Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4743 - Evaluating the Benefits of Continued Polyp Surveillance Beyond Age 80: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JA
James Anundson, MS, BS
Georgetown University School of Medicine
Columbia, MD
Presenting Author(s)
James Anundson, MS, BS1, Priyanka Kanth, MD2, Deema Sallout, MBBS2
1Georgetown University School of Medicine, Columbia, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Current guidelines for colorectal cancer (CRC) screening recommend stopping routine colonoscopy surveillance in average-risk adults by age 75, or by 85 depending on health status. However, limited data exist to guide decisions about continuing polyp surveillance beyond age 80, particularly regarding its clinical value and risk-benefit profile.
This study evaluated whether continued polyp surveillance after age 80 is associated with meaningful clinical benefits or increased risks. We compared polyp prevalence, CRC incidence, post-procedural complications, procedure burden, and hospitalization rates between those who continued surveillance and those who did not.
Methods: We conducted a retrospective cohort study using data from the All of Us Research Program, a large, diverse NIH-backed database. Participants contribute data via surveys, electronic health records, biospecimens, physical measurements, and wearables. All data are de-identified and standardized using the OMOP Common Data Model. Adults over age 80 who had colonoscopies were grouped into continued surveillance (n=112) or discontinued (n=393,484). Procedures were categorized as post-80 surveillance if colonoscopy or polypectomy occurred after age 80. Procedure indication (screening, diagnostic, or surveillance) could not be definitively determined. The primary outcome was polyp prevalence; secondary outcomes included CRC incidence, 14-day post-procedural complications, and hospitalization rates.
Results: Patients who continued surveillance had significantly higher odds of polyp detection (OR 4.84, 95% CI: 3.19–7.36; p< 0.001) and higher relative risk of CRC diagnosis (RR 1.08, 95% CI: 1.02–1.14; p< 0.001). However, absolute CRC incidence remained low in both groups (8.0% vs 0.9%), possibly reflecting detection bias. In the continued group, 7.1% experienced GI hemorrhage post-procedure, with no cases of perforation, infection, or surgical hemorrhage. Among surveillance patients, 54.5% were female; racial distribution was 84.8% White, 6.2% Black or African American, and 8.0% Other. Increased detection may not equate to clinical benefit and could increase procedural risk.
Discussion: Surveillance beyond age 80 was linked to more polyp and CRC detection, but minimal CRC impact and non-trivial procedural risks. These findings raise questions about the value of routine colonoscopy in this age group and support individualized decision-making. Limitations include lack of indication data and lack of cause-specific mortality information.
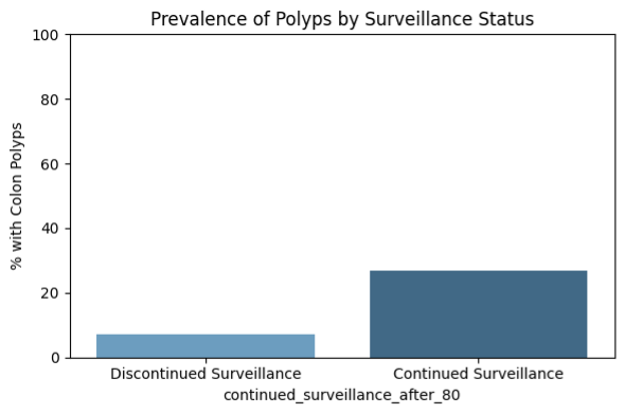
Figure: Figure: Prevalence of colon polyps stratified by surveillance status among adults over age 80.
Patients who continued surveillance after age 80 had a significantly higher prevalence of polyps (≈27%) compared to those who discontinued surveillance (≈8%), suggesting increased polyp detection in the surveillance group. However, this may reflect increased procedural exposure rather than true biological difference.
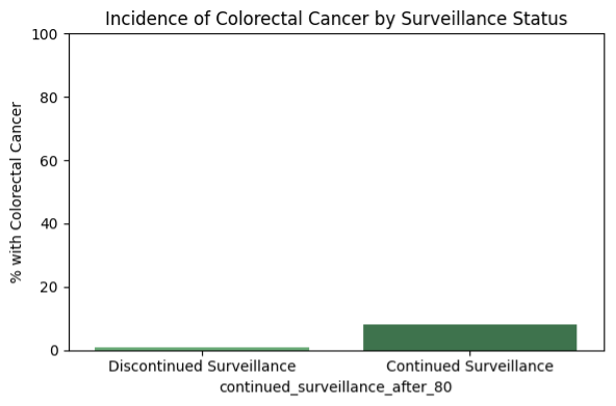
Figure: Figure: Incidence of colorectal cancer (CRC) by surveillance status in adults over age 80.
Colorectal cancer was diagnosed more frequently in patients who continued surveillance (8.0%) compared to those who discontinued surveillance (0.9%). This difference may reflect increased detection due to ongoing procedures rather than a true increase in CRC incidence.
Disclosures:
James Anundson indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Deema Sallout indicated no relevant financial relationships.
