Tuesday Poster Session
Category: Colon
P4683 - From Incidental to Alarming: Hematochezia and Constipation Due to a Progressing Colonic Lipoma

Jai Kumar, MD
Wayne State University School of Medicine / Ascension Providence Rochester Hospital
Rochester, MI
Presenting Author(s)
1Wayne State University School of Medicine / Ascension Providence Rochester Hospital, Rochester, MI; 2Ascension St. John Hospital, Macomb, MI
Introduction: Colonic lipomas are benign submucosal tumors found in ~0.2–4.4% of colonoscopies. Most are < 2 cm, asymptomatic, and incidentally discovered. Larger lesions ( >2 cm) may cause pain, bleeding, or obstruction, and can mimic malignancy, especially when ulcerated or causing mucosal distortion.
Case Description/
Methods:
In May 2024, a 48-year-old man with a family history of colonic polyps and a personal history of intermittent hematochezia underwent diagnostic colonoscopy. His bleeding episodes were infrequent, self-limited, and without chronic bowel issues or weight loss.
Colonoscopy revealed a smooth, 3 cm sessile submucosal lesion in the ascending colon and two small polyps—one in the descending colon and one in the sigmoid. Internal hemorrhoids were also visualized. The distal ileal and colonic mucosa appeared normal. Hemorrhoids were presumed the likely cause of his intermittent bleeding.
Biopsies confirmed the ascending colonic lesion as a submucosal lipoma—benign adipose tissue without dysplasia or malignancy. Polyp histology was hyperplastic.
In October 2024, he was hospitalized with persistent hematochezia. Hemodynamically stable, his labs showed a modest hemoglobin drop suggesting acute blood loss. Contrast-enhanced CT abdomen showed sigmoid wall thickening, pericolonic fat stranding, punctate extraluminal gas, and proximal air-stool levels—raising concern for colitis, ischemia, or a submucosal mass.
