanna Schweininger, DO1, Ahmed Z. Shahzad, 2, Alexis Sieber, MD, BA3, Houston R. Ward, BS4, Tanay-Veer Gandhi, BA5, Krystal Hunter, PhD, MBA1, Christina Tofani, MD, FACG2, Anthony Infantolino, MD6, Rachel Frank, MD7. P4754 - Reducing Delays in Colonoscopy and EGD Access Through Real-Time Virtual Scheduling: A Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ; 3Cooper Medical School of Rowan University, Philadelphia, PA; 4Cooper Medical School of Rowan University, Bound Brook, NJ; 5Cooper Medical School of Rowan University, Morganville, NJ; 6MD Anderson Cooper Digestive Health, Mt Laurel, NJ; 7Cooper University Hospital, Philadelphia, PA
Introduction: Timely endoscopic access is critical for preventing colorectal cancer. However, scheduling inefficiencies persist as a significant barrier and contribute to prolonged wait times. At our institution, patients were scheduled for endoscopy through telephone calls, often resulting in miscommunication, or no-shows. To address this, we implemented a quality improvement intervention using a virtual scheduler embedded in the gastroenterology clinic. This study evaluated its impact on procedure completion rates.
Methods: Pre-Intervention:
We performed a retrospective chart review of all patients who were scheduled for a colonoscopy or EGD between February and May, 2024 at an underserved tertiary care center. During this period, standard scheduling procedures were used without the aid of a real-time scheduler.
Post-Intervention:
Beginning August 5, 2024, a virtual scheduler was introduced at the clinic to assist patients in booking their colonoscopy or EGD appointments prior to leaving the office. All patients scheduled were prospectively followed.
Results: A total of 658 patients were evenly divided between the pre- and post-intervention groups (328 vs. 330). While demographic characteristics such as sex, race, and language were similar across groups, there were statistically significant differences in age and income. Implementation of the virtual scheduler significantly reduced time from procedure scheduling to completion (mean: 65.9 vs. 55.8 days, p = 0.018) and time from procedure ordering to completion (mean: 79.3 vs. 56.1 days, p < 0.001). Despite improvements in timeliness, overall procedure completion rates remained comparable between the pre- and post-intervention groups (69.8% vs. 70.9%, p = 0.759).
Although contact rates and willingness to complete follow-up surveys were comparable (p = 0.127 and p = 0.744), post-intervention patients reported more barriers, including life demands (29.0% vs. 10.4%, p = 0.001), health-related concerns (18.0% vs. 3.1%, p = 0.001), time constraints for bowel preparation (p = 0.007), and cost-related barriers (23.2% vs. 11.1%, p = 0.028).
Discussion: The implementation of a virtual scheduler significantly reduced delays in scheduling and overall time to procedure, highlighting its effectiveness as a patient navigation tool. However, social and financial barriers persist, underscoring the need for multi-level interventions to further enhance procedure completion in vulnerable populations.
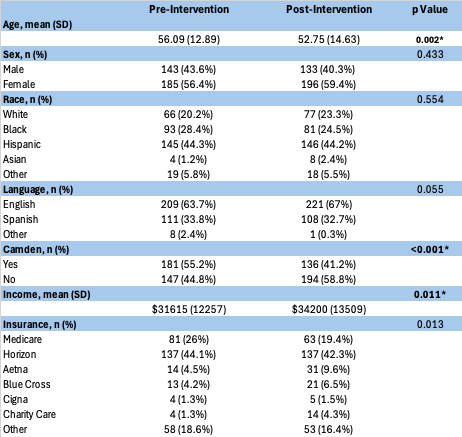
Figure: Table 1: Demographics between pre- and post intervention group
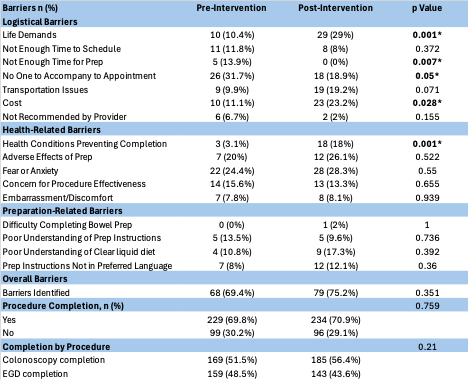
Figure: Table 2: Barriers between pre-and post intervention group
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Ahmed Shahzad indicated no relevant financial relationships.
Alexis Sieber indicated no relevant financial relationships.
Houston Ward: McKesson Corp. – Stock-publicly held company(excluding mutual/index funds).
Tanay-Veer Gandhi indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Christina Tofani indicated no relevant financial relationships.
Anthony Infantolino indicated no relevant financial relationships.
Rachel Frank indicated no relevant financial relationships.
Fariha Hasan, MD1, Maryanna Schweininger, DO1, Ahmed Z. Shahzad, 2, Alexis Sieber, MD, BA3, Houston R. Ward, BS4, Tanay-Veer Gandhi, BA5, Krystal Hunter, PhD, MBA1, Christina Tofani, MD, FACG2, Anthony Infantolino, MD6, Rachel Frank, MD7. P4754 - Reducing Delays in Colonoscopy and EGD Access Through Real-Time Virtual Scheduling: A Quality Improvement Initiative, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
