Tuesday Poster Session
Category: Colon
P4687 - Persistent Ulcerated Nodular Mucosa at the Hepatic Flexure: Diagnostic and Management Challenges in Indeterminate Colitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Oleksandr Shumeiko, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Oleksandr Shumeiko, MD1, Sue Dong, MD2, Raissa Nana Sede Mbakop Forlemu, MD1, Taranika Sarkar Das, MD1, Manasa Ginjupalli, MD1, Isaac Moshenyat, MD1, Madhavi Reddy, MD2
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Isolated and recurrent ulceration in the same colonic segment is rare and often diagnostically challenging. Focal indeterminate colitis, lacking definitive features of classic inflammatory bowel disease (IBD), raises questions about etiology and optimal management.
Case Description/
Methods: A 55-year-old female with hypertension and hyperlipidemia was referred for evaluation of colonic ulceration initially identified during screening colonoscopy in November 2022. The patient denied NSAID use and had no family history of IBD or GI malignancy. Findings included a localized area of ulcerated nodular mucosa at the hepatic flexure, with biopsy showing ulceration and focal mild active colitis. A tattoo was placed adjacent to the lesion for surveillance.
Subsequent colonoscopies in May 2023 and May 2024 revealed persistent ulcerated nodular mucosa at the same site, with minimal improvement. Histology evolved from mild active colitis to moderate-to-severe chronic active colitis with crypt microabscesses, but without granulomas, viral cytopathy, or dysplasia. Biopsies from the rest of the colon and terminal ileum remained normal.
She was intermittently symptomatic with loose stools, which improved with mesalamine therapy and eradication of Helicobacter pylori gastritis confirmed by stool antigen testing. Fecal calprotectin during symptoms was within normal limits. She is remained asymptomatic off mesalamine, under clinical surveillance.
Discussion: This case illustrates a persistent, isolated, non-granulomatous colonic ulcer with a chronic inflammatory pattern localized to the hepatic flexure. The histologic progression without clinical deterioration suggests a stable, non-neoplastic process. Differential diagnoses include focal drug-induced colitis (e.g., prior NSAID use), segmental colitis associated with diverticulosis, or an indolent, localized form of IBD.
The interplay between mesalamine discontinuation, H. pylori treatment, and symptom resolution complicates causal inference. The patient’s consistently normal calprotectin and lack of systemic symptoms further support a localized process rather than systemic IBD.
Recurrent localized colonic ulceration in the absence of systemic features or progressive histologic dysplasia represents a diagnostic and therapeutic gray zone. This case supports a conservative management approach with symptom-guided therapy and interval endoscopic surveillance, highlighting the importance of close clinical monitoring in focal indeterminate colitis.
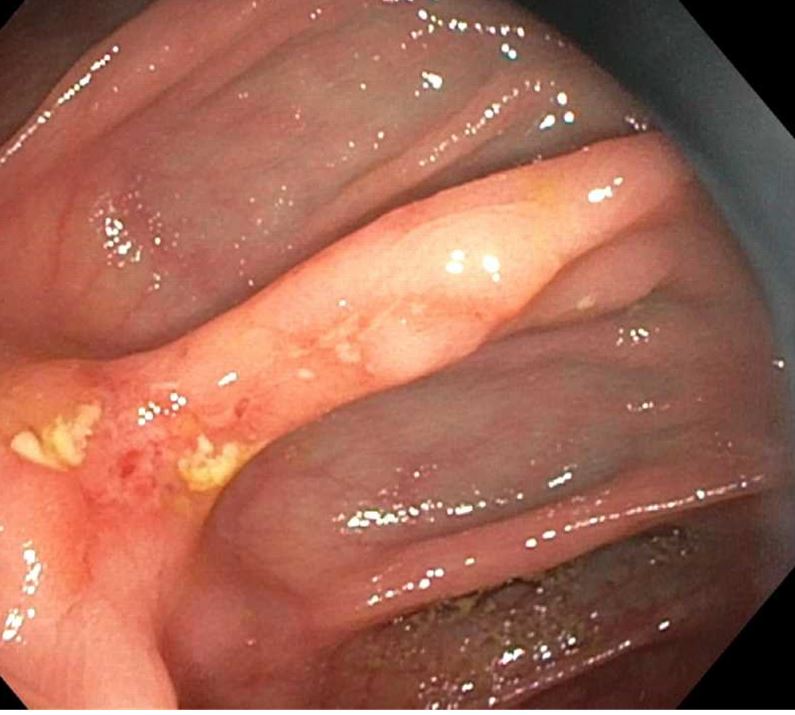
Figure: Ulcerated nodular mucosa at the hepatic flexure with biopsy showing ulceration and focal mild active colitis. A tattoo was placed adjacent to the lesion for surveillance.
