Tuesday Poster Session
Category: Liver
P6059 - Incidental Discovery of Amyloidosis in Donor Livers: A Case Series and Implications for Liver Transplant Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Isaac Giovannie, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Giovannie Isaac-Coss, MD1, Aryanna Sousa, MD, MPH2, Edie Chan, MD1, Nancy Reau, MD, FACG1, Justin Mitchell, MD1, Sujit Janardhan, MD, PhD1, Sheila Eswaran, MD1
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center, Providence, RI
Introduction: Amyloidosis is a rare condition, with an estimated prevalence of 7 cases per million persons per year, characterized by extracellular deposition of misfolded protein fibrils that can affect multiple organs, including the liver. While hepatic involvement can lead to hepatomegaly, cholestasis, and liver dysfunction, incidental amyloid deposition in donor livers used for orthotopic liver transplantation (OLT) is exceedingly rare, and its clinical significance remains uncertain. We present two cases of donor liver amyloidosis identified during OLT, including one confirmed as AA-type amyloid by mass spectrometry, and discuss implications for graft outcomes.
Case Description/
Methods: Case 1:
A 64-year-old woman with MASH and hep B cirrhosis complicated by hepatic encephalopathy, ascites, and hepatic hydrothorax underwent OLT. Postop course was complicated by hepatic artery thrombosis, requiring retransplantation one week later. Biopsy of the second donor liver revealed globular, periportal, and perivascular amyloid deposition, confirmed by Congo red staining. Mild portal fibrosis was present without significant inflammation or steatosis. Follow-up biopsy one month later showed persistent amyloid deposition without acute rejection.
Case 2:
A 51-year-old man with AALD cirrhosis complicated by ascites and HE underwent OLT. Donor liver biopsy demonstrated sinusoidal amyloid deposition with hepatocyte atrophy. Congo red stain confirmed amyloid, and liquid chromatography tandem mass spectrometry identified AA (serum amyloid A)-type amyloid. Follow-up biopsy three months post-transplant showed persistent sinusoidal amyloid without evidence of acute cellular rejection or significant fibrosis.
