Tuesday Poster Session
Category: Liver
P5986 - A Cryptic Presentation of Post-transplant Lymphoproliferative Disorder in a Patient With Crohn's Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Divya Roy, DO (she/her/hers)
NYU Langone Health
Mineola, NY
Presenting Author(s)
Divya Roy, DO1, Peter Block, MD2, Saikiran Kilaru, MD2
1NYU Langone Health, Mineola, NY; 2NYU Langone Health, New York, NY
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a complication of solid organ transplant. Early-onset PTLD arises within the first year post transplant and is classically associated with Epstein-Barr virus (EBV) infection. In contrast, late onset PTLD occurs more than five years post-transplant with "very late" PTLD occurring beyond 10 years after transplantation. We describe a case of very late onset PTLD in a patient who initially presented with clinical and radiographic findings suggestive of a Crohn's disease (CD) flare, which upon further evaluation revealed EBV-negative diffuse large B cell lymphoma (DLBCL).
Case Description/
Methods: 44 year old male with a past medical history of ileal CD and primary sclerosing cholangitis status post liver transplant 11 years ago presented to the ED with acute abdominal pain, nausea and vomiting. He had been taking mycophenolate 500 mg twice daily for his liver allograft and mesalamine for CD, the latter he stopped taking a few months prior to presentation due to absent symptoms. He presented with an elevated C-reactive protein, fecal calprotectin and a CT abdomen pelvis showing circumferential mural thickening, possible small bowel intussusception, terminal ileum (TI) wall thickening and multiple enlarged lymph nodes necrotic in nature. Magnetic resonance enterography (MRE) confirmed TI inflammation. He was started on IV steroids for possible CD flare. He underwent colonoscopy which noted a few ileal aphthous ulcers with otherwise normal appearing colon (simplified endoscopic score for Crohn's disease of 7), and was transitioned to an oral steroid taper. Biopsy results showed mildly active chronic ileits without granuloma or dysplasia. Biopsy of the necrotic mesenteric lymph nodes revealed EBV negative DLBCL. He was treated with R-CHOP chemotherapy with consequent remission of PTLD.
