Tuesday Poster Session
Category: Colorectal Cancer Prevention
P4742 - Diagnostic Outcomes and Demographic Patterns After Positive Multitarget Stool DNA Screening in a US Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad AbuAssi, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Mohammad Abuassi, MD1, Kinan Obeidat, MD2, Mahmoud Y. Madi, MD3
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2University of Texas Medical Branch, Santa Fe, TX; 3University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Multitarget stool DNA (mt-sDNA) tests, including Cologuard, provide a noninvasive approach to colorectal cancer (CRC) screening. However, real-world outcomes and demographic variations following positive results remain insufficiently studied.
Methods: We conducted a retrospective cohort study using the TriNetX US Collaborative Network, a federated platform aggregating de-identified electronic health records from 67 healthcare organizations. Adults aged 45–85 who received a positive multitarget stool DNA (mt-sDNA) test (LOINC 77354-9) between January 1, 2022, and December 31, 2024, and subsequently underwent colonoscopy (CPT 1022231) were included. Patients without follow-up colonoscopy after a positive mt-sDNA result were excluded. Primary outcomes were incidence proportions of colorectal cancer (ICD-10: C18–C21), adenomas (D12), and diverticulosis (K57). TriNetX calculated incidence proportions and stratified results by age, sex, race, and ethnicity.
Results: A total of 12,543 patients met inclusion criteria. The mean age was 65 years (SD ±9), with 53.8% female and 87.5% identifying as White. Only 3.0% were Hispanic/Latino, while ethnicity data were unknown in 38.5%. Diagnostic colonoscopy revealed adenomas in 58.4% of patients, diverticulosis in 38.8%, and CRC in 2.6%. Males had a significantly higher incidence of both CRC (3.2% vs. 2.0%, p < 0.001) and adenomas (63.4% vs. 54.2%, p < 0.001) compared to females. Racial disparities were notable American Indian or Alaska Native patients had the highest CRC incidence (28.6%) and adenoma prevalence (73.5%), though subgroup sample size constraints may affect generalizability. Asian and Black patients had slightly higher CRC rates compared to White patients (4.3% and 3.9% vs. 2.4%). CRC incidence increased with age, peaking at 6.7% in the 80–84 age group. Diverticulosis rates also increased with age, affecting nearly 60% of those aged 80–84.
Discussion: Following a positive mt-sDNA test, nearly 60% of patients were found to have adenomas, and 1 in 40 had CRC. Diagnostic yields varied substantially across age, sex, and race, with older adults and racial minorities, particularly American Indian or Alaska Native patients, experiencing disproportionately higher rates of CRC and adenomas. These findings show the diagnostic value of mt-sDNA testing and highlight disparities in post-screening outcomes, reinforcing the necessity of timely colonoscopy follow-up and advocating for more equitable CRC screening initiatives tailored to diverse populations.
