Tuesday Poster Session
Category: Colon
P4644 - Beyond the Surface: When Colonoscopy Leads to Newly Diagnosed Endometriosis With Colonic Infiltration
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rhett Harmon, MD (he/him/his)
Olive View-UCLA Medical Center
Los Angeles, CA
Presenting Author(s)
Rhett Harmon, MD1, Mark R. Baniqued, MD1, Firas Bahdi, MD2, Deepthi Karunasiri, MD3, Shaun Chandna, DO3, Payman Fathizadeh, MD3
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Twenty percent of women with endometriosis develop infiltration into surrounding structures in the pelvis and retroperitoneum. Colorectal endometriosis (CE) is a subtype that often impacts the rectosigmoid. While usually asymptomatic, CE can present with intermittent hematochezia or bowel obstruction, highlighting the need for early diagnosis and management. We present a case of sigmoid stenosis, due to colonic endometriosis, as first presentation of endometriosis in a patient without gastrointestinal symptoms.
Case Description/
Methods:
A 47-year-old woman was referred for colonoscopy after positive fecal immunochemical test. She denied abdominal pain, hematochezia, bowel habit changes, or weight loss. Colonoscopy revealed 5 cm moderate sigmoid stricture with distal mucosal irregularity concerning for though not overtly malignant. The stricture was traversable. Biopsies initially revealed sessile serrated lesion changes with low grade dysplasia and ultimately a small focus of endometriosis. The serrated changes in correlation are suspected to be reactive due to the underlying submucosal endometriosis. Endometriosis was confirmed by immunohistochemical staining positive for PAX8, ER, and CD10 markers. CT identified redundant sigmoid with narrowing adjacent to right adnexa/uterus and new right adnexal cysts 4.6 cm in size. No obvious invasion into bowel. Pelvic ultrasound showed 5.1 cm right adnexal cystic mass favored to be ovarian. Multidisciplinary discussion with gynecology-oncology favored medical therapy with oral contraceptive pills (OCPs). She has had dysmenorrhea treated with NSAIDs, prior hormonal contraception intolerance, no menorrhagia. Surveillance colonoscopy and EGD for iron deficiency planned.
Discussion: Colorectal endometriosis typically presents with cyclical symptoms that worsen during menstruation, including abdominal pain, dyschezia, hematochezia, and altered bowel habits. Endoscopically, CE can mimic malignancy or irregular stricture in the rectosigmoid. The subepithelial nature of the disease poses a challenge during tissue acquisition, as biopsies may not yield the diagnosis. Techniques such as transvaginal/transrectal US, MRI, and barium enema can assist in determining disease location and extent. Initial treatment of mild-moderate non-obstructive cases includes hormonal suppression with OCPs or progestins, with about two-thirds of patients finding relief. Surgical intervention is reserved for severe bowel obstruction or when medical therapy fails to control symptoms.
