Tuesday Poster Session
Category: Colon
P4643 - Primary Anorectal Melanoma: An Unexpected Finding During Colorectal Cancer Surveillance
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ruchir Paladiya, MBBS
University of Connecticut School of Medicine
Farmington, CT
Presenting Author(s)
Ruchir Paladiya, MBBS1, Khushi Gadhia, MBBS2, John Wysocki, MD3
1University of Connecticut School of Medicine, Farmington, CT; 2Pramukhswami Medical College, Hartford, CT; 3University of Connecticut Health Center, Hartford, CT
Introduction: Anorectal melanoma is a rare and aggressive cancer, comprising less than 1% of all melanomas and 0.4–1.6% of anorectal malignancies. Its nonspecific symptoms often mimic benign conditions and delay diagnosis. The disease typically has a poor prognosis, with a median survival of two years. Herein, we present a case of asymptomatic anorectal melanoma identified during routine surveillance colonoscopy.
Case Description/
Methods: A 57-year-old man with a first-degree family history of colorectal cancer underwent screening colonoscopy in 2019, which revealed diverticulosis, non-bleeding hemorrhoids, and a small hyperplastic polyp. A five-year follow-up was recommended. On repeat colonoscopy in April 2024, a 20 mm sessile polyp was noted at the anorectal junction and was removed. Histopathology revealed sheets of atypical melanocytic cells with prominent nucleoli and brisk mitosis. Immunohistochemical staining was positive for S100, SOX10, HMB-45, MART-1, CD10, and focal CD117, which is consistent with malignant melanoma. Glandular dysplasia was not observed.
CT and MRI imaging revealed benign-appearing hepatic, splenic, and renal cysts, along with indeterminate lesions in the right kidney and liver, but no definitive metastatic disease. PET/CT showed physiological rectal uptake without distant malignancy. Physical examination results were unremarkable. The case was discussed by a multidisciplinary tumor board. The patient was referred for further evaluation of the indeterminate lesions and systemic chemotherapy.
Discussion: Owing to its subtle presentation, anorectal melanoma is frequently diagnosed at advanced stages, with a five-year survival rate below 20%. Diagnosis requires biopsy and confirmation of melanocytic markers. Historically managed with abdominoperineal resection, treatment has shifted toward wide local excision when feasible. Immunotherapy, particularly immune checkpoint inhibitors, is increasingly used in advanced or metastatic anorectal melanoma and may improve survival in select patients, but its benefit in the adjuvant or neoadjuvant setting for resected localized disease remains unproven and is an area of ongoing investigation.
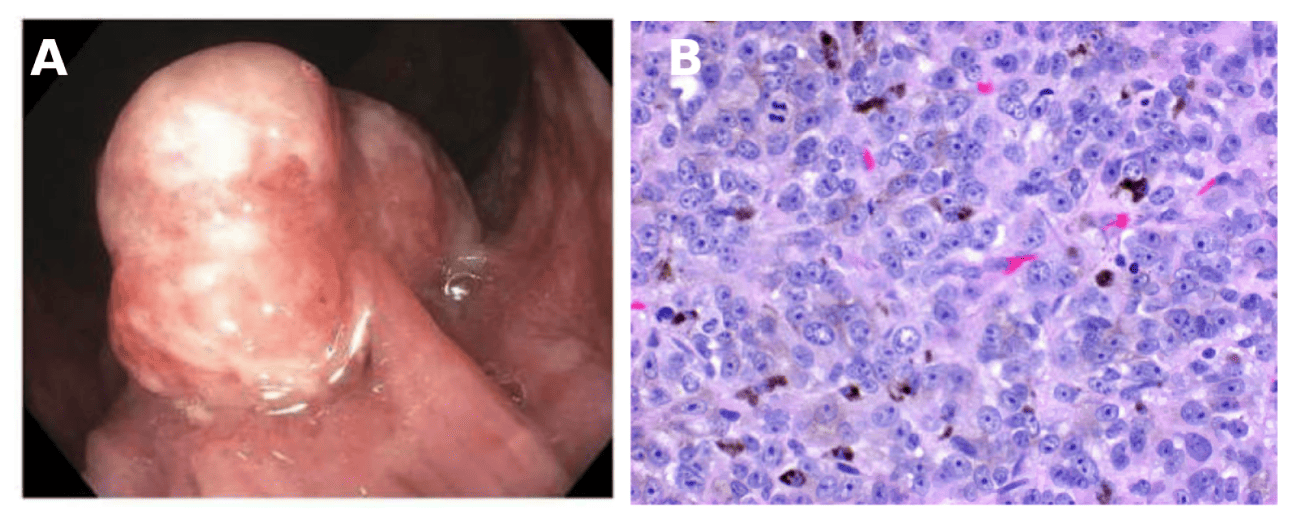
Figure: Figure A: Endoscopic view of a 20 mm polypoid mass at the anorectal junction.
Figure B: High-power view of a primary anorectal melanoma on hematoxylin and eosin stain. The image demonstrates intracellular melanin pigment, atypical hyperchromatic nuclei, and a mitotic figure, consistent with malignant melanoma.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Khushi Gadhia indicated no relevant financial relationships.
John Wysocki indicated no relevant financial relationships.