James Anundson, MS, BS1, Priyanka Kanth, MD2, Deema Sallout, MBBS2. P4743 - Evaluating the Benefits of Continued Polyp Surveillance Beyond Age 80: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Georgetown University School of Medicine, Columbia, MD; 2MedStar Georgetown University Hospital, Washington, DC
Introduction: Current guidelines for colorectal cancer (CRC) screening recommend stopping routine colonoscopy surveillance in average-risk adults by age 75, or by 85 depending on health status. However, limited data exist to guide decisions about continuing polyp surveillance beyond age 80, particularly regarding its clinical value and risk-benefit profile.
This study evaluated whether continued polyp surveillance after age 80 is associated with meaningful clinical benefits or increased risks. We compared polyp prevalence, CRC incidence, post-procedural complications, procedure burden, and hospitalization rates between those who continued surveillance and those who did not.
Methods: We conducted a retrospective cohort study using data from the All of Us Research Program, a large, diverse NIH-backed database. Participants contribute data via surveys, electronic health records, biospecimens, physical measurements, and wearables. All data are de-identified and standardized using the OMOP Common Data Model. Adults over age 80 who had colonoscopies were grouped into continued surveillance (n=112) or discontinued (n=393,484). Procedures were categorized as post-80 surveillance if colonoscopy or polypectomy occurred after age 80. Procedure indication (screening, diagnostic, or surveillance) could not be definitively determined. The primary outcome was polyp prevalence; secondary outcomes included CRC incidence, 14-day post-procedural complications, and hospitalization rates.
Results: Patients who continued surveillance had significantly higher odds of polyp detection (OR 4.84, 95% CI: 3.19–7.36; p< 0.001) and higher relative risk of CRC diagnosis (RR 1.08, 95% CI: 1.02–1.14; p< 0.001). However, absolute CRC incidence remained low in both groups (8.0% vs 0.9%), possibly reflecting detection bias. In the continued group, 7.1% experienced GI hemorrhage post-procedure, with no cases of perforation, infection, or surgical hemorrhage. Among surveillance patients, 54.5% were female; racial distribution was 84.8% White, 6.2% Black or African American, and 8.0% Other. Increased detection may not equate to clinical benefit and could increase procedural risk.
Discussion: Surveillance beyond age 80 was linked to more polyp and CRC detection, but minimal CRC impact and non-trivial procedural risks. These findings raise questions about the value of routine colonoscopy in this age group and support individualized decision-making. Limitations include lack of indication data and lack of cause-specific mortality information.
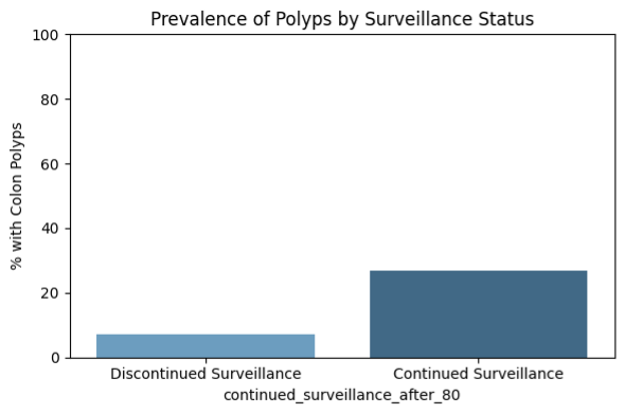
Figure: Figure: Prevalence of colon polyps stratified by surveillance status among adults over age 80.
Patients who continued surveillance after age 80 had a significantly higher prevalence of polyps (≈27%) compared to those who discontinued surveillance (≈8%), suggesting increased polyp detection in the surveillance group. However, this may reflect increased procedural exposure rather than true biological difference.
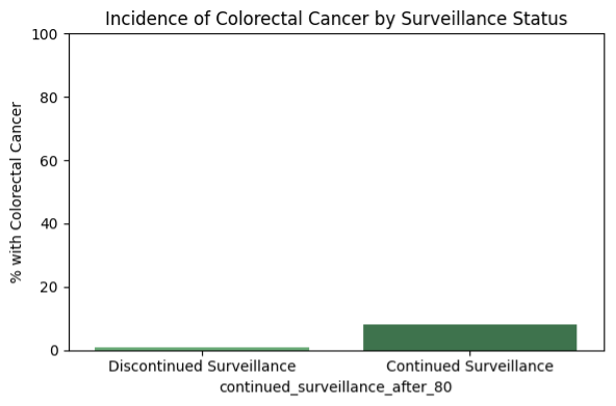
Figure: Figure: Incidence of colorectal cancer (CRC) by surveillance status in adults over age 80.
Colorectal cancer was diagnosed more frequently in patients who continued surveillance (8.0%) compared to those who discontinued surveillance (0.9%). This difference may reflect increased detection due to ongoing procedures rather than a true increase in CRC incidence.
Disclosures:
James Anundson indicated no relevant financial relationships.
Priyanka Kanth indicated no relevant financial relationships.
Deema Sallout indicated no relevant financial relationships.
James Anundson, MS, BS1, Priyanka Kanth, MD2, Deema Sallout, MBBS2. P4743 - Evaluating the Benefits of Continued Polyp Surveillance Beyond Age 80: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