Discussion: This case highlights the importance of maintaining high clinical suspicion for PTLD in liver transplant recipients with co-existing medical history of inflammatory bowel disease (IBD), as clinical management of de-novo PTLD versus IBD flare is fundamentally different. PTLD requires immunosuppressive reduction with potential chemotherapeutic augmentation while IBD flares are managed with immunosuppressive therapy. Patients with IBD have an increased risk of developing lymphoproliferative disorders (LPDs), even in the absence of immunosuppression. This patient had both immunosuppressive therapy and CD putting him at a high risk for developing PTLD.
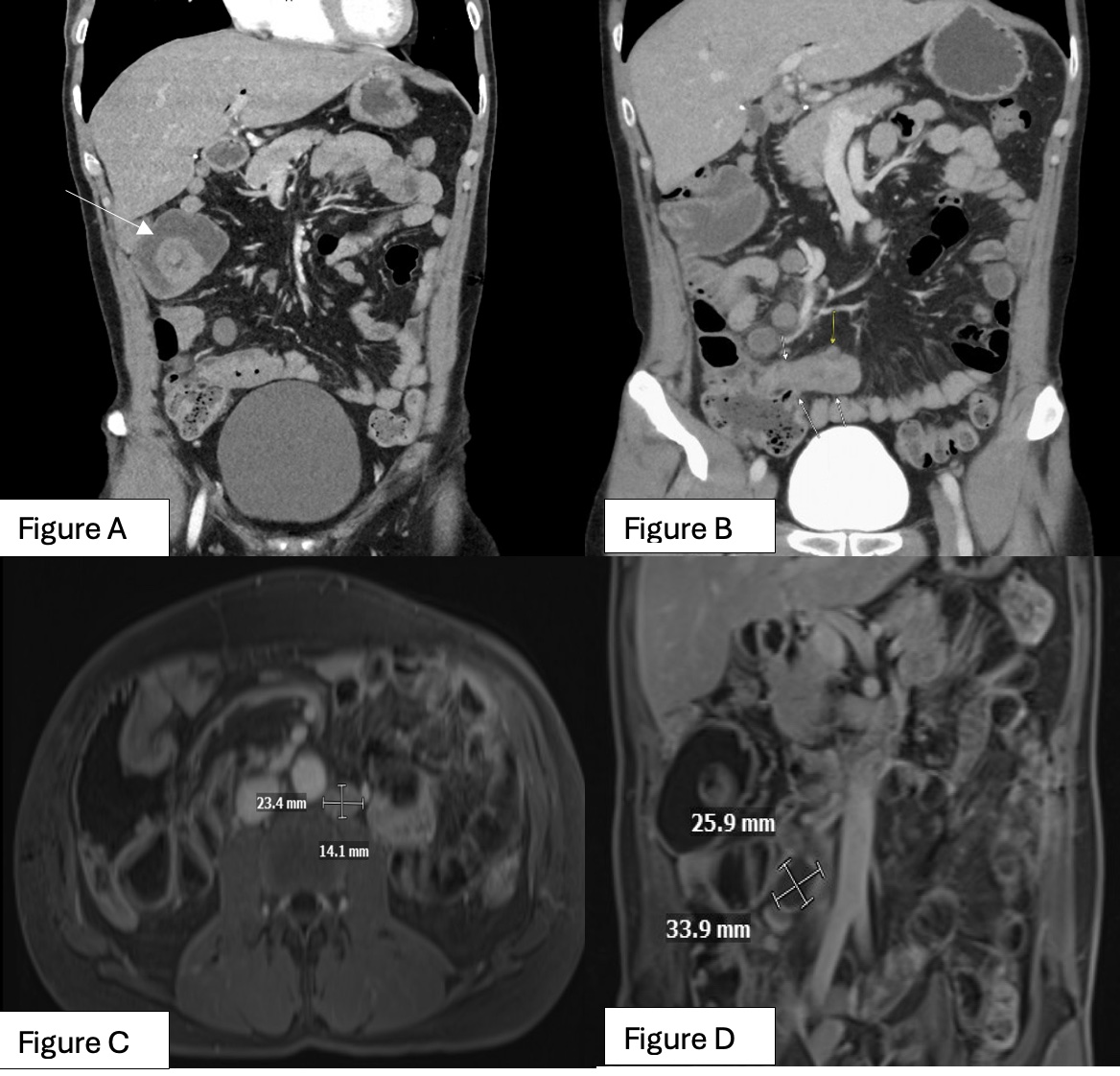
Figure: Figure A: CT abdomen/pelvis arrow showing a transient right upper quadrant small bowel intussusception
Figure B: CT abdomen/pelvis arrows showing distal/terminal ileum wall thickening suggestive of active inflammation
Figure C: MR enterography showing enlarging left lower para aortic lymph node
Figure D: MR enterography showing the largest of the lymph nodes with peripheral rim-enhancement and central necrosis
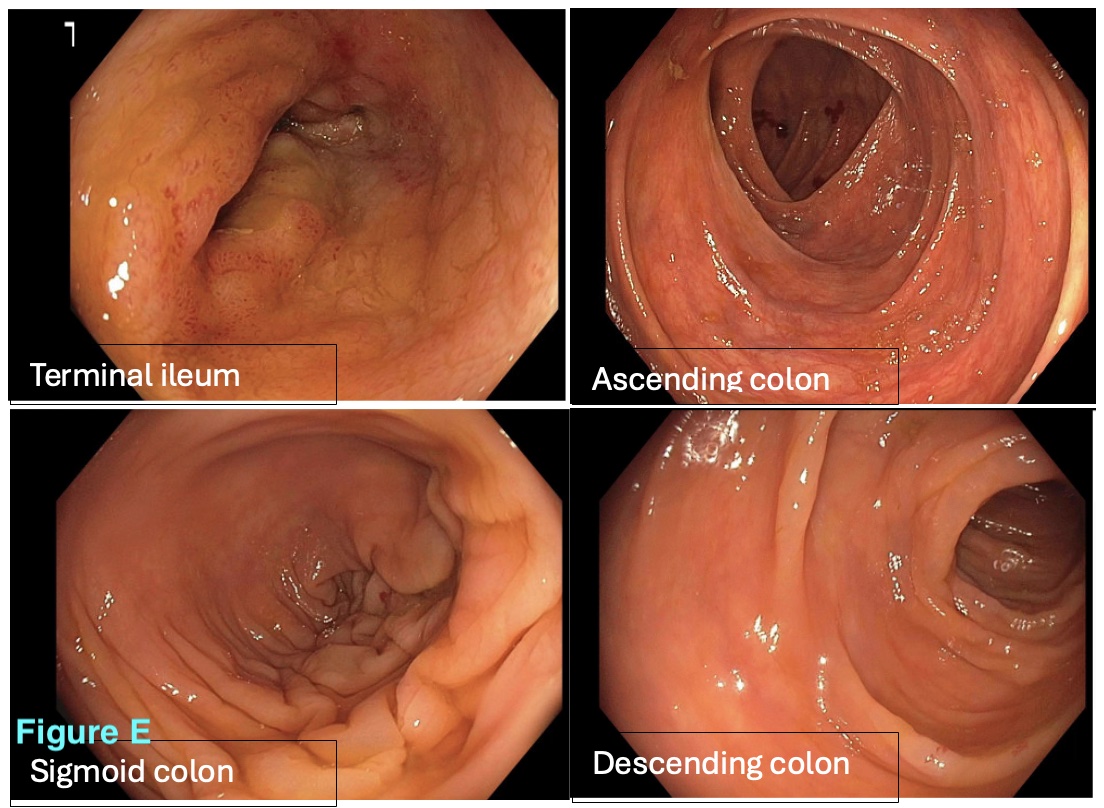
Figure: Figure E: Colonoscopy findings of the terminal ileum, ascending colon, sigmoid colon and descending colon with simple endoscopic score for Crohn's Disease: 7, mucosal inflammatory changes secondary Crohn's disease with ileitis. Aphthous ulcers noted in the ileum otherwise normal appearing colon.
Disclosures:
Divya Roy indicated no relevant financial relationships.
Peter Block indicated no relevant financial relationships.
Saikiran Kilaru indicated no relevant financial relationships.
