Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4748 - Colorectal Cancer Burden From Metabolic and Dietary Risks in the United States Over 3 Decades
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Omar Al Ta'ani, MD
Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA
Pittsburgh, PA
Presenting Author(s)
Omar Al Ta’ani, MD1, Rahul Karna, MD2, Yahya Alhalalmeh, MD3, Aseel Saadeh, MD4, Mohammad Bilal, MD, FACG5
1Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 2University of Minnesota Medical Center, Minneapolis, MN; 3New York Medical College - Saint Michael's Medical Center, Newark, NJ; 4Geisinger Health System, Danville, PA; 5University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Colorectal cancer (CRC) remains a major contributor to cancer-related morbidity and mortality in the United States. A significant portion of this burden is attributable to modifiable risk factors, and obtaining insight into long-term trends and geographic variation in CRC burden attributable to these factors is essential to ascertain effective prevention strategies.
Methods: We analyzed data from the Global Burden of Disease (GBD) study to estimate the burden of CRC attributable to elevated body mass index (BMI), high fasting plasma glucose, and dietary risks in the United States from 1990 to 2021. Age-standardized disability-adjusted life years (DALYs) and deaths were extracted for each risk factor. Temporal trends were assessed by sex and year using line graphs, while geographic variation was visualized with state-level choropleth maps. All analyses were completed using R software version 4.3.2.
Results: In 1990, colorectal cancer attributable to dietary risks accounted for 26,740 deaths, increasing to 30,257 in 2021 (+13.2%). Deaths due to high fasting plasma glucose rose from 4,826 to 8,793 (+82.2%), while those from high BMI increased from 7,377 to 11,402 (+54.6%). Over the same period, the age-standardized DALY rate declined by 31.5% for dietary risks and 8.2% for high BMI but rose by 2.8% for high fasting plasma glucose (Figure 1).
In 2021, the highest BMI-attributable CRC DALY rate was observed in Mississippi (81.7 per 100,000; 95% CI: 35.6–129.2) and the lowest in Colorado (36.3 per 100,000; 95% CI: 15.2–59.1). The highest BMI-attributable CRC death rate was also in Mississippi (3.0 per 100,000; 95% CI: 1.3–4.8), and the lowest in Colorado (1.5 per 100,000; 95% CI: 0.6–2.4), as shown in Figure 2.
Discussion: Although the age-standardized DALY rates attributable to dietary and metabolic risks have declined over the past three decades, the absolute burden of CRC linked to these modifiable factors remains substantial. Given the modifiable nature of these exposures, targeted public health interventions are needed to curb preventable CRC mortality and morbidity in the United States.
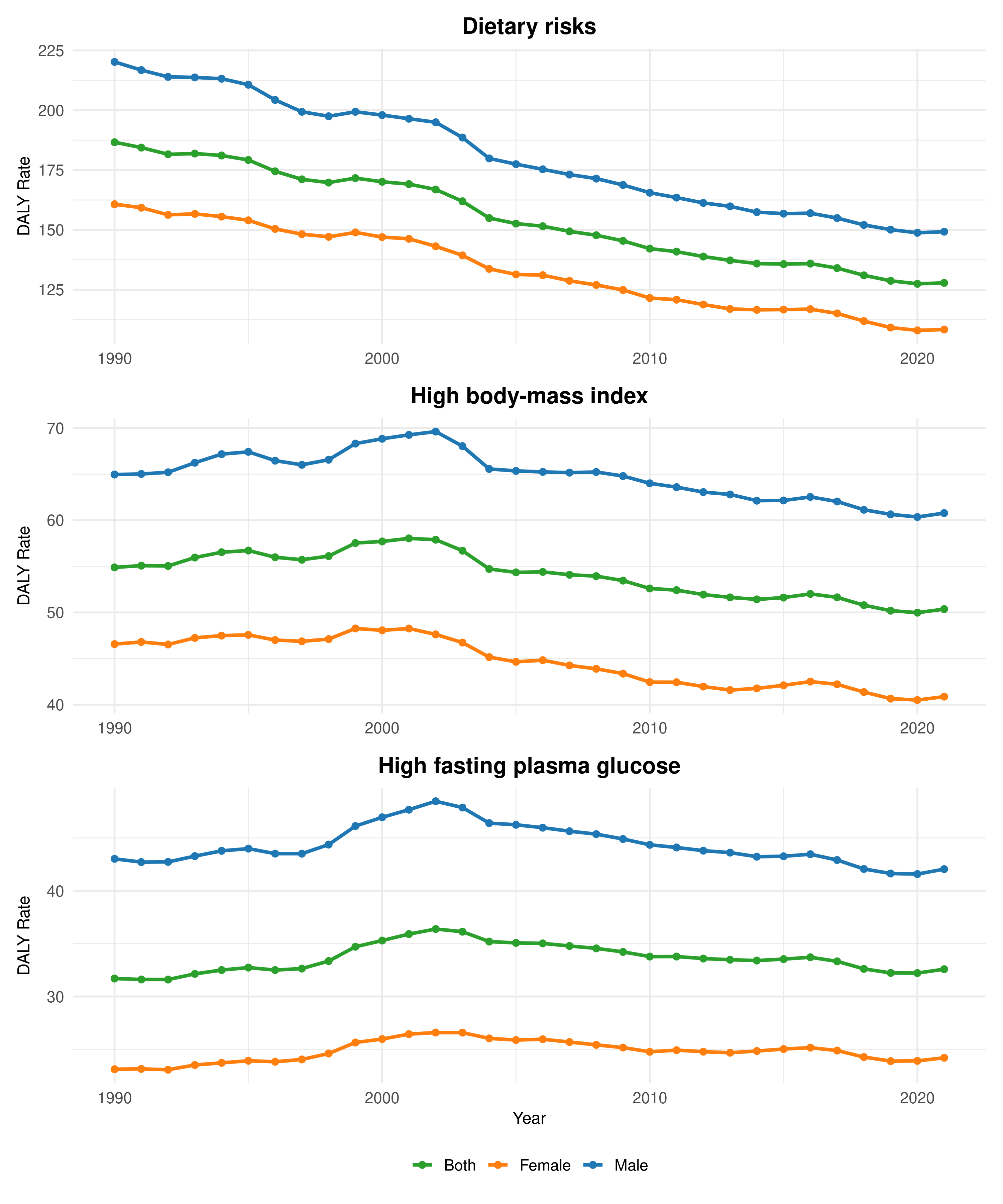
Figure: Figure 1. Trends in Age-Standardized DALY Rates Attributable to Metabolic and Dietary Risk Factors (1990–2021)