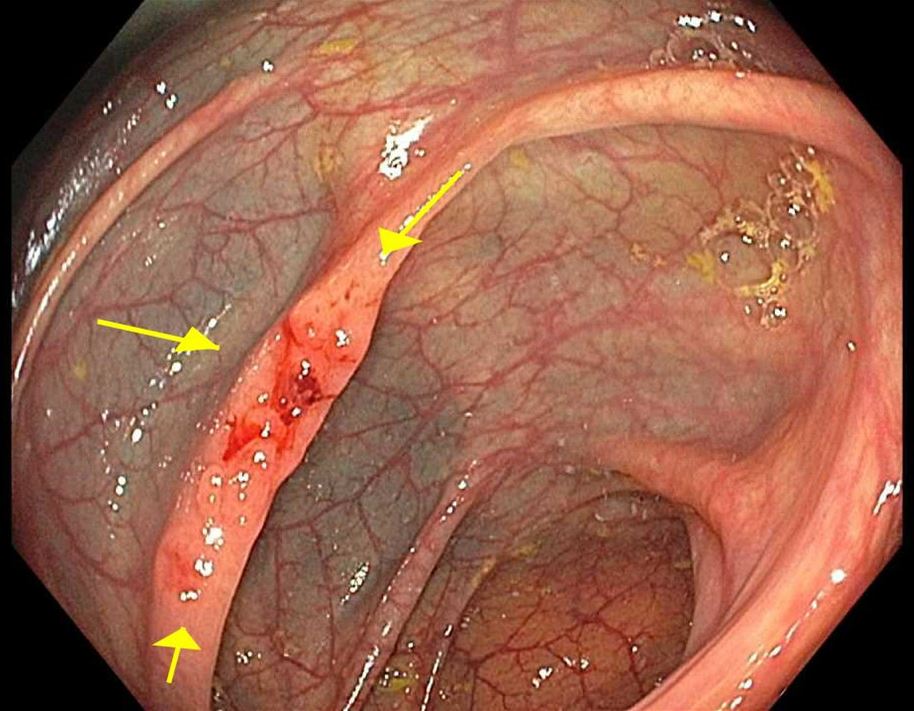
Figure: Persistent ulceration on the second surveillance colonoscopy
Disclosures:
Oleksandr Shumeiko indicated no relevant financial relationships.
Sue Dong indicated no relevant financial relationships.
Raissa Nana Sede Mbakop Forlemu indicated no relevant financial relationships.
Taranika Sarkar Das indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Isaac Moshenyat indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Oleksandr Shumeiko, MD1, Sue Dong, MD2, Raissa Nana Sede Mbakop Forlemu, MD1, Taranika Sarkar Das, MD1, Manasa Ginjupalli, MD1, Isaac Moshenyat, MD1, Madhavi Reddy, MD2. P4687 - Persistent Ulcerated Nodular Mucosa at the Hepatic Flexure: Diagnostic and Management Challenges in Indeterminate Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Isolated and recurrent ulceration in the same colonic segment is rare and often diagnostically challenging. Focal indeterminate colitis, lacking definitive features of classic inflammatory bowel disease (IBD), raises questions about etiology and optimal management.
Case Description/
Methods: A 55-year-old female with hypertension and hyperlipidemia was referred for evaluation of colonic ulceration initially identified during screening colonoscopy in November 2022. The patient denied NSAID use and had no family history of IBD or GI malignancy. Findings included a localized area of ulcerated nodular mucosa at the hepatic flexure, with biopsy showing ulceration and focal mild active colitis. A tattoo was placed adjacent to the lesion for surveillance.
Subsequent colonoscopies in May 2023 and May 2024 revealed persistent ulcerated nodular mucosa at the same site, with minimal improvement. Histology evolved from mild active colitis to moderate-to-severe chronic active colitis with crypt microabscesses, but without granulomas, viral cytopathy, or dysplasia. Biopsies from the rest of the colon and terminal ileum remained normal.
She was intermittently symptomatic with loose stools, which improved with mesalamine therapy and eradication of Helicobacter pylori gastritis confirmed by stool antigen testing. Fecal calprotectin during symptoms was within normal limits. She is remained asymptomatic off mesalamine, under clinical surveillance.
Discussion: This case illustrates a persistent, isolated, non-granulomatous colonic ulcer with a chronic inflammatory pattern localized to the hepatic flexure. The histologic progression without clinical deterioration suggests a stable, non-neoplastic process. Differential diagnoses include focal drug-induced colitis (e.g., prior NSAID use), segmental colitis associated with diverticulosis, or an indolent, localized form of IBD.
The interplay between mesalamine discontinuation, H. pylori treatment, and symptom resolution complicates causal inference. The patient’s consistently normal calprotectin and lack of systemic symptoms further support a localized process rather than systemic IBD.
Recurrent localized colonic ulceration in the absence of systemic features or progressive histologic dysplasia represents a diagnostic and therapeutic gray zone. This case supports a conservative management approach with symptom-guided therapy and interval endoscopic surveillance, highlighting the importance of close clinical monitoring in focal indeterminate colitis.