Divya Roy, DO1, Peter Block, MD2, Saikiran Kilaru, MD2. P5986 - A Cryptic Presentation of Post-transplant Lymphoproliferative Disorder in a Patient With Crohn's Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYU Langone Health, Mineola, NY; 2NYU Langone Health, New York, NY
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a complication of solid organ transplant. Early-onset PTLD arises within the first year post transplant and is classically associated with Epstein-Barr virus (EBV) infection. In contrast, late onset PTLD occurs more than five years post-transplant with "very late" PTLD occurring beyond 10 years after transplantation. We describe a case of very late onset PTLD in a patient who initially presented with clinical and radiographic findings suggestive of a Crohn's disease (CD) flare, which upon further evaluation revealed EBV-negative diffuse large B cell lymphoma (DLBCL).
Case Description/
Methods: 44 year old male with a past medical history of ileal CD and primary sclerosing cholangitis status post liver transplant 11 years ago presented to the ED with acute abdominal pain, nausea and vomiting. He had been taking mycophenolate 500 mg twice daily for his liver allograft and mesalamine for CD, the latter he stopped taking a few months prior to presentation due to absent symptoms. He presented with an elevated C-reactive protein, fecal calprotectin and a CT abdomen pelvis showing circumferential mural thickening, possible small bowel intussusception, terminal ileum (TI) wall thickening and multiple enlarged lymph nodes necrotic in nature. Magnetic resonance enterography (MRE) confirmed TI inflammation. He was started on IV steroids for possible CD flare. He underwent colonoscopy which noted a few ileal aphthous ulcers with otherwise normal appearing colon (simplified endoscopic score for Crohn's disease of 7), and was transitioned to an oral steroid taper. Biopsy results showed mildly active chronic ileits without granuloma or dysplasia. Biopsy of the necrotic mesenteric lymph nodes revealed EBV negative DLBCL. He was treated with R-CHOP chemotherapy with consequent remission of PTLD.