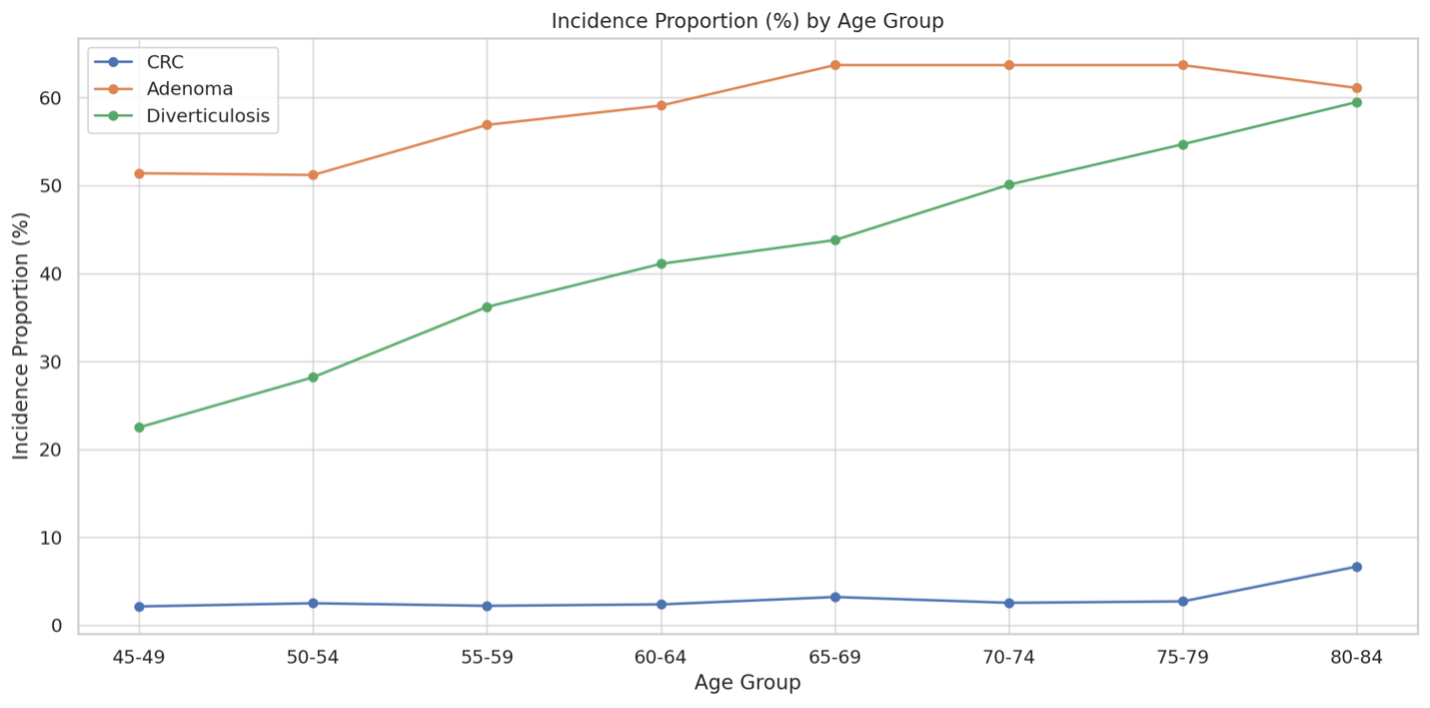
Figure: Incidence proportions of CRC, adenomas, and diverticulosis stratified by age group. CRC and diverticulosis rates increased with age, with CRC peaking in the 80–84 age group. Adenomas were consistently prevalent across all age groups.

Figure: Incidence proportions of colorectal cancer (CRC), adenomas, and diverticulosis among patients with positive mt-sDNA tests, stratified by race and sex. Males had higher rates of CRC and adenomas. Racial disparities were observed, with American Indian or Alaska Native patients exhibiting the highest incidence of both outcomes.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Kinan Obeidat, MD2, Mahmoud Y. Madi, MD3. P4742 - Diagnostic Outcomes and Demographic Patterns After Positive Multitarget Stool DNA Screening in a US Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2University of Texas Medical Branch, Santa Fe, TX; 3University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Multitarget stool DNA (mt-sDNA) tests, including Cologuard, provide a noninvasive approach to colorectal cancer (CRC) screening. However, real-world outcomes and demographic variations following positive results remain insufficiently studied.
Methods: We conducted a retrospective cohort study using the TriNetX US Collaborative Network, a federated platform aggregating de-identified electronic health records from 67 healthcare organizations. Adults aged 45–85 who received a positive multitarget stool DNA (mt-sDNA) test (LOINC 77354-9) between January 1, 2022, and December 31, 2024, and subsequently underwent colonoscopy (CPT 1022231) were included. Patients without follow-up colonoscopy after a positive mt-sDNA result were excluded. Primary outcomes were incidence proportions of colorectal cancer (ICD-10: C18–C21), adenomas (D12), and diverticulosis (K57). TriNetX calculated incidence proportions and stratified results by age, sex, race, and ethnicity.
Results: A total of 12,543 patients met inclusion criteria. The mean age was 65 years (SD ±9), with 53.8% female and 87.5% identifying as White. Only 3.0% were Hispanic/Latino, while ethnicity data were unknown in 38.5%. Diagnostic colonoscopy revealed adenomas in 58.4% of patients, diverticulosis in 38.8%, and CRC in 2.6%. Males had a significantly higher incidence of both CRC (3.2% vs. 2.0%, p < 0.001) and adenomas (63.4% vs. 54.2%, p < 0.001) compared to females. Racial disparities were notable American Indian or Alaska Native patients had the highest CRC incidence (28.6%) and adenoma prevalence (73.5%), though subgroup sample size constraints may affect generalizability. Asian and Black patients had slightly higher CRC rates compared to White patients (4.3% and 3.9% vs. 2.4%). CRC incidence increased with age, peaking at 6.7% in the 80–84 age group. Diverticulosis rates also increased with age, affecting nearly 60% of those aged 80–84.