Discussion: These cases highlight the rare incidental finding of amyloidosis in donor livers. Amyloid types include AL (light chain), AA (serum amyloid A), and ATTR (transthyretin), among others, with diagnosis confirmed by Congo red staining and mass spectrometry for subtype identification. Notably, in Case 2, AA-type amyloid suggests unrecognized systemic inflammation in the donor. Neither recipient exhibited early graft dysfunction despite persistent amyloid on follow-up. While natural history studies suggest hepatic amyloidosis can progress to portal hypertension and liver dysfunction over time, such progression was not observed here. Currently, no specific guidelines exist for managing donor grafts with incidental amyloidosis; recognizing this rare finding may warrant closer post-transplant surveillance.
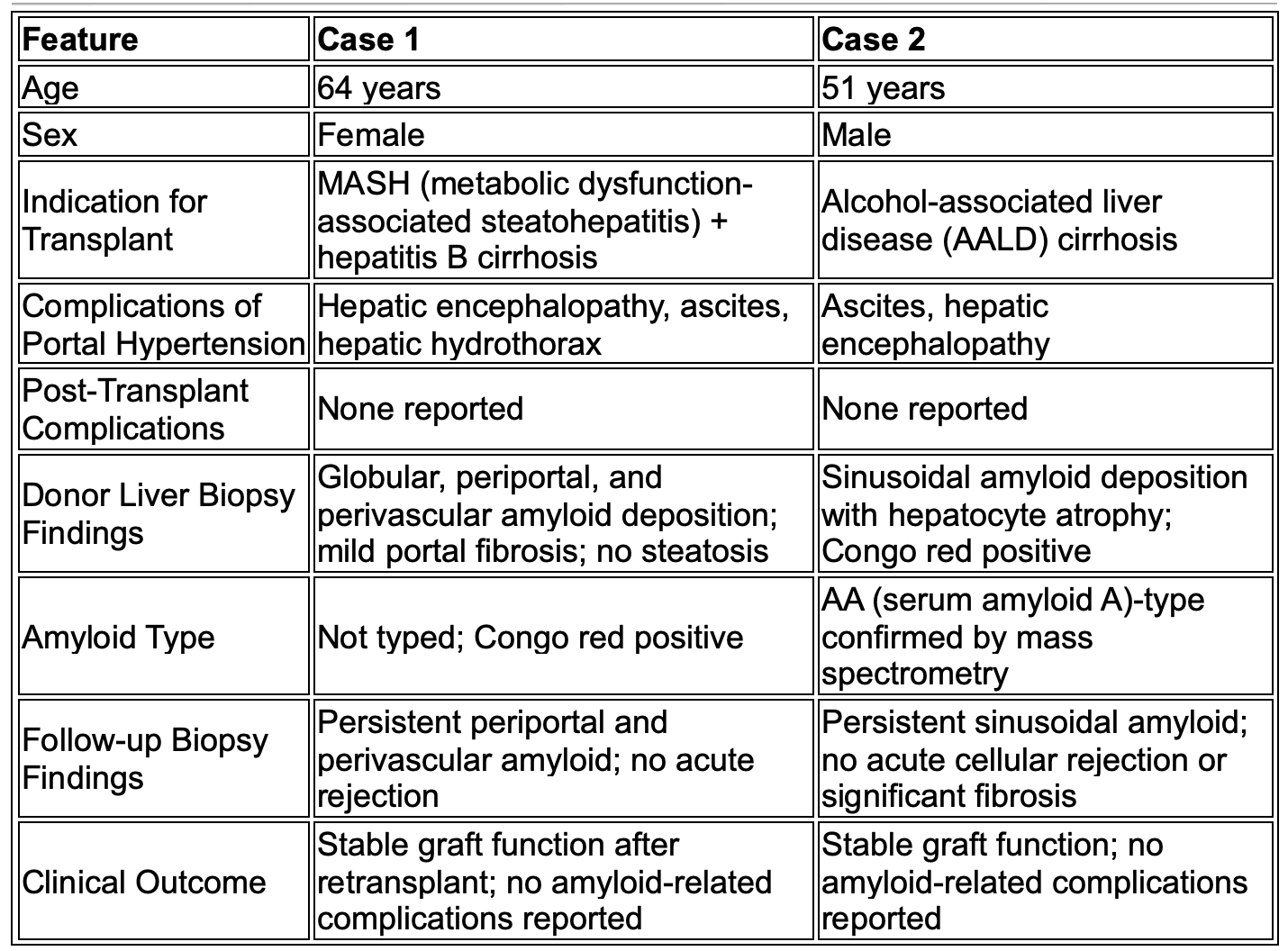
Figure: Table 1: Clinical and Histopathologic Comparison of Two Cases of Donor Liver Amyloidosis Identified During Orthotopic Liver Transplantation
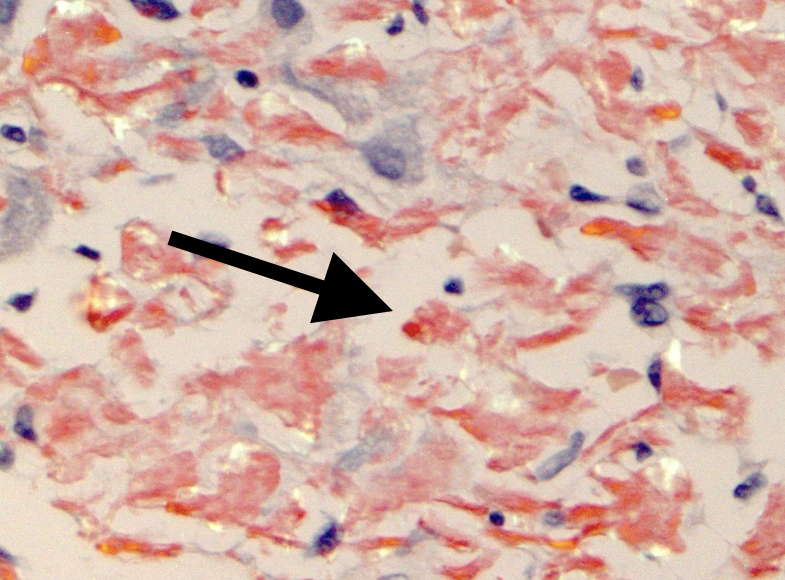
Figure: Image 1: Case 1, biopsy of the donor liver showing globular, periportal, and perivascular amyloid deposition, confirmed by Congo red staining (black arrow) (40X). Mild portal fibrosis was present without significant inflammation or steatosis.
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Edie Chan indicated no relevant financial relationships.
Nancy Reau: AbbVie – Grant/Research Support. Arbutus – Advisor or Review Panel Member. Gilead – Advisory Committee/Board Member, Grant/Research Support. Salix – Advisory Committee/Board Member, Grant/Research Support. VIR – Advisory Committee/Board Member, Grant/Research Support.
Justin Mitchell indicated no relevant financial relationships.
Sujit Janardhan indicated no relevant financial relationships.
