Tuesday Poster Session
Category: Liver
P5990 - From Tolerance to Toxicity: Flares of Alcohol-Related Liver Injury Post-Sleeve Gastrectomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mehak Mastoi, MD
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Mehak Mastoi, MD1, Chidiebele Omaliko, MD2, Adedeji Adenusi, MD, MPH1, Abdelaziz Mohamed, MBBS1, Cherif El Younis, MD2
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY
Introduction: Bariatric surgery reduces first-pass hepatic metabolism and raises peak blood alcohol concentrations, therefore changing alcohol pharmacokinetics. Although this is generally known, there is less information on the clinical effects of modest alcohol intake following surgery without past liver disease. We present a case of intermittent alcohol use-induced flares of hepatitis following sleeve gastrectomy. This case emphasizes the potential for increased hepatotoxicity in this demographic.
Case Description/
Methods: A 52-year-old male with morbid obesity and hyperlipidemia underwent laparoscopic sleeve gastrectomy (LSG) in June 2022. He used to drink 42 drinks a week before surgery and showed little indication of liver injury and required no admission for alcoholic liver disease. One year after bariatric surgery, he was repeatedly hospitalized and had frequent emergency visits for abdominal pain and jaundice with minimal alcohol consumption of three beers a week.
Laboratory findings showed elevated liver enzymes during the 2024 hospitalizations, with bilirubin up to 41 mg/dL, AST 358 U/L, ALP 309 U/L, and INR 1.92 after a single episode of weekend alcohol use. Maddrey Discriminant Function (MDF) was 58.4, and his MELD-3 was 26. Ethanol concentration was negligible. His