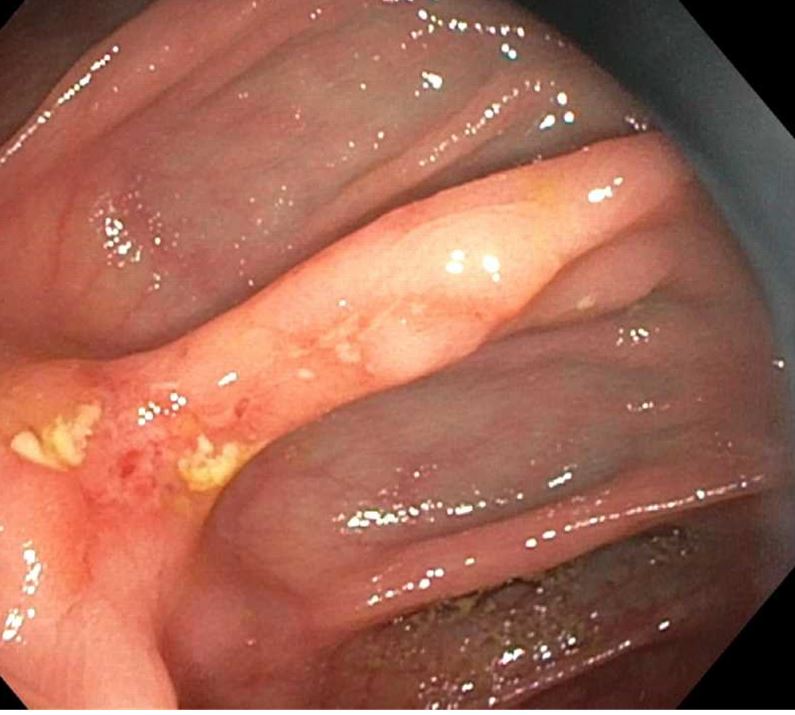
Figure: Ulcerated nodular mucosa at the hepatic flexure with biopsy showing ulceration and focal mild active colitis. A tattoo was placed adjacent to the lesion for surveillance.
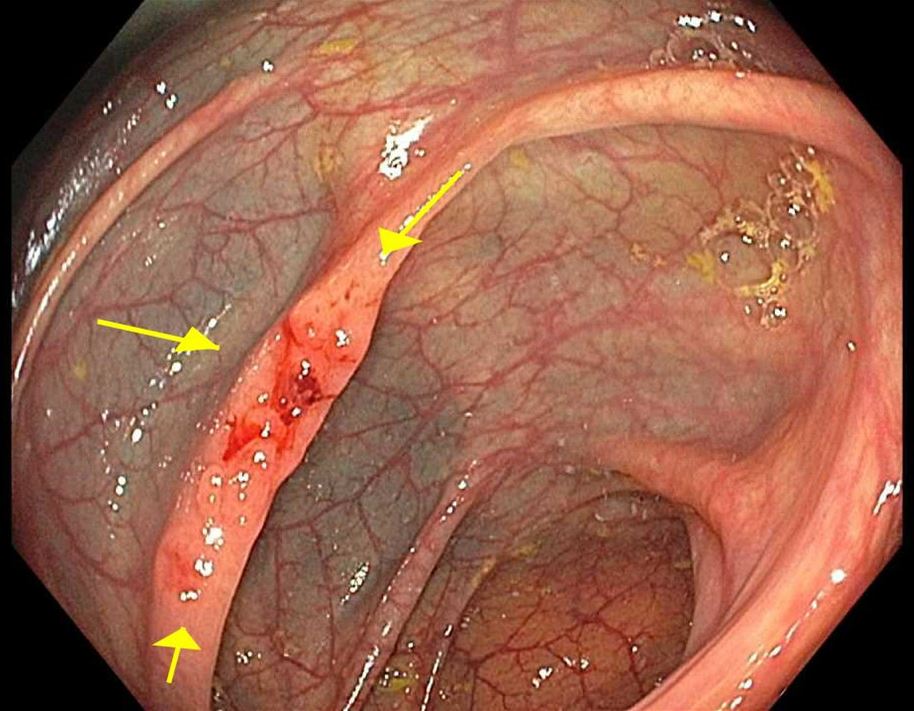
Figure: Persistent ulceration on the second surveillance colonoscopy
Disclosures:
Oleksandr Shumeiko indicated no relevant financial relationships.
Sue Dong indicated no relevant financial relationships.
Raissa Nana Sede Mbakop Forlemu indicated no relevant financial relationships.
Taranika Sarkar Das indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Isaac Moshenyat indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Oleksandr Shumeiko, MD1, Sue Dong, MD2, Raissa Nana Sede Mbakop Forlemu, MD1, Taranika Sarkar Das, MD1, Manasa Ginjupalli, MD1, Isaac Moshenyat, MD1, Madhavi Reddy, MD2. P4687 - Persistent Ulcerated Nodular Mucosa at the Hepatic Flexure: Diagnostic and Management Challenges in Indeterminate Colitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