Figure: Figure 2. Geographic Variation in Age-Standardized DALY and Death Rates Attributable to Elevated Body-Mass Index in the United States (1990 vs. 2021)
Disclosures:
Omar Al Ta’ani indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Aseel Saadeh indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Omar Al Ta’ani, MD1, Rahul Karna, MD2, Yahya Alhalalmeh, MD3, Aseel Saadeh, MD4, Mohammad Bilal, MD, FACG5. P4748 - Colorectal Cancer Burden From Metabolic and Dietary Risks in the United States Over 3 Decades, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine, Allegheny Health Network, Pittsburgh, Pennsylvania, USA, Pittsburgh, PA; 2University of Minnesota Medical Center, Minneapolis, MN; 3New York Medical College - Saint Michael's Medical Center, Newark, NJ; 4Geisinger Health System, Danville, PA; 5University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Colorectal cancer (CRC) remains a major contributor to cancer-related morbidity and mortality in the United States. A significant portion of this burden is attributable to modifiable risk factors, and obtaining insight into long-term trends and geographic variation in CRC burden attributable to these factors is essential to ascertain effective prevention strategies.
Methods: We analyzed data from the Global Burden of Disease (GBD) study to estimate the burden of CRC attributable to elevated body mass index (BMI), high fasting plasma glucose, and dietary risks in the United States from 1990 to 2021. Age-standardized disability-adjusted life years (DALYs) and deaths were extracted for each risk factor. Temporal trends were assessed by sex and year using line graphs, while geographic variation was visualized with state-level choropleth maps. All analyses were completed using R software version 4.3.2.
Results: In 1990, colorectal cancer attributable to dietary risks accounted for 26,740 deaths, increasing to 30,257 in 2021 (+13.2%). Deaths due to high fasting plasma glucose rose from 4,826 to 8,793 (+82.2%), while those from high BMI increased from 7,377 to 11,402 (+54.6%). Over the same period, the age-standardized DALY rate declined by 31.5% for dietary risks and 8.2% for high BMI but rose by 2.8% for high fasting plasma glucose (Figure 1).
In 2021, the highest BMI-attributable CRC DALY rate was observed in Mississippi (81.7 per 100,000; 95% CI: 35.6–129.2) and the lowest in Colorado (36.3 per 100,000; 95% CI: 15.2–59.1). The highest BMI-attributable CRC death rate was also in Mississippi (3.0 per 100,000; 95% CI: 1.3–4.8), and the lowest in Colorado (1.5 per 100,000; 95% CI: 0.6–2.4), as shown in Figure 2.
Discussion: Although the age-standardized DALY rates attributable to dietary and metabolic risks have declined over the past three decades, the absolute burden of CRC linked to these modifiable factors remains substantial. Given the modifiable nature of these exposures, targeted public health interventions are needed to curb preventable CRC mortality and morbidity in the United States.
