Tuesday Poster Session
Category: Liver
P5978 - The Milky Mystery: Non-Chylous Ascites in Systemic Lupus Erythematosus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Kazi Haque, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Jacob Reitnauer, 1, Kazi Haque, MD2, Nina Quirk, MD, MS3, Iyad Al-Bustami, MD, MPH2, Ruth Bell, MD4, Akshata Moghe, MD2
1University of Texas at Houston, Houston, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3University of Texas Health Sciences Center in Houston, Houston, TX; 4McGovern Medical School at UTHealth, Houston, TX
Introduction: Ascites is a physical sign that is commonly associated with cirrhosis but can manifest due to other etiologies. We present a patient without cirrhosis who presented with milky, but non-chylous ascites, as a likely manifestation of worsening systemic lupus erythematosus (SLE).
Case Description/
Methods: A 27-year-old woman with recently diagnosed Class IV lupus nephritis was admitted for worsening lupus flare. Her hospital course included a cardiac workup that revealed dilated cardiomyopathy secondary to SLE with a reduced ejection fraction (41%) and a component of myocarditis. Her volume overload was initially managed by diuresis but soon she developed worsening ascites unresponsive to diuretics and a low-salt diet. She required multiple paracenteses. Ascitic fluid studies were notable for a milky appearance (Figure 1) but negative for infection and hypertriglyceridemia. Serum Albumin Ascites Gradient (SAAG) was 1.6 g/dL with ascitic protein < 2.5 g/dL. However, she had no evidence of cirrhosis on clinical exam, laboratory testing or imaging. Ultrasound elastography also showed a liver stiffness of only 5.9 kPa, ruling out advanced fibrosis. Additional testing with QuantiFERON gold, amylase, and serum triglycerides was normal/negative. Ascitic fluid cytology was negative for malignancy. Her nephritis was managed with diuretics and anti-hypertensive medications by nephrology, and she was discharged with close rheumatology follow up. Three months later, ascites has resolved with improvement in the nephritis.
Discussion: This patient’s ascitic fluid appears to be liver-related due to the high SAAG score and low ascitic protein. Algorithms point toward hepatologic or portal vascular pathologies, however, she has no evidence of liver disease. Ascitic triglycerides were not above the threshold of 200 mg/dl to be considered chylous ascites. Milky, non-chylous ascites has been described in literature as a manifestation of lupus nephritis. In SLE, serositis and peritoneal inflammation leads to immune activation and increased vascular permeability. Other etiologies include pseudochylous ascites which present as ascites with a milky appearance but with low triglycerides, high cholesterol, and no chylomicrons; and lupus protein-losing enteropathy which would be characterized by low albumin ascites. Microscopy can aid in solidifying the diagnosis. Management focuses on treatment of the underlying nephritis and cardiomyopathy as well as symptomatic management with paracentesis.
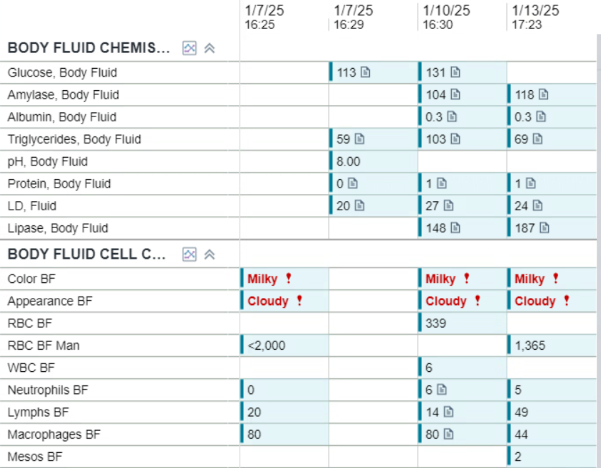
Figure: Figure 1 A-C: a-b) Axial slice (a) and Coronal Slice (b) of CT Abdomen and Pelvis showing significant ascites. Green arrows pointing to Ascites
c) Sample of Milky Ascites obtained from paracentesis.
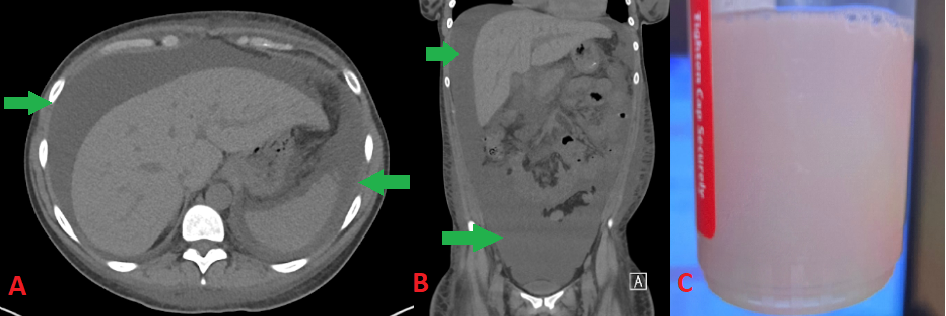
Figure: Table 1: Labs related to the three paracentesis that occurred while patient remained in hospital.
Disclosures:
Jacob Reitnauer indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Nina Quirk indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Ruth Bell indicated no relevant financial relationships.
Akshata Moghe indicated no relevant financial relationships.
