Tuesday Poster Session
Category: Liver
P5979 - Pus Without Pathogen: A Surprising Case of Multiple Sterile Pyogenic Liver Abscesses
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Kazi Haque, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Mariam Rizvi, MD1, Jacob Reitnauer, 1, George Ishac, MD1, Iyad Al-Bustami, MD, MPH2, Kazi Haque, MD3
1University of Texas at Houston, Houston, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3McGovern Medical School at UTHealth, Pearland, TX
Introduction: Pyogenic liver abscesses (PLA) are localized collections of pus within the liver, typically arising from biliary disease, malignancies, or diabetes. A subset known as cryptogenic liver abscesses (CLAs) occurs without an identifiable source. We discuss a case of a liver abscess with no known etiology, examining its clinical course, treatment approach, and potential underlying factors.
Case Description/
Methods: A 59-year-old male with a history of treated hepatitis C presented with 1-2 weeks of fever, night sweats, decreased appetite, vomiting and generalized abdominal pain. He was noted to be afebrile with stable vital signs. Labs were notable for leukocytosis and an elevated alkaline phosphatase. CT abdomen and pelvis showed three hypodense masses throughout the liver concerning for multifocal abscesses further confirmed by MRI. Tumor markers were negative. HIV, respiratory, blood and urine cultures were negative. Hepatitis panel revealed a reactive hepatitis C antibody with a negative hepatitis C PCR. He was started on vancomycin, cefepime and piperacillin/tazobactam. Interventional radiology (IR) initially placed two drains leading to partial abscess improvement, however a residual collection remained unchanged, prompting placement of a third drain. Antibiotics were de-escalated. Infectious workup performed on all drain specimens returned negative for bacteria, fungi and tuberculosis. Despite negative culture data, he was transitioned to oral ciprofloxacin and metronidazole due to the size and number of his abscesses. He was then discharged. All three drains were removed a month later outpatient and repeat CT imaging revealed resolution of abscesses.
Discussion: While many cases of PLA have identifiable causes, a significant proportion remain cryptogenic with no apparent source of infection. This raises important questions about the pathogenesis and management of CLAs. The case described above underscores the complexities of PLA management, particularly in patients requiring multiple IR interventions for persistent collections. Given these uncertainties, there is a clear need for further research to better understand the pathophysiology of CLAs and refine treatment strategies. Identifying potential risk factors and improving diagnostic precision could ultimately enhance patient outcomes and target therapeutic approaches. As illustrated by our patient’s case, persistent abscess collections necessitate a dynamic approach, integrating IR-guided interventions with antimicrobial therapy.
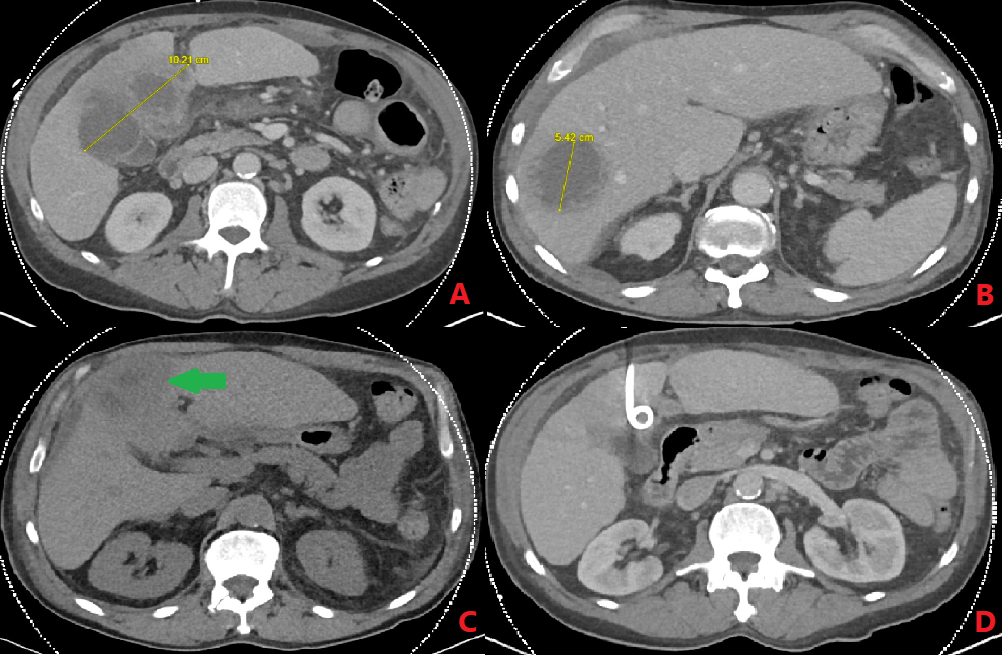
Figure: Figure 1 A-D: A-B) Initial CT Abdomen and Pelvis (CTAP) on 12/14/25 indicating two distinct masses with sizes of 10.3 cm and 5.2 cm. Third Mass is not shown. C) Repeat CTAP on 12/22/24 showing an un-resolving liver abscess necessitating IR-guided drain placement. Other two masses had decreased in size. D) Repeat CTAP on 1/9/25 showing resolution of all masses with pigtail catheter in-view.
Disclosures:
Mariam Rizvi indicated no relevant financial relationships.
Jacob Reitnauer indicated no relevant financial relationships.
