Tuesday Poster Session
Category: Colon
P4708 - Hyperbaric Oxygen Therapy for Ischemic Colon Ulceration in a Patient With Immune-Mediated Colitis: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RP
Rohan Patel (he/him/his)
MD Anderson Cancer Center
Houston, Texas
Presenting Author(s)
Award: ACG Presidential Poster Award
Rohan Patel, 1, Carolina Cruz, MD2, Maria Julia M. N.. Santos, MD1, Sharada Wali, MBBS, MPH2, Krishnavathana Varatharajalu, MD1, Yinghong Wang, MD, PhD, MS2
1MD Anderson Cancer Center, Houston, TX; 2University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Immune checkpoint inhibitors (ICI) enhance antitumor T-cell responses, boosting immune function. However, they may trigger off-target inflammation mimicking autoimmunity, often manifesting as colitis. While clinical remission is commonly achieved with medical therapy, symptoms may persist in those with prior colorectal surgeries, particularly when anastomoses are located in vascular watershed areas prone to ischemia and reduced drug perfusion. Hyperbaric oxygen therapy (HBOT), which promotes angiogenesis and tissue oxygenation, has shown benefits in inflammatory bowel disease. We report a novel case of ICI-mediated colitis (IMC) with persistent rectal ulcers near the surgical anastomosis refractory to standard therapy, achieve mucosal healing with HBOT.
Case Description/
Methods: A 77-year-old female with stage II lung adenocarcinoma, status post right upper lobectomy, received carboplatin, pemetrexed, and subsequently 12 cycles of atezolizumab –discontinued due to toxicity. Her history also included diverticulitis managed with partial colectomy and anastomosis 4 years earlier. She developed grade 3 diarrhea and grade 2 colitis (CTCAE), with rectal bleeding. Colonoscopy revealed pancolitis (Mayo 3) with ulcerations, histologic inflammation, and fecal calprotectin (FC) of 2343 µg/g. Despite corticosteroids, three vedolizumab doses, and two fecal microbiota transplantations (FMT) with PuraStat spray over nine months, only partial relief was achieved, with persistent urgency and hematochezia. At the 2nd FMT, colonoscopy showed remaining large ulcerations extending from the anal verge to the anastomosis at 10 cm, with FC exceeding 8000 mcg/g, otherwise there was complete resolution of colitis proximal to the anastomosis. Suspecting ischemic injury related to prior anastomosis, HBOT was initiated –daily 2-hour session for 20 days. Clinical remission occurred within 2 weeks and was sustained for six months. Final flexible sigmoidoscopy 6 months later showed fully healed ulcers, with mild patchy erythema and inflammatory polyps.
Discussion: This was the first reported case of HBOT achieving complete clinical and endoscopic remission in refractory IMC associated with segmental ischemic injury at prior anastomosis. The case underscores HBOT’s potential as an adjunctive therapy in patients with concurrent immune and hypoxic-related inflammation.
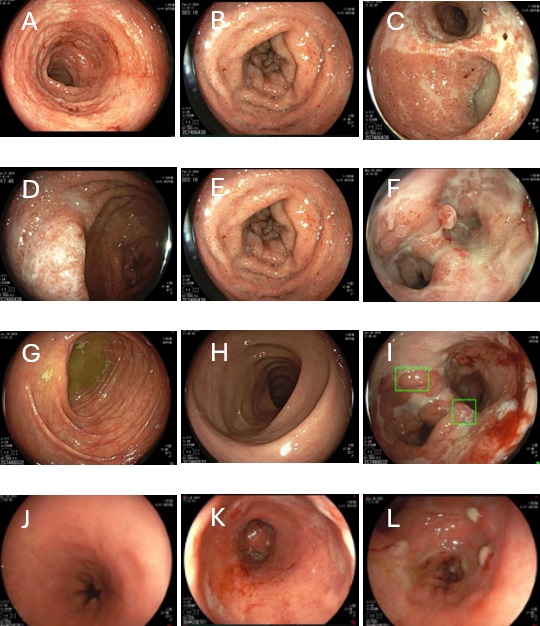
Figure: Diagnostic colonoscopy:
Baseline at IMDC diagnosis: A: Ascending colon B: Transverse colon C: Anastomosis area
Colonoscopy at 3 months after steroid and 3 doses of vedolizumab: D: Ascending colon E: Transverse colon F: Anastomosis area
Colonoscopy at 2 months after first FMT: G: Ascending colon H: Transverse colon I: Anastomosis area
Flexible sigmoidoscopy at six months post-HBOT: J: Splenic flexure showing normal mucosa K: Rectum with patchy erythema and healed ulcers L: Anastomosis with few inflammatory polyps
Disclosures:
Rohan Patel indicated no relevant financial relationships.
Carolina Cruz indicated no relevant financial relationships.
Maria Julia Santos indicated no relevant financial relationships.
Sharada Wali indicated no relevant financial relationships.
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Yinghong Wang indicated no relevant financial relationships.