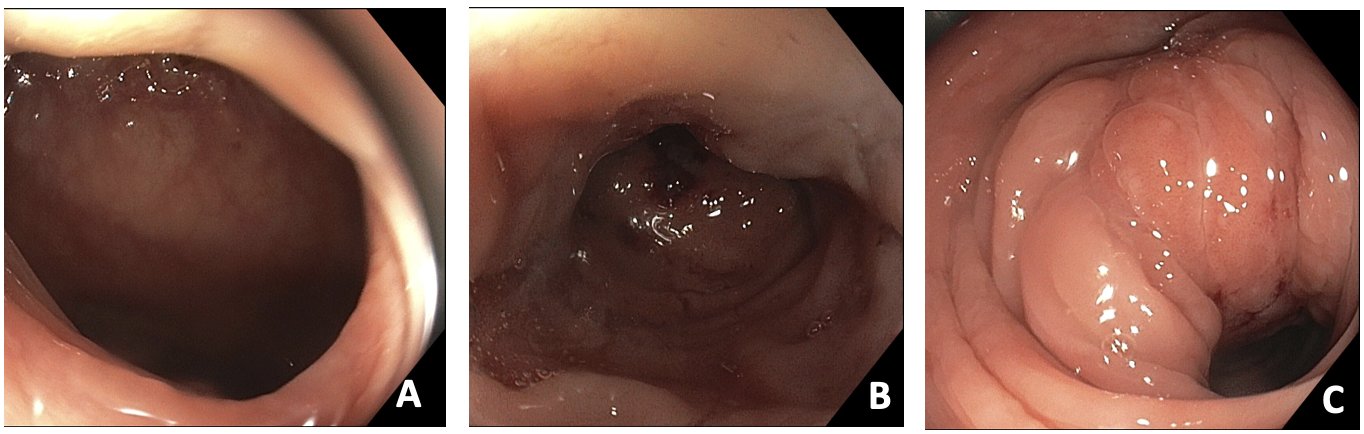
Figure: Biopsies obtained from the sigmoid stricture and irregularity demonstrate multiple fragments of colonic mucosa exhibiting reactive epithelial changes, with focal areas displaying hyperplastic features. Scattered minute atypical foci are identified within the specimens (A). Examination of the atypical foci reveals ectopic endometrial tissue (B) characterized by endometrial stroma (b1) and endometrial glands (b2) replacing the native colonic mucosa. Immunohistochemical staining for PAX8 (Paired Box Gene 8) confirms the presence of endometrial epithelial cells (C) infiltrating and replacing the colonic mucosa.
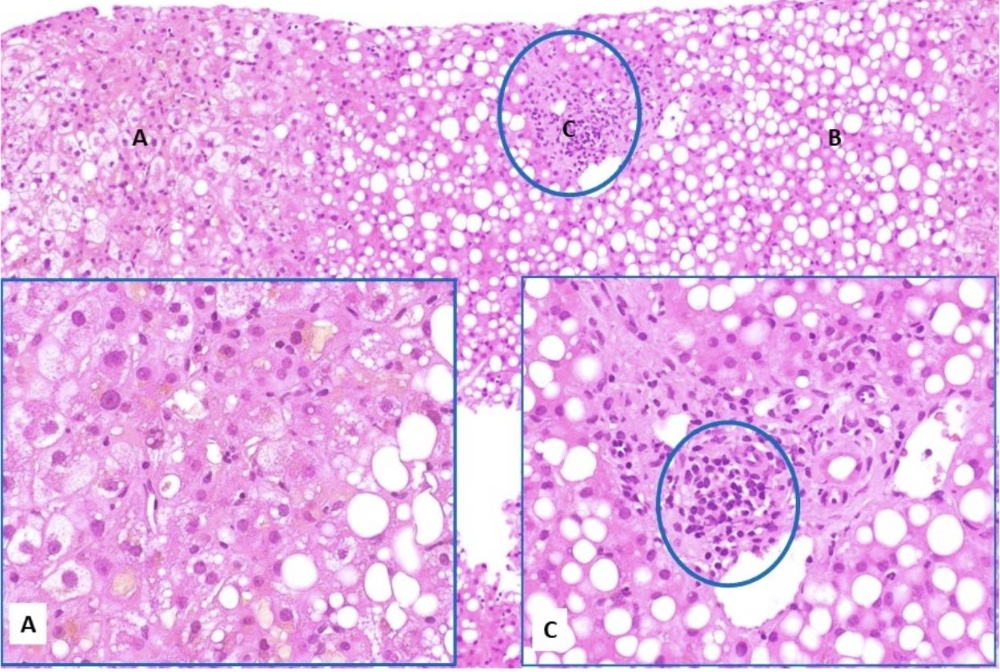
Figure: A: Proximal end of sigmoid stenosis
B: Middle end of sigmoid stenosis
C: Distal end of sigmoid stenosis with mucosal irregularity
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Mark Baniqued indicated no relevant financial relationships.
Firas Bahdi indicated no relevant financial relationships.
Deepthi Karunasiri indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Payman Fathizadeh indicated no relevant financial relationships.