In March 2025, repeat colonoscopy revealed that the 3 cm lipoma now had central ulceration with contact oozing. No other bleeding source was found. Multiple biopsies were obtained.
Histopathology showed focal ulceration and granulation tissue without dysplasia, malignancy, or chronic colitis—consistent with an ulcerated colonic lipoma, now recognized as the bleeding and obstruction source. Although bleeding resolved without transfusion, the ulceration and symptoms prompted referral for endoscopic submucosal dissection (ESD).
Discussion: Colonic lipomas, found in 0.2–4.4% of benign colonic tumors, are usually incidental. Lesions >2 cm may cause bleeding, intussusception, or obstruction. Mucosal ulceration can mimic malignancy. Our case highlights the need to reassess lipomas when new symptoms emerge.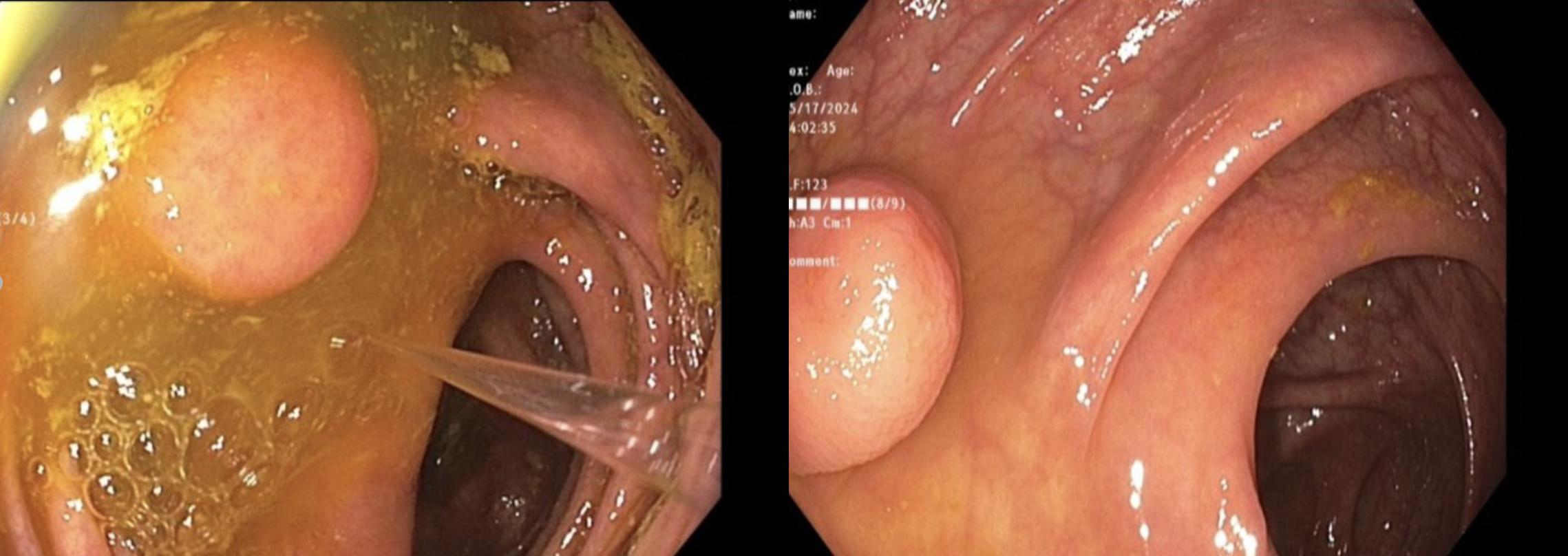
Figure: Endoscopic images from May 2024 showing a smooth, pedunculated 3 cm submucosal lesion consistent with colonic lipoma, without ulceration. 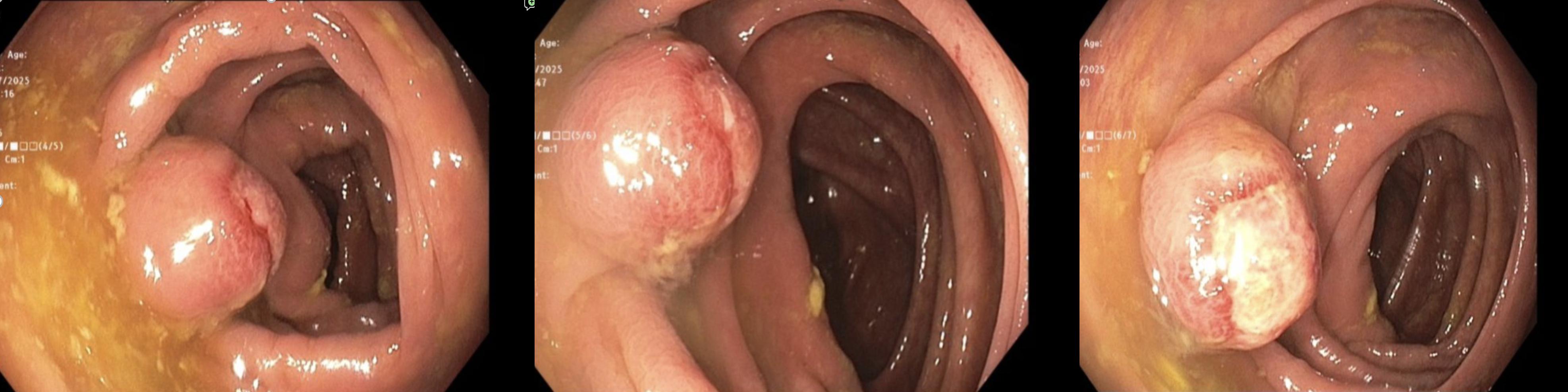
Figure: Endoscopic images from March 2025 showing an enlarged 3 cm colonic lipoma with surface ulceration and erythema, consistent with pressure necrosis and source of lower GI bleeding.
Disclosures:
Jai Kumar indicated no relevant financial relationships.
Leonid Shamban indicated no relevant financial relationships.
Jai Kumar, MD1, Leonid Shamban, DO2. P4683 - From Incidental to Alarming: Hematochezia and Constipation Due to a Progressing Colonic Lipoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