Discussion: This case highlights the importance of maintaining high clinical suspicion for PTLD in liver transplant recipients with co-existing medical history of inflammatory bowel disease (IBD), as clinical management of de-novo PTLD versus IBD flare is fundamentally different. PTLD requires immunosuppressive reduction with potential chemotherapeutic augmentation while IBD flares are managed with immunosuppressive therapy. Patients with IBD have an increased risk of developing lymphoproliferative disorders (LPDs), even in the absence of immunosuppression. This patient had both immunosuppressive therapy and CD putting him at a high risk for developing PTLD.
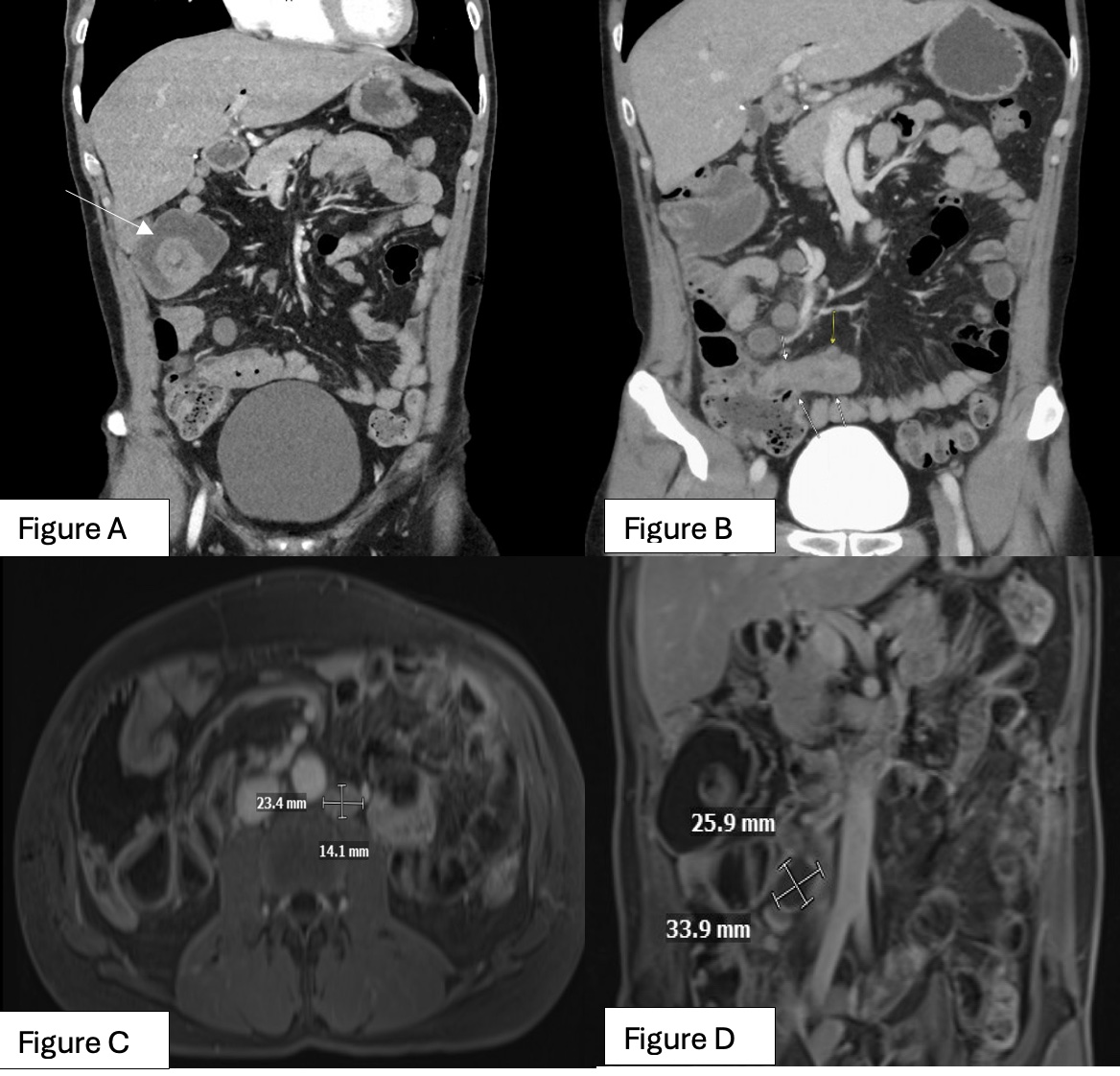
Figure: Figure A: CT abdomen/pelvis arrow showing a transient right upper quadrant small bowel intussusception
Figure B: CT abdomen/pelvis arrows showing distal/terminal ileum wall thickening suggestive of active inflammation