Rhett Harmon, MD1, Mark R. Baniqued, MD1, Firas Bahdi, MD2, Deepthi Karunasiri, MD3, Shaun Chandna, DO3, Payman Fathizadeh, MD3. P4644 - Beyond the Surface: When Colonoscopy Leads to Newly Diagnosed Endometriosis With Colonic Infiltration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Los Angeles, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3Olive View-UCLA Medical Center, Sylmar, CA
Introduction: Twenty percent of women with endometriosis develop infiltration into surrounding structures in the pelvis and retroperitoneum. Colorectal endometriosis (CE) is a subtype that often impacts the rectosigmoid. While usually asymptomatic, CE can present with intermittent hematochezia or bowel obstruction, highlighting the need for early diagnosis and management. We present a case of sigmoid stenosis, due to colonic endometriosis, as first presentation of endometriosis in a patient without gastrointestinal symptoms.
Case Description/
Methods:
A 47-year-old woman was referred for colonoscopy after positive fecal immunochemical test. She denied abdominal pain, hematochezia, bowel habit changes, or weight loss. Colonoscopy revealed 5 cm moderate sigmoid stricture with distal mucosal irregularity concerning for though not overtly malignant. The stricture was traversable. Biopsies initially revealed sessile serrated lesion changes with low grade dysplasia and ultimately a small focus of endometriosis. The serrated changes in correlation are suspected to be reactive due to the underlying submucosal endometriosis. Endometriosis was confirmed by immunohistochemical staining positive for PAX8, ER, and CD10 markers. CT identified redundant sigmoid with narrowing adjacent to right adnexa/uterus and new right adnexal cysts 4.6 cm in size. No obvious invasion into bowel. Pelvic ultrasound showed 5.1 cm right adnexal cystic mass favored to be ovarian. Multidisciplinary discussion with gynecology-oncology favored medical therapy with oral contraceptive pills (OCPs). She has had dysmenorrhea treated with NSAIDs, prior hormonal contraception intolerance, no menorrhagia. Surveillance colonoscopy and EGD for iron deficiency planned.
Discussion: Colorectal endometriosis typically presents with cyclical symptoms that worsen during menstruation, including abdominal pain, dyschezia, hematochezia, and altered bowel habits. Endoscopically, CE can mimic malignancy or irregular stricture in the rectosigmoid. The subepithelial nature of the disease poses a challenge during tissue acquisition, as biopsies may not yield the diagnosis. Techniques such as transvaginal/transrectal US, MRI, and barium enema can assist in determining disease location and extent. Initial treatment of mild-moderate non-obstructive cases includes hormonal suppression with OCPs or progestins, with about two-thirds of patients finding relief. Surgical intervention is reserved for severe bowel obstruction or when medical therapy fails to control symptoms.
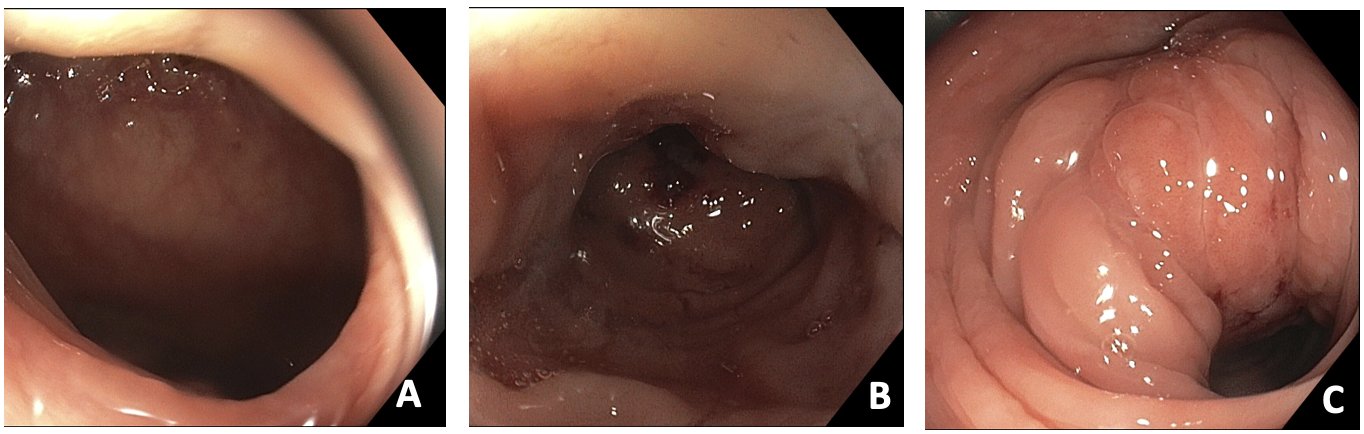
Figure: Biopsies obtained from the sigmoid stricture and irregularity demonstrate multiple fragments of colonic mucosa exhibiting reactive epithelial changes, with focal areas displaying hyperplastic features. Scattered minute atypical foci are identified within the specimens (A). Examination of the atypical foci reveals ectopic endometrial tissue (B) characterized by endometrial stroma (b1) and endometrial glands (b2) replacing the native colonic mucosa. Immunohistochemical staining for PAX8 (Paired Box Gene 8) confirms the presence of endometrial epithelial cells (C) infiltrating and replacing the colonic mucosa.