Rohan Patel, 1, Carolina Cruz, MD2, Maria Julia M. N.. Santos, MD1, Sharada Wali, MBBS, MPH2, Krishnavathana Varatharajalu, MD1, Yinghong Wang, MD, PhD, MS2. P4708 - Hyperbaric Oxygen Therapy for Ischemic Colon Ulceration in a Patient With Immune-Mediated Colitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rohan Patel, 1, Carolina Cruz, MD2, Maria Julia M. N.. Santos, MD1, Sharada Wali, MBBS, MPH2, Krishnavathana Varatharajalu, MD1, Yinghong Wang, MD, PhD, MS2
1MD Anderson Cancer Center, Houston, TX; 2University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Immune checkpoint inhibitors (ICI) enhance antitumor T-cell responses, boosting immune function. However, they may trigger off-target inflammation mimicking autoimmunity, often manifesting as colitis. While clinical remission is commonly achieved with medical therapy, symptoms may persist in those with prior colorectal surgeries, particularly when anastomoses are located in vascular watershed areas prone to ischemia and reduced drug perfusion. Hyperbaric oxygen therapy (HBOT), which promotes angiogenesis and tissue oxygenation, has shown benefits in inflammatory bowel disease. We report a novel case of ICI-mediated colitis (IMC) with persistent rectal ulcers near the surgical anastomosis refractory to standard therapy, achieve mucosal healing with HBOT.
Case Description/
Methods: A 77-year-old female with stage II lung adenocarcinoma, status post right upper lobectomy, received carboplatin, pemetrexed, and subsequently 12 cycles of atezolizumab –discontinued due to toxicity. Her history also included diverticulitis managed with partial colectomy and anastomosis 4 years earlier. She developed grade 3 diarrhea and grade 2 colitis (CTCAE), with rectal bleeding. Colonoscopy revealed pancolitis (Mayo 3) with ulcerations, histologic inflammation, and fecal calprotectin (FC) of 2343 µg/g. Despite corticosteroids, three vedolizumab doses, and two fecal microbiota transplantations (FMT) with PuraStat spray over nine months, only partial relief was achieved, with persistent urgency and hematochezia. At the 2nd FMT, colonoscopy showed remaining large ulcerations extending from the anal verge to the anastomosis at 10 cm, with FC exceeding 8000 mcg/g, otherwise there was complete resolution of colitis proximal to the anastomosis. Suspecting ischemic injury related to prior anastomosis, HBOT was initiated –daily 2-hour session for 20 days. Clinical remission occurred within 2 weeks and was sustained for six months. Final flexible sigmoidoscopy 6 months later showed fully healed ulcers, with mild patchy erythema and inflammatory polyps.
Discussion: This was the first reported case of HBOT achieving complete clinical and endoscopic remission in refractory IMC associated with segmental ischemic injury at prior anastomosis. The case underscores HBOT’s potential as an adjunctive therapy in patients with concurrent immune and hypoxic-related inflammation.
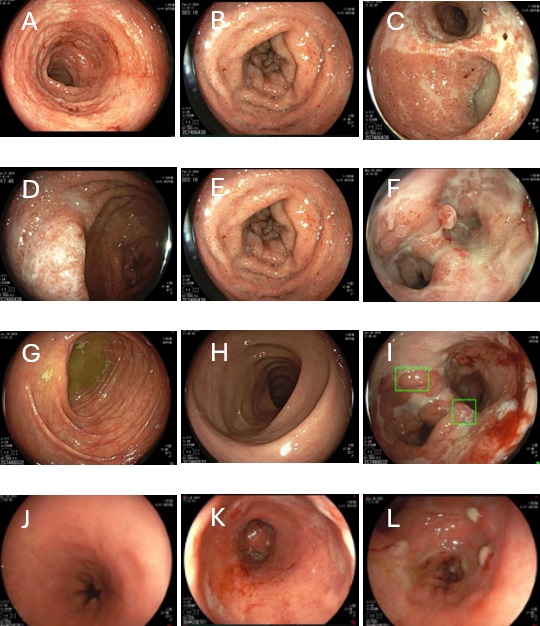
Figure: Diagnostic colonoscopy:
Baseline at IMDC diagnosis: A: Ascending colon B: Transverse colon C: Anastomosis area
Colonoscopy at 3 months after steroid and 3 doses of vedolizumab: D: Ascending colon E: Transverse colon F: Anastomosis area
Colonoscopy at 2 months after first FMT: G: Ascending colon H: Transverse colon I: Anastomosis area
Flexible sigmoidoscopy at six months post-HBOT: J: Splenic flexure showing normal mucosa K: Rectum with patchy erythema and healed ulcers L: Anastomosis with few inflammatory polyps
Disclosures:
Rohan Patel indicated no relevant financial relationships.
Carolina Cruz indicated no relevant financial relationships.
Maria Julia Santos indicated no relevant financial relationships.
Sharada Wali indicated no relevant financial relationships.
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Yinghong Wang indicated no relevant financial relationships.
Rohan Patel, 1, Carolina Cruz, MD2, Maria Julia M. N.. Santos, MD1, Sharada Wali, MBBS, MPH2, Krishnavathana Varatharajalu, MD1, Yinghong Wang, MD, PhD, MS2. P4708 - Hyperbaric Oxygen Therapy for Ischemic Colon Ulceration in a Patient With Immune-Mediated Colitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