Ruchir Paladiya, MBBS 1, Khushi Gadhia, MBBS2, John Wysocki, MD3. P4643 - Primary Anorectal Melanoma: An Unexpected Finding During Colorectal Cancer Surveillance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ:American College of Gastroenterology.
1University of Connecticut School of Medicine, Farmington, CT; 2Pramukhswami Medical College, Hartford, CT; 3University of Connecticut Health Center, Hartford, CT
Introduction: Anorectal melanoma is a rare and aggressive cancer, comprising less than 1% of all melanomas and 0.4–1.6% of anorectal malignancies. Its nonspecific symptoms often mimic benign conditions and delay diagnosis. The disease typically has a poor prognosis, with a median survival of two years. Herein, we present a case of asymptomatic anorectal melanoma identified during routine surveillance colonoscopy.
Case Description/
Methods: A 57-year-old man with a first-degree family history of colorectal cancer underwent screening colonoscopy in 2019, which revealed diverticulosis, non-bleeding hemorrhoids, and a small hyperplastic polyp. A five-year follow-up was recommended. On repeat colonoscopy in April 2024, a 20 mm sessile polyp was noted at the anorectal junction and was removed. Histopathology revealed sheets of atypical melanocytic cells with prominent nucleoli and brisk mitosis. Immunohistochemical staining was positive for S100, SOX10, HMB-45, MART-1, CD10, and focal CD117, which is consistent with malignant melanoma. Glandular dysplasia was not observed.
CT and MRI imaging revealed benign-appearing hepatic, splenic, and renal cysts, along with indeterminate lesions in the right kidney and liver, but no definitive metastatic disease. PET/CT showed physiological rectal uptake without distant malignancy. Physical examination results were unremarkable. The case was discussed by a multidisciplinary tumor board. The patient was referred for further evaluation of the indeterminate lesions and systemic chemotherapy.
Discussion: Owing to its subtle presentation, anorectal melanoma is frequently diagnosed at advanced stages, with a five-year survival rate below 20%. Diagnosis requires biopsy and confirmation of melanocytic markers. Historically managed with abdominoperineal resection, treatment has shifted toward wide local excision when feasible. Immunotherapy, particularly immune checkpoint inhibitors, is increasingly used in advanced or metastatic anorectal melanoma and may improve survival in select patients, but its benefit in the adjuvant or neoadjuvant setting for resected localized disease remains unproven and is an area of ongoing investigation.
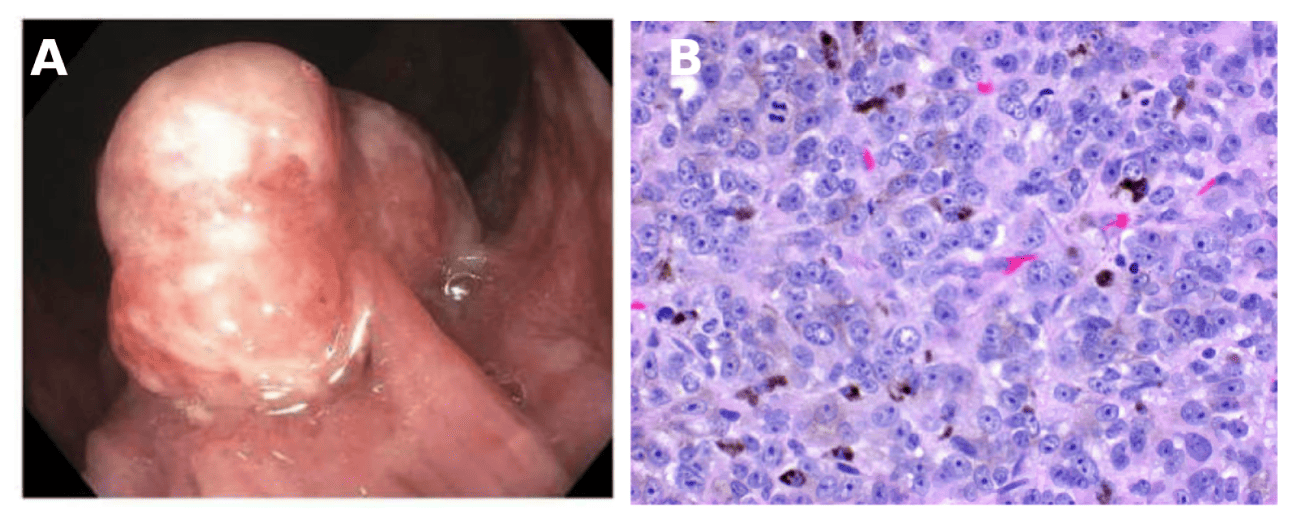
Figure: Figure A: Endoscopic view of a 20 mm polypoid mass at the anorectal junction.
Figure B: High-power view of a primary anorectal melanoma on hematoxylin and eosin stain. The image demonstrates intracellular melanin pigment, atypical hyperchromatic nuclei, and a mitotic figure, consistent with malignant melanoma.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Khushi Gadhia indicated no relevant financial relationships.
John Wysocki indicated no relevant financial relationships.
Ruchir Paladiya, MBBS 1, Khushi Gadhia, MBBS2, John Wysocki, MD3. P4643 - Primary Anorectal Melanoma: An Unexpected Finding During Colorectal Cancer Surveillance, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ:American College of Gastroenterology.