imaging revealed hepatic steatosis without cirrhosis or biliary obstruction. Autoimmune, metabolic, and infectious workups were negative. His liver injury episodes were more severe and more frequent with flares of alcoholic hepatitis, even though he consumed much less alcohol postoperatively.
Discussion: This case demonstrates increased sensitivity to alcohol-induced liver injury after sleeve gastrectomy, mainly due to a 50-70% reduction in gastric alcohol dehydrogenase enzyme (ADH) activity following LSG. This reduction lowers first-pass metabolism, resulting in higher blood alcohol levels and increased liver exposure to toxic metabolites. Consequently, even small amounts of alcohol can trigger severe hepatotoxicity.
Although bariatric surgery lowers steatosis and metabolic dysfunction-associated steatosis (MASH), therefore improving liver health, it paradoxically raises the risk of alcohol-related steatohepatitis. Up to 5% of patients develop alcohol-associated liver disease, and 33% develop problematic drinking post-surgery.
Clinicians should emphasize the selection process for bariatric surgery, identifying high-risk patients, counseling on complete alcohol abstinence, and close social support to reduce this phenomenon.
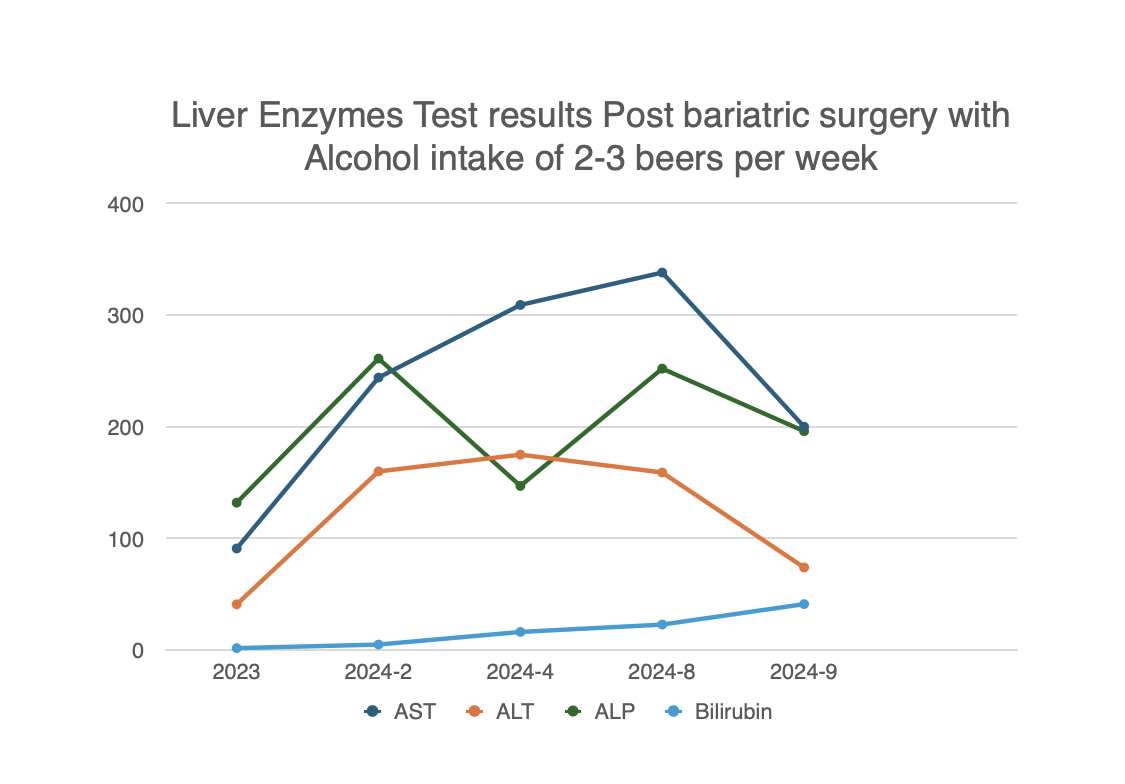
Figure: Liver Enzymes Results Prior to Bariatric Surgery with Alcohol intake of 42 beers per week
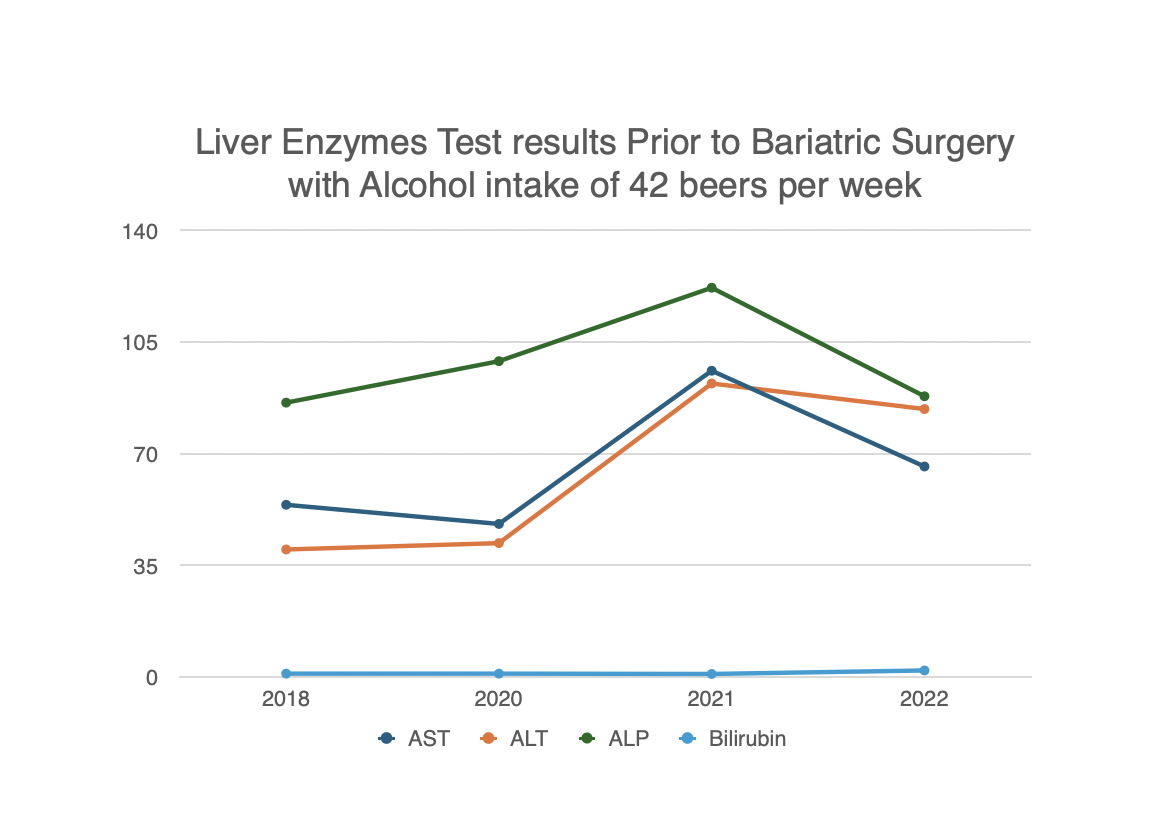
Figure: Liver Enzymes results Post Bariatric surgery with alcohol intake of 2-3 beers per week
Disclosures:
Mehak Mastoi indicated no relevant financial relationships.
Chidiebele Omaliko indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Cherif El Younis indicated no relevant financial relationships.