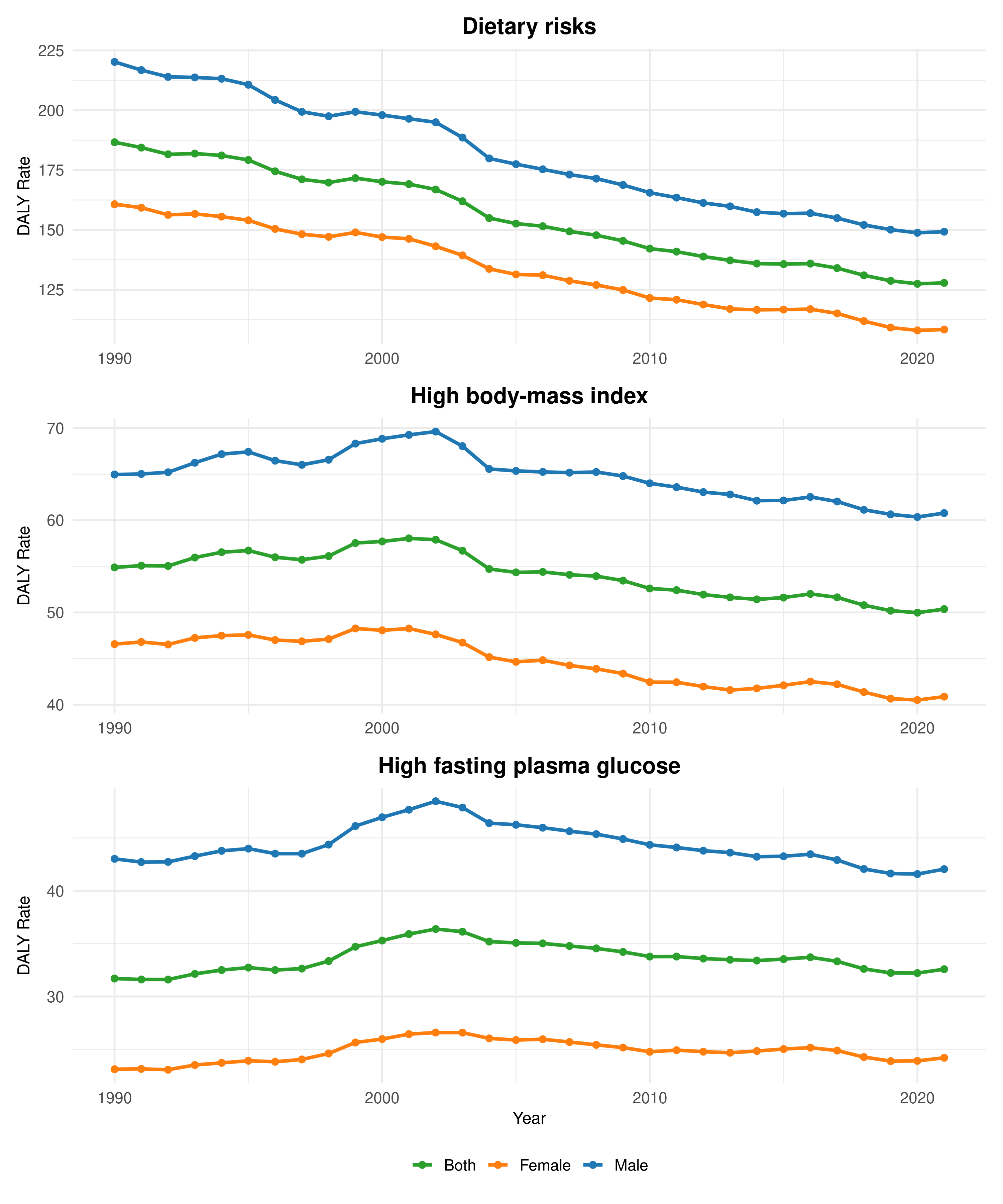
Figure: Figure 1. Trends in Age-Standardized DALY Rates Attributable to Metabolic and Dietary Risk Factors (1990–2021)

Figure: Figure 2. Geographic Variation in Age-Standardized DALY and Death Rates Attributable to Elevated Body-Mass Index in the United States (1990 vs. 2021)
Disclosures:
Omar Al Ta’ani indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Yahya Alhalalmeh indicated no relevant financial relationships.
Aseel Saadeh indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Omar Al Ta’ani, MD1, Rahul Karna, MD2, Yahya Alhalalmeh, MD3, Aseel Saadeh, MD4, Mohammad Bilal, MD, FACG5. P4748 - Colorectal Cancer Burden From Metabolic and Dietary Risks in the United States Over 3 Decades, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