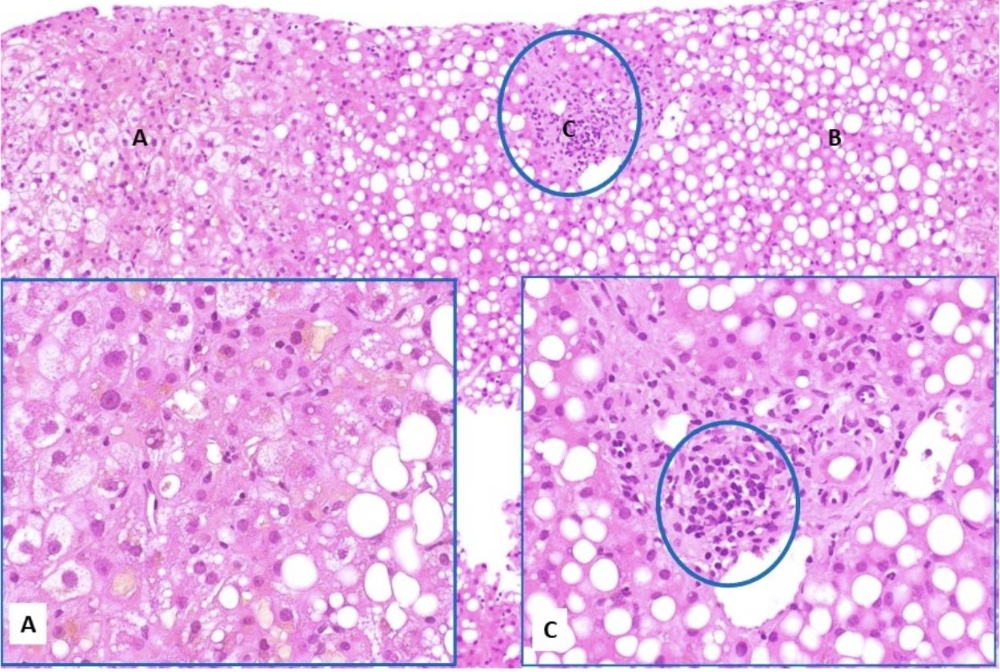
Figure: A: Proximal end of sigmoid stenosis
B: Middle end of sigmoid stenosis
C: Distal end of sigmoid stenosis with mucosal irregularity
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Mark Baniqued indicated no relevant financial relationships.
Firas Bahdi indicated no relevant financial relationships.
Deepthi Karunasiri indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Ipsen – Consultant. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Consultant, Grant/Research Support.
Payman Fathizadeh indicated no relevant financial relationships.
Rhett Harmon, MD1, Mark R. Baniqued, MD1, Firas Bahdi, MD2, Deepthi Karunasiri, MD3, Shaun Chandna, DO3, Payman Fathizadeh, MD3. P4644 - Beyond the Surface: When Colonoscopy Leads to Newly Diagnosed Endometriosis With Colonic Infiltration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