Figure C: MR enterography showing enlarging left lower para aortic lymph node
Figure D: MR enterography showing the largest of the lymph nodes with peripheral rim-enhancement and central necrosis
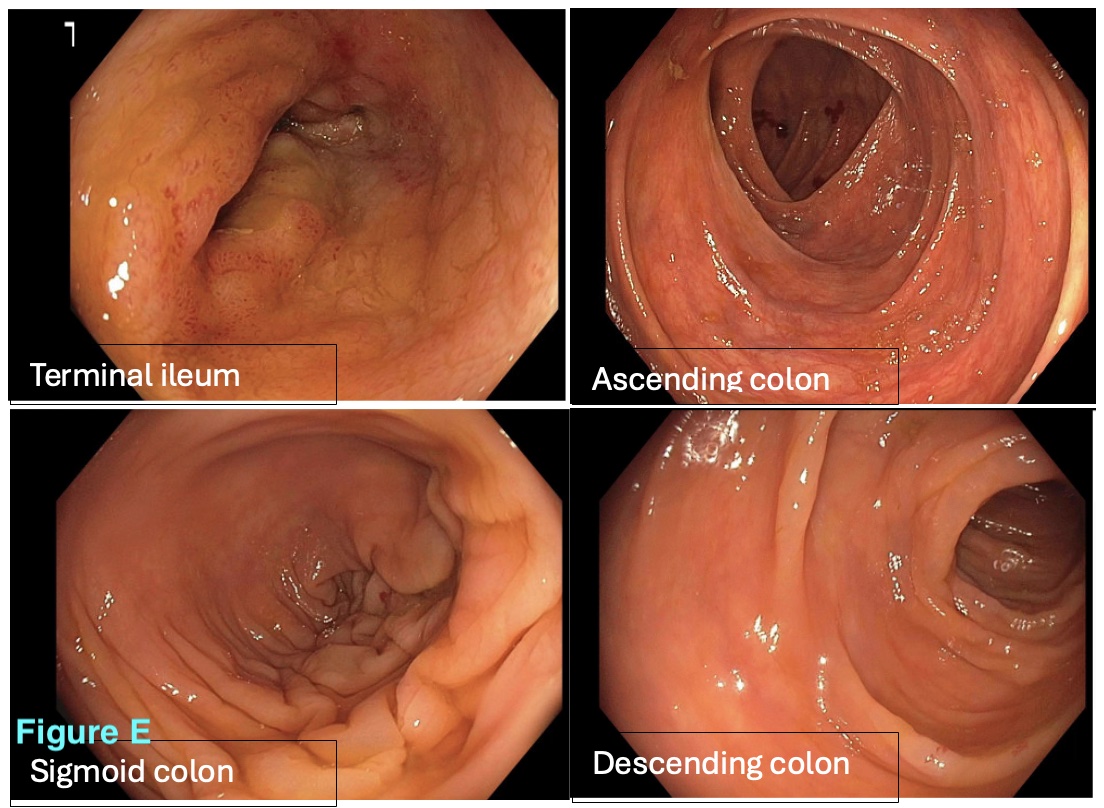
Figure: Figure E: Colonoscopy findings of the terminal ileum, ascending colon, sigmoid colon and descending colon with simple endoscopic score for Crohn's Disease: 7, mucosal inflammatory changes secondary Crohn's disease with ileitis. Aphthous ulcers noted in the ileum otherwise normal appearing colon.
Disclosures:
Divya Roy indicated no relevant financial relationships.
Peter Block indicated no relevant financial relationships.
Saikiran Kilaru indicated no relevant financial relationships.
Divya Roy, DO1, Peter Block, MD2, Saikiran Kilaru, MD2. P5986 - A Cryptic Presentation of Post-transplant Lymphoproliferative Disorder in a Patient With Crohn's Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