Mehak Mastoi, MD1, Chidiebele Omaliko, MD2, Adedeji Adenusi, MD, MPH1, Abdelaziz Mohamed, MBBS1, Cherif El Younis, MD2. P5990 - From Tolerance to Toxicity: Flares of Alcohol-Related Liver Injury Post-Sleeve Gastrectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY
Introduction: Bariatric surgery reduces first-pass hepatic metabolism and raises peak blood alcohol concentrations, therefore changing alcohol pharmacokinetics. Although this is generally known, there is less information on the clinical effects of modest alcohol intake following surgery without past liver disease. We present a case of intermittent alcohol use-induced flares of hepatitis following sleeve gastrectomy. This case emphasizes the potential for increased hepatotoxicity in this demographic.
Case Description/
Methods: A 52-year-old male with morbid obesity and hyperlipidemia underwent laparoscopic sleeve gastrectomy (LSG) in June 2022. He used to drink 42 drinks a week before surgery and showed little indication of liver injury and required no admission for alcoholic liver disease. One year after bariatric surgery, he was repeatedly hospitalized and had frequent emergency visits for abdominal pain and jaundice with minimal alcohol consumption of three beers a week.
Laboratory findings showed elevated liver enzymes during the 2024 hospitalizations, with bilirubin up to 41 mg/dL, AST 358 U/L, ALP 309 U/L, and INR 1.92 after a single episode of weekend alcohol use. Maddrey Discriminant Function (MDF) was 58.4, and his MELD-3 was 26. Ethanol concentration was negligible. His imaging revealed hepatic steatosis without cirrhosis or biliary obstruction. Autoimmune, metabolic, and infectious workups were negative. His liver injury episodes were more severe and more frequent with flares of alcoholic hepatitis, even though he consumed much less alcohol postoperatively.