Sheila Eswaran indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Aryanna Sousa, MD, MPH2, Edie Chan, MD1, Nancy Reau, MD, FACG1, Justin Mitchell, MD1, Sujit Janardhan, MD, PhD1, Sheila Eswaran, MD1. P6059 - Incidental Discovery of Amyloidosis in Donor Livers: A Case Series and Implications for Liver Transplant Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Giovannie Isaac-Coss, MD1, Aryanna Sousa, MD, MPH2, Edie Chan, MD1, Nancy Reau, MD, FACG1, Justin Mitchell, MD1, Sujit Janardhan, MD, PhD1, Sheila Eswaran, MD1
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center, Providence, RI
Introduction: Amyloidosis is a rare condition, with an estimated prevalence of 7 cases per million persons per year, characterized by extracellular deposition of misfolded protein fibrils that can affect multiple organs, including the liver. While hepatic involvement can lead to hepatomegaly, cholestasis, and liver dysfunction, incidental amyloid deposition in donor livers used for orthotopic liver transplantation (OLT) is exceedingly rare, and its clinical significance remains uncertain. We present two cases of donor liver amyloidosis identified during OLT, including one confirmed as AA-type amyloid by mass spectrometry, and discuss implications for graft outcomes.
Case Description/
Methods: Case 1:
A 64-year-old woman with MASH and hep B cirrhosis complicated by hepatic encephalopathy, ascites, and hepatic hydrothorax underwent OLT. Postop course was complicated by hepatic artery thrombosis, requiring retransplantation one week later. Biopsy of the second donor liver revealed globular, periportal, and perivascular amyloid deposition, confirmed by Congo red staining. Mild portal fibrosis was present without significant inflammation or steatosis. Follow-up biopsy one month later showed persistent amyloid deposition without acute rejection.
Case 2:
A 51-year-old man with AALD cirrhosis complicated by ascites and HE underwent OLT. Donor liver biopsy demonstrated sinusoidal amyloid deposition with hepatocyte atrophy. Congo red stain confirmed amyloid, and liquid chromatography tandem mass spectrometry identified AA (serum amyloid A)-type amyloid. Follow-up biopsy three months post-transplant showed persistent sinusoidal amyloid without evidence of acute cellular rejection or significant fibrosis.