Jacob Reitnauer, 1, Kazi Haque, MD2, Nina Quirk, MD, MS3, Iyad Al-Bustami, MD, MPH2, Ruth Bell, MD4, Akshata Moghe, MD2. P5978 - The Milky Mystery: Non-Chylous Ascites in Systemic Lupus Erythematosus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas at Houston, Houston, TX; 2University of Texas Health, McGovern Medical School, Houston, TX; 3University of Texas Health Sciences Center in Houston, Houston, TX; 4McGovern Medical School at UTHealth, Houston, TX
Introduction: Ascites is a physical sign that is commonly associated with cirrhosis but can manifest due to other etiologies. We present a patient without cirrhosis who presented with milky, but non-chylous ascites, as a likely manifestation of worsening systemic lupus erythematosus (SLE).
Case Description/
Methods: A 27-year-old woman with recently diagnosed Class IV lupus nephritis was admitted for worsening lupus flare. Her hospital course included a cardiac workup that revealed dilated cardiomyopathy secondary to SLE with a reduced ejection fraction (41%) and a component of myocarditis. Her volume overload was initially managed by diuresis but soon she developed worsening ascites unresponsive to diuretics and a low-salt diet. She required multiple paracenteses. Ascitic fluid studies were notable for a milky appearance (Figure 1) but negative for infection and hypertriglyceridemia. Serum Albumin Ascites Gradient (SAAG) was 1.6 g/dL with ascitic protein < 2.5 g/dL. However, she had no evidence of cirrhosis on clinical exam, laboratory testing or imaging. Ultrasound elastography also showed a liver stiffness of only 5.9 kPa, ruling out advanced fibrosis. Additional testing with QuantiFERON gold, amylase, and serum triglycerides was normal/negative. Ascitic fluid cytology was negative for malignancy. Her nephritis was managed with diuretics and anti-hypertensive medications by nephrology, and she was discharged with close rheumatology follow up. Three months later, ascites has resolved with improvement in the nephritis.
Discussion: This patient’s ascitic fluid appears to be liver-related due to the high SAAG score and low ascitic protein. Algorithms point toward hepatologic or portal vascular pathologies, however, she has no evidence of liver disease. Ascitic triglycerides were not above the threshold of 200 mg/dl to be considered chylous ascites. Milky, non-chylous ascites has been described in literature as a manifestation of lupus nephritis. In SLE, serositis and peritoneal inflammation leads to immune activation and increased vascular permeability. Other etiologies include pseudochylous ascites which present as ascites with a milky appearance but with low triglycerides, high cholesterol, and no chylomicrons; and lupus protein-losing enteropathy which would be characterized by low albumin ascites. Microscopy can aid in solidifying the diagnosis. Management focuses on treatment of the underlying nephritis and cardiomyopathy as well as symptomatic management with paracentesis.
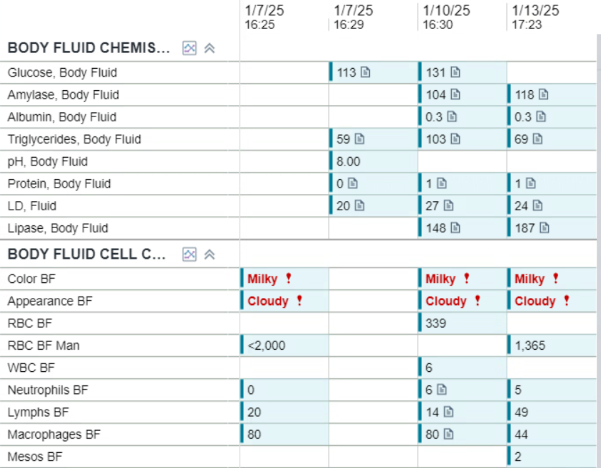
Figure: Figure 1 A-C: a-b) Axial slice (a) and Coronal Slice (b) of CT Abdomen and Pelvis showing significant ascites. Green arrows pointing to Ascites
c) Sample of Milky Ascites obtained from paracentesis.
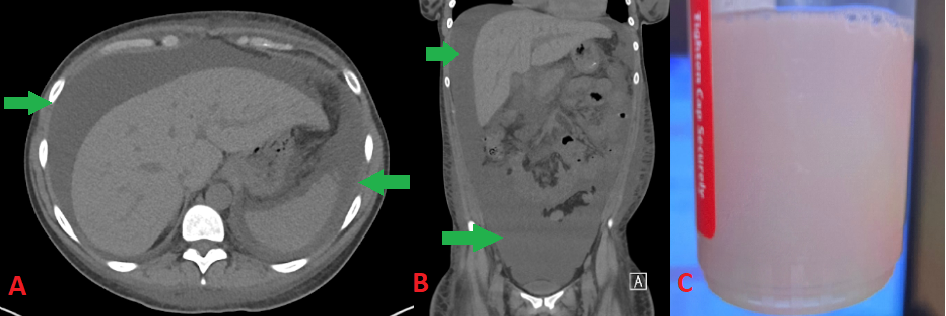
Figure: Table 1: Labs related to the three paracentesis that occurred while patient remained in hospital.
Disclosures:
Jacob Reitnauer indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Nina Quirk indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Ruth Bell indicated no relevant financial relationships.
Akshata Moghe indicated no relevant financial relationships.
Jacob Reitnauer, 1, Kazi Haque, MD2, Nina Quirk, MD, MS3, Iyad Al-Bustami, MD, MPH2, Ruth Bell, MD4, Akshata Moghe, MD2. P5978 - The Milky Mystery: Non-Chylous Ascites in Systemic Lupus Erythematosus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