Discussion: This case demonstrates increased sensitivity to alcohol-induced liver injury after sleeve gastrectomy, mainly due to a 50-70% reduction in gastric alcohol dehydrogenase enzyme (ADH) activity following LSG. This reduction lowers first-pass metabolism, resulting in higher blood alcohol levels and increased liver exposure to toxic metabolites. Consequently, even small amounts of alcohol can trigger severe hepatotoxicity.
Although bariatric surgery lowers steatosis and metabolic dysfunction-associated steatosis (MASH), therefore improving liver health, it paradoxically raises the risk of alcohol-related steatohepatitis. Up to 5% of patients develop alcohol-associated liver disease, and 33% develop problematic drinking post-surgery.
Clinicians should emphasize the selection process for bariatric surgery, identifying high-risk patients, counseling on complete alcohol abstinence, and close social support to reduce this phenomenon.
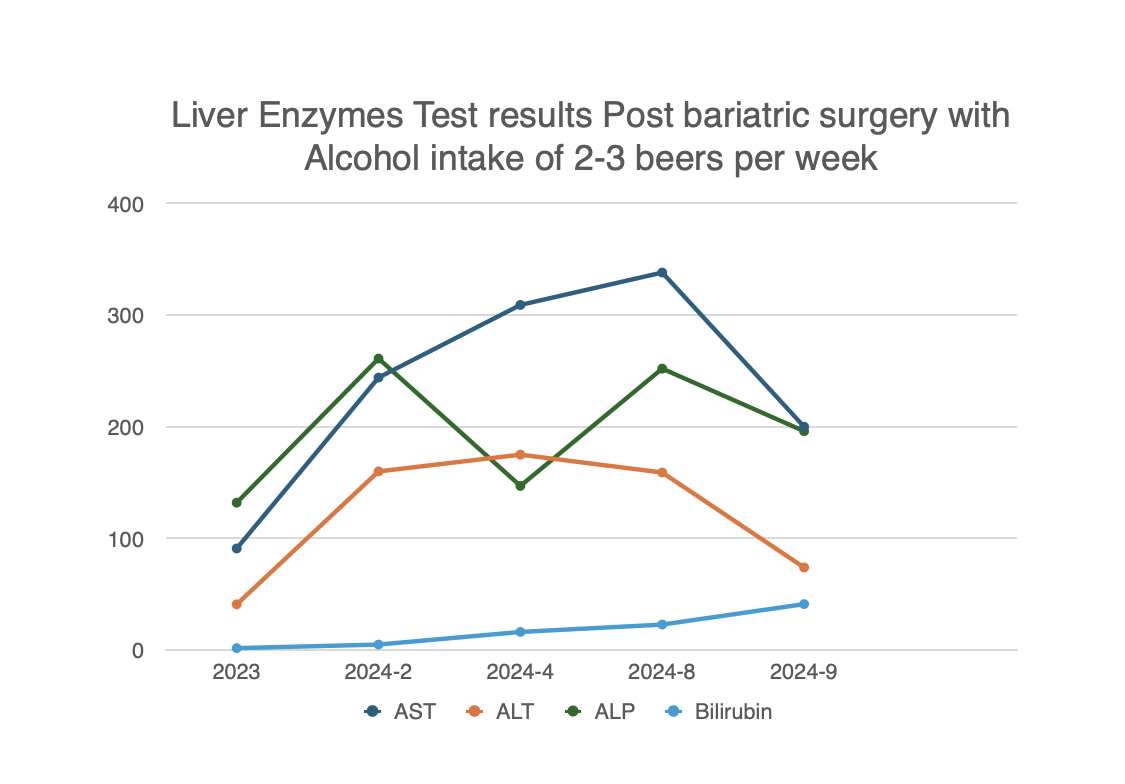
Figure: Liver Enzymes Results Prior to Bariatric Surgery with Alcohol intake of 42 beers per week
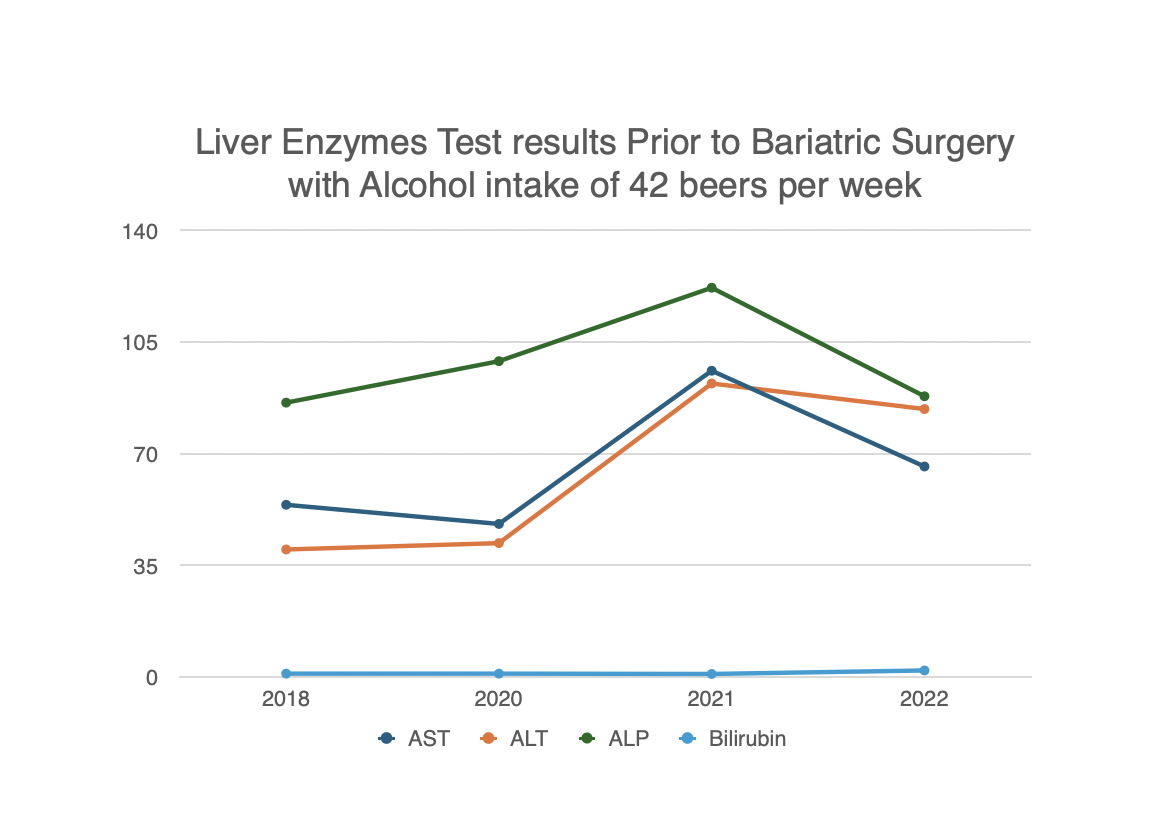
Figure: Liver Enzymes results Post Bariatric surgery with alcohol intake of 2-3 beers per week
Disclosures:
Mehak Mastoi indicated no relevant financial relationships.
Chidiebele Omaliko indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Abdelaziz Mohamed indicated no relevant financial relationships.
Cherif El Younis indicated no relevant financial relationships.
Mehak Mastoi, MD1, Chidiebele Omaliko, MD2, Adedeji Adenusi, MD, MPH1, Abdelaziz Mohamed, MBBS1, Cherif El Younis, MD2. P5990 - From Tolerance to Toxicity: Flares of Alcohol-Related Liver Injury Post-Sleeve Gastrectomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