Discussion: These cases highlight the rare incidental finding of amyloidosis in donor livers. Amyloid types include AL (light chain), AA (serum amyloid A), and ATTR (transthyretin), among others, with diagnosis confirmed by Congo red staining and mass spectrometry for subtype identification. Notably, in Case 2, AA-type amyloid suggests unrecognized systemic inflammation in the donor. Neither recipient exhibited early graft dysfunction despite persistent amyloid on follow-up. While natural history studies suggest hepatic amyloidosis can progress to portal hypertension and liver dysfunction over time, such progression was not observed here. Currently, no specific guidelines exist for managing donor grafts with incidental amyloidosis; recognizing this rare finding may warrant closer post-transplant surveillance.
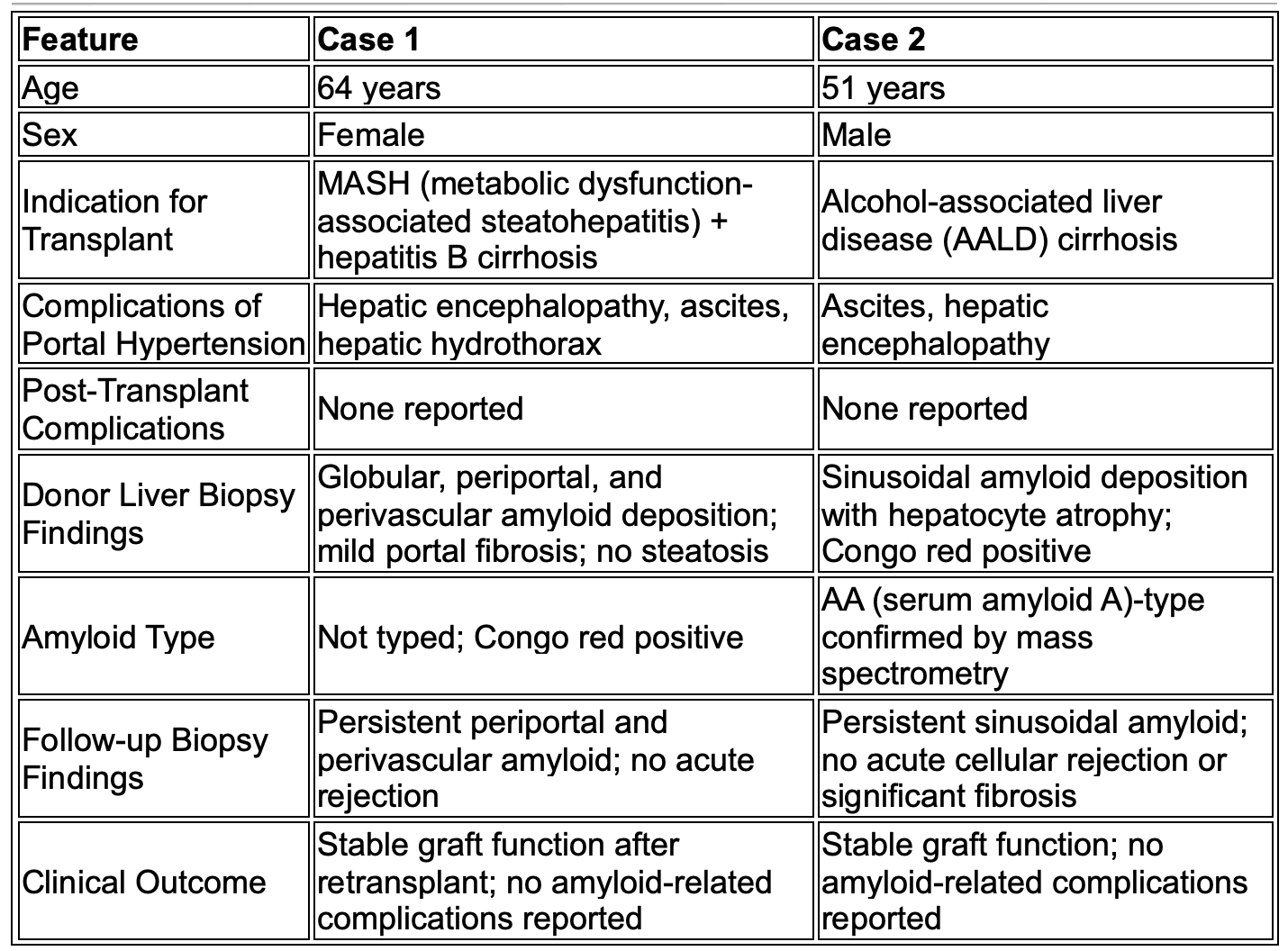
Figure: Table 1: Clinical and Histopathologic Comparison of Two Cases of Donor Liver Amyloidosis Identified During Orthotopic Liver Transplantation
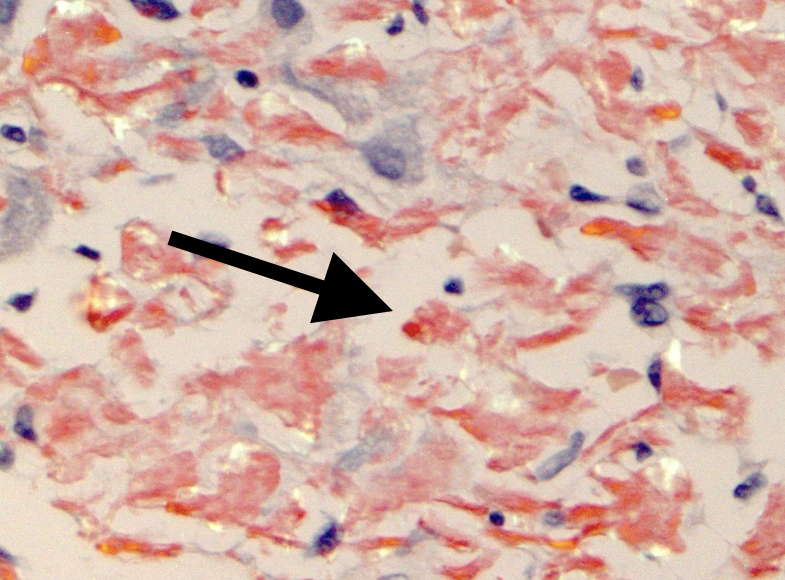
Figure: Image 1: Case 1, biopsy of the donor liver showing globular, periportal, and perivascular amyloid deposition, confirmed by Congo red staining (black arrow) (40X). Mild portal fibrosis was present without significant inflammation or steatosis.
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Edie Chan indicated no relevant financial relationships.
Nancy Reau: AbbVie – Grant/Research Support. Arbutus – Advisor or Review Panel Member. Gilead – Advisory Committee/Board Member, Grant/Research Support. Salix – Advisory Committee/Board Member, Grant/Research Support. VIR – Advisory Committee/Board Member, Grant/Research Support.
Justin Mitchell indicated no relevant financial relationships.
Sujit Janardhan indicated no relevant financial relationships.
Sheila Eswaran indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Aryanna Sousa, MD, MPH2, Edie Chan, MD1, Nancy Reau, MD, FACG1, Justin Mitchell, MD1, Sujit Janardhan, MD, PhD1, Sheila Eswaran, MD1. P6059 - Incidental Discovery of Amyloidosis in Donor Livers: A Case Series and Implications for Liver Transplant Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