Discussion: Following a positive mt-sDNA test, nearly 60% of patients were found to have adenomas, and 1 in 40 had CRC. Diagnostic yields varied substantially across age, sex, and race, with older adults and racial minorities, particularly American Indian or Alaska Native patients, experiencing disproportionately higher rates of CRC and adenomas. These findings show the diagnostic value of mt-sDNA testing and highlight disparities in post-screening outcomes, reinforcing the necessity of timely colonoscopy follow-up and advocating for more equitable CRC screening initiatives tailored to diverse populations.
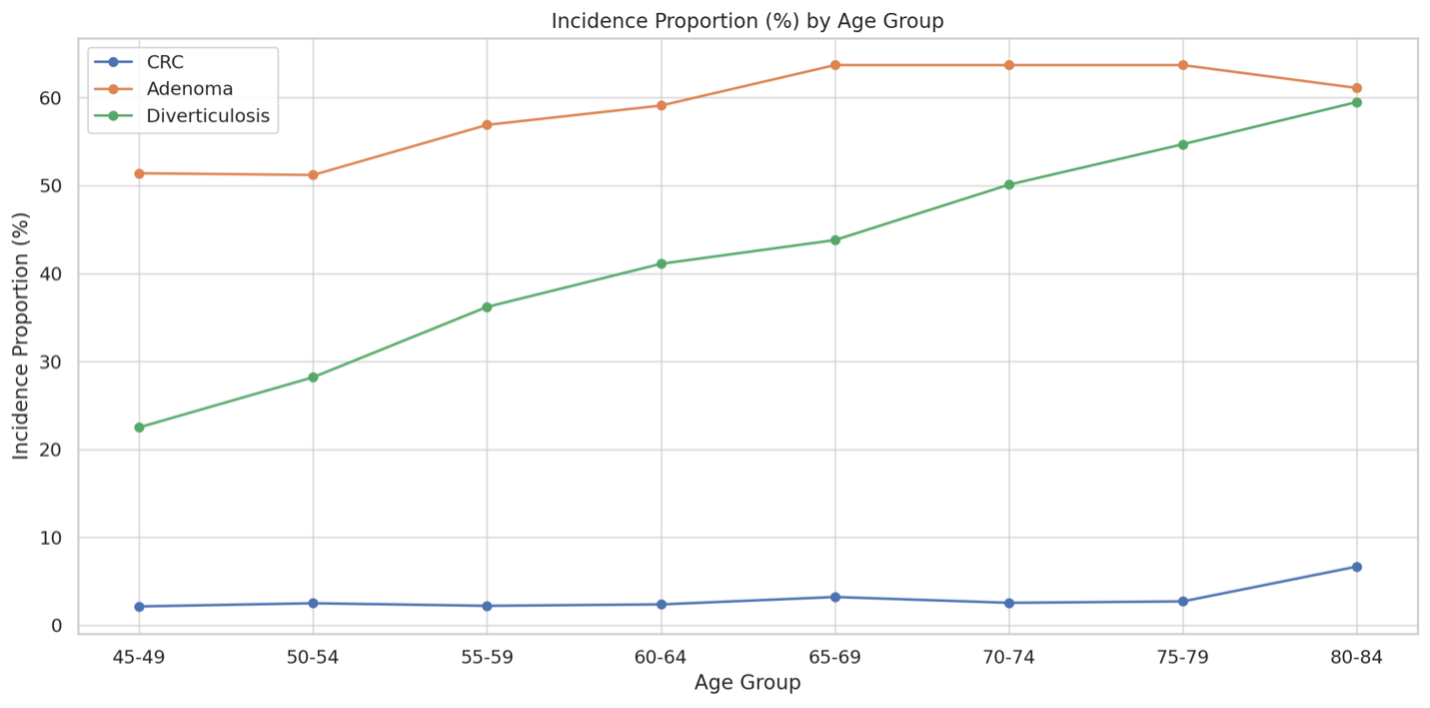
Figure: Incidence proportions of CRC, adenomas, and diverticulosis stratified by age group. CRC and diverticulosis rates increased with age, with CRC peaking in the 80–84 age group. Adenomas were consistently prevalent across all age groups.

Figure: Incidence proportions of colorectal cancer (CRC), adenomas, and diverticulosis among patients with positive mt-sDNA tests, stratified by race and sex. Males had higher rates of CRC and adenomas. Racial disparities were observed, with American Indian or Alaska Native patients exhibiting the highest incidence of both outcomes.
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Kinan Obeidat, MD2, Mahmoud Y. Madi, MD3. P4742 - Diagnostic Outcomes and Demographic Patterns After Positive Multitarget Stool DNA Screening in a US Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
