Tuesday Poster Session
Category: Colon
P4689 - A Rare Case of Lymphatic Malformations Presenting as Protein-Losing Enteropathy and Literature Review
Jacintha Thomas, DO (she/her/hers)
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
University of Nebraska Medical Center, Omaha, NE
Introduction:
Lymphatic malformations (LMs) are rare, benign tumors characterized by abnormal proliferation of lymphatic vessels. Abdominal LMs account for less than 5% of all LMs1. This is the first case of an adult with abdominal LMs causing protein-losing enteropathy that was treated with dietary changes alone.
Case Description/
Methods:
A 24-year-old female without significant past medical history presented with chronic diarrhea and weight loss. Labs showed hypoalbuminemia, low fecal calprotectin, normal fecal elastase, and elevated fecal Alpha-1-Antitrypsin (A1AT).
Abdominal computed tomography was concerning for mucinous carcinomatosis or pseudomyxoma peritonei with fluid signal involving the colon and pancreas (Figures 1A, 1B). Upper endoscopic ultrasound showed hyperechoic spaces surrounding the pancreas. Attempted aspiration of the spaces was unsuccessful. Colonoscopy showed an edematous cecum with the appearance of extrinsic compression. The biopsies from esophagogastroduodenoscopy and colonoscopy were negative.
An omental biopsy was negative for carcinomatosis but showed changes most consistent with a diagnosis of abdominal LMs (Figures 1C, 1D). With dietary changes, the patient reported 85-90% improvement in symptoms.
Discussion:
LMs can lead to impaired lymphatic drainage and dilation of lymphatic vessels (lymphangiectasia). Abdominal lymphangiectasias can lead to protein-losing enteropathy, resulting in hypoproteinemia and elevated fecal A1AT. Symptomatic patients are often treated with surgical resection or sclerotherapy1,2. For this patient, these interventions were not performed due to the diffuse nature of LMs with no identifiable cystic masses. For non-procedural candidates, Sirolimus (an mTOR inhibitor), which inhibits lymphangiogenesis, can be used2. To treat the protein-losing enteropathy, a low-fat, high-protein diet supplemented by medium chain triglycerides (MCTs) can be trialed. In this case, the patient experienced significant improvement in symptoms and stool burden with dietary changes.
In adults, abdominal LMs are often asymptomatic with the majority discovered incidentally1. Our literature review resulted only a handful of symptomatic adult cases, and all were managed surgically. This is the first reported adult case of protein-losing enteropathy due to abdominal LMs that was treated with dietary changes alone.
References:
- Hoang et al. Japanese Journal of Radiology. July 2022. 283-302.
- Leboulanger et al. Orthanet Journal of Rare Diseases. 2023. 18:10.
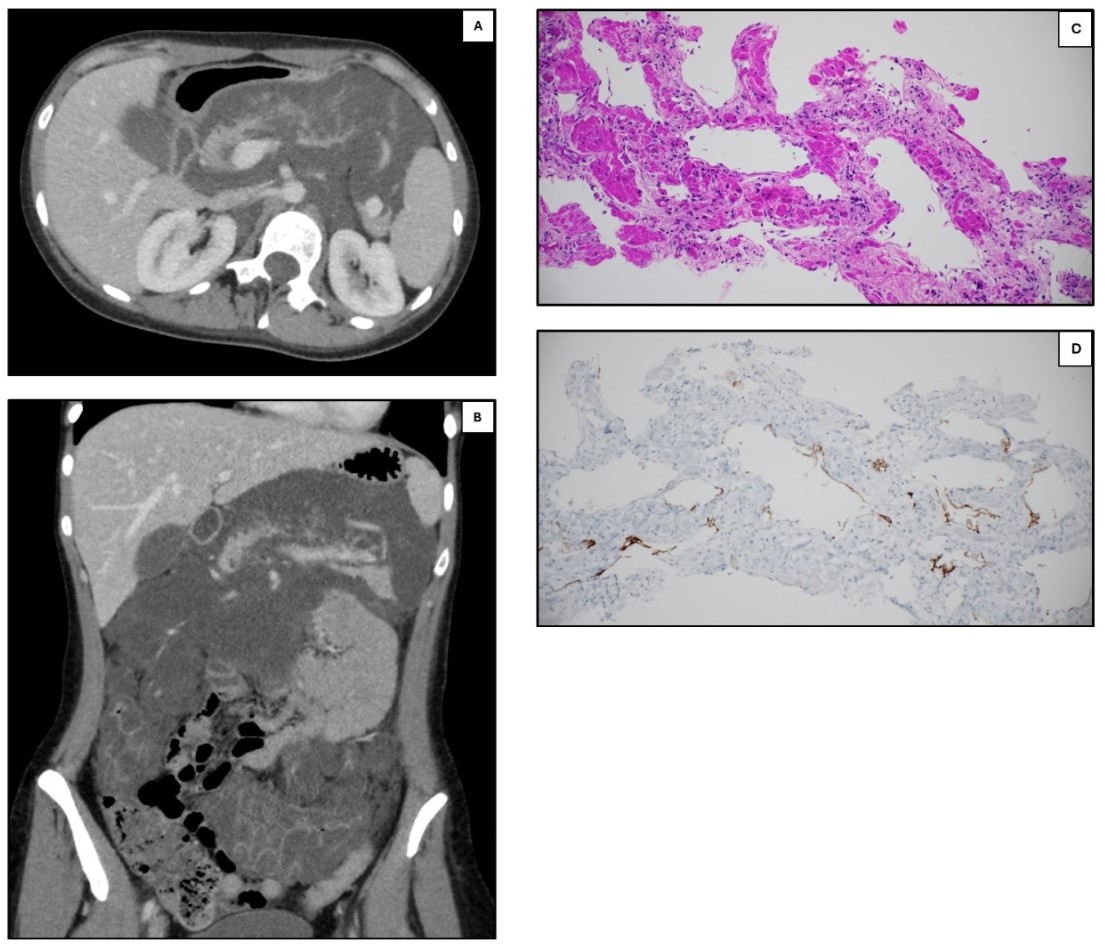
Figure: Figure 1. A. CT abdomen/pelvis (axial view) demonstrating extensive mucinous encasement of the pancreatic body. B. CT abdomen/pelvis (coronal view) demonstrating extensive mucinous encasement of the intraperitoneal portions of the transverse and ascending colon and involving and replacing the pancreatic body. C. This H&E slide shows dilated spaces lined by flattered endothelium consistent with lymphatic channels. The stroma surrounding the lymphatic channels has abundant smooth muscle that is brightly eosinophilic. D. This D2-40 stain, which highlights podoplanin, stains the lining of the dilated spaces confirming that these spaces are lymphatic channels.
Disclosures:
Jacintha Thomas indicated no relevant financial relationships.
Katerina Roma indicated no relevant financial relationships.
Ishfaq Bhat indicated no relevant financial relationships.
Jacintha Thomas, DO, Katerina Roma, DO, Ishfaq Bhat, MD. P4689 - A Rare Case of Lymphatic Malformations Presenting as Protein-Losing Enteropathy and Literature Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