George Ishac indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Mariam Rizvi, MD1, Jacob Reitnauer, 1, George Ishac, MD1, Iyad Al-Bustami, MD, MPH2, Kazi Haque, MD3. P5979 - Pus Without Pathogen: A Surprising Case of Multiple Sterile Pyogenic Liver Abscesses, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Houston, Houston, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3McGovern Medical School at UTHealth, Pearland, TX
Introduction: Pyogenic liver abscesses (PLA) are localized collections of pus within the liver, typically arising from biliary disease, malignancies, or diabetes. A subset known as cryptogenic liver abscesses (CLAs) occurs without an identifiable source. We discuss a case of a liver abscess with no known etiology, examining its clinical course, treatment approach, and potential underlying factors.
Case Description/
Methods: A 59-year-old male with a history of treated hepatitis C presented with 1-2 weeks of fever, night sweats, decreased appetite, vomiting and generalized abdominal pain. He was noted to be afebrile with stable vital signs. Labs were notable for leukocytosis and an elevated alkaline phosphatase. CT abdomen and pelvis showed three hypodense masses throughout the liver concerning for multifocal abscesses further confirmed by MRI. Tumor markers were negative. HIV, respiratory, blood and urine cultures were negative. Hepatitis panel revealed a reactive hepatitis C antibody with a negative hepatitis C PCR. He was started on vancomycin, cefepime and piperacillin/tazobactam. Interventional radiology (IR) initially placed two drains leading to partial abscess improvement, however a residual collection remained unchanged, prompting placement of a third drain. Antibiotics were de-escalated. Infectious workup performed on all drain specimens returned negative for bacteria, fungi and tuberculosis. Despite negative culture data, he was transitioned to oral ciprofloxacin and metronidazole due to the size and number of his abscesses. He was then discharged. All three drains were removed a month later outpatient and repeat CT imaging revealed resolution of abscesses.
Discussion: While many cases of PLA have identifiable causes, a significant proportion remain cryptogenic with no apparent source of infection. This raises important questions about the pathogenesis and management of CLAs. The case described above underscores the complexities of PLA management, particularly in patients requiring multiple IR interventions for persistent collections. Given these uncertainties, there is a clear need for further research to better understand the pathophysiology of CLAs and refine treatment strategies. Identifying potential risk factors and improving diagnostic precision could ultimately enhance patient outcomes and target therapeutic approaches. As illustrated by our patient’s case, persistent abscess collections necessitate a dynamic approach, integrating IR-guided interventions with antimicrobial therapy.
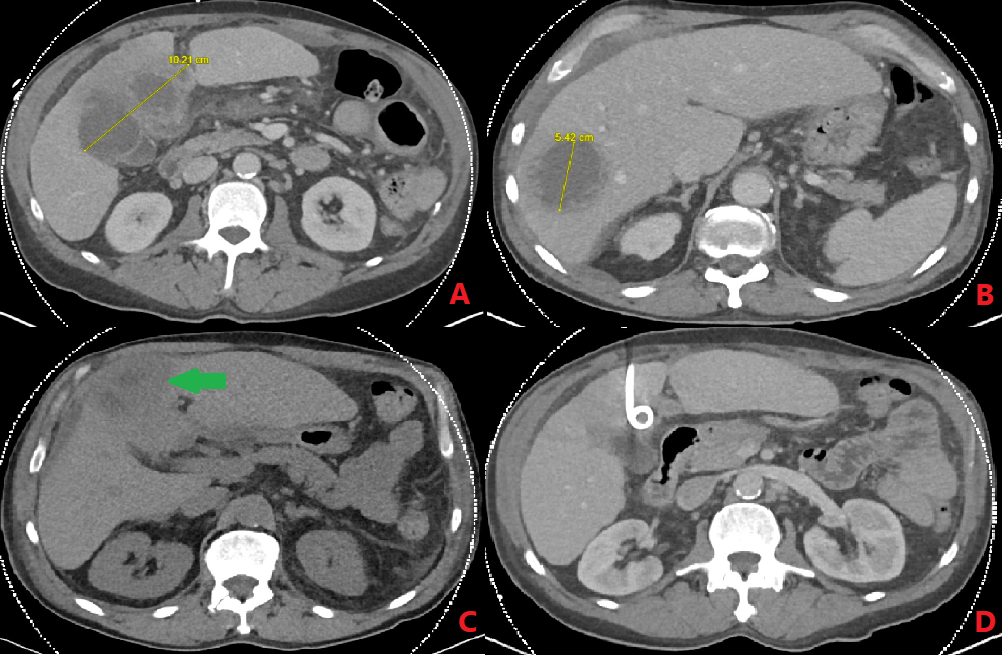
Figure: Figure 1 A-D: A-B) Initial CT Abdomen and Pelvis (CTAP) on 12/14/25 indicating two distinct masses with sizes of 10.3 cm and 5.2 cm. Third Mass is not shown. C) Repeat CTAP on 12/22/24 showing an un-resolving liver abscess necessitating IR-guided drain placement. Other two masses had decreased in size. D) Repeat CTAP on 1/9/25 showing resolution of all masses with pigtail catheter in-view.
Disclosures:
Mariam Rizvi indicated no relevant financial relationships.
Jacob Reitnauer indicated no relevant financial relationships.
George Ishac indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Mariam Rizvi, MD1, Jacob Reitnauer, 1, George Ishac, MD1, Iyad Al-Bustami, MD, MPH2, Kazi Haque, MD3. P5979 - Pus Without Pathogen: A Surprising Case of Multiple Sterile Pyogenic Liver Abscesses, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
