Tuesday Poster Session
Category: Liver
P6055 - A Rare Case of Severe Hepatic Crisis in a Patient With Sickle Cell Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Veronica West, DO
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Veronica West, DO1, John Sheehy, BS2, Carolyn Hogan, MD1, Miguel Agudelo, MD1
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Acute hepatic vaso-occlusive episodes are seen in approximately 10% of adults with sickle cell disease (SCD). The typical presentation includes RUQ pain, tender hepatomegaly, and aminotransferase levels that rarely surpass 300 units/L. We present a case of a 29-year-old male with sickle cell hemoglobin SC disease who presented with a sickle cell pain crisis found to have towering transaminases secondary to ischemic injury from sickle cell hepatopathy (SCH).
Case Description/
Methods: History was notable for days of extremity, back pain, nausea after a binge alcohol ingestion. The patient was hemodynamically stable and had no encephalopathy. Labs were notable for an alanine aminotransferase of 374 U/L peaking at 2,201 U/L, an aspartate aminotransferase of 849 U/L peaking at 4,267 U/L, prolonged INR of 3.0, and a direct hyperbilirubinemia peaking at 5.1 mg/dl. Viral hepatitides were negative. Contrasted CT showed acute pancreatitis and cholelithiasis, but was negative for choledocholithiasis, cholecystitis, portal vein thrombosis, or outflow obstruction. His only risk factor for liver disease was alcohol use. To decrease the amount of sickling, red cell exchange was used to lower the hemoglobin S-C level. His liver function and enzymes subsequently improved.
Discussion: The rapid improvement in his aminotransferase levels was consistent with ischemic hepatopathy. The likely etiology was SCH, resulting from microvascular vaso-occlusion due to red blood cell sickling within the hepatic vasculature. In SCH, aminotransferase levels typically peak around 300 U/L; values exceeding 1,000 U/L, as seen in this case, are rare. Although hepatic crisis in SCD of this severity are uncommon, they are clinically significant and can have serious consequences. Severe hepatic crisis accounts for over 7% of SCD-related deaths, and 16–29% of individuals with SCD develop cirrhosis. Routine monitoring of liver function tests (LFTs) is essential in patients with SCD to detect early signs of hepatic dysfunction. Optimizing SCD management to reduce the frequency of vaso-occlusive episodes is critical in preventing sickle cell hepatopathy and minimizing long-term liver damage.
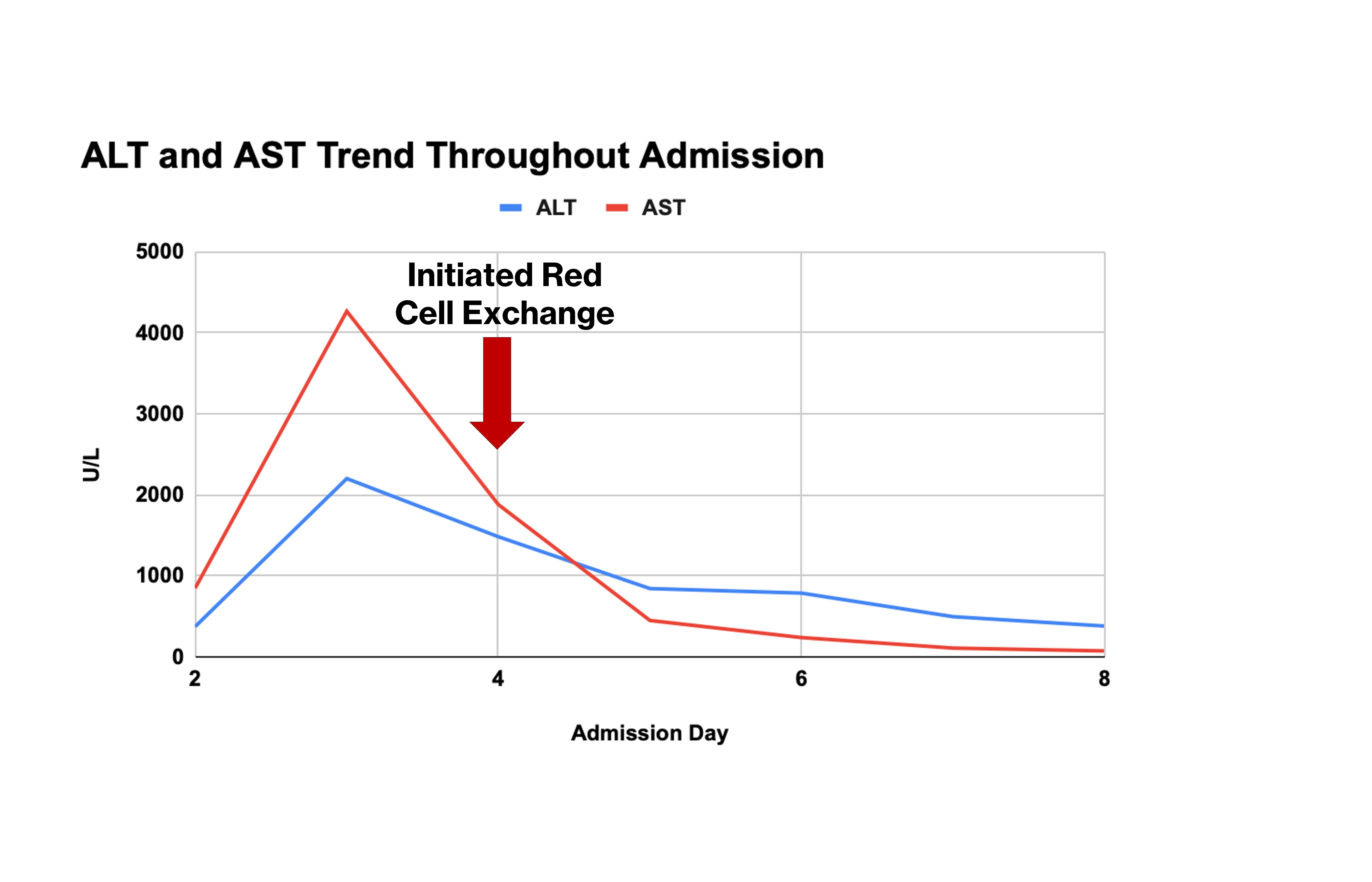
Figure: Figure 1: ALT and AST trend before and after red cell exchange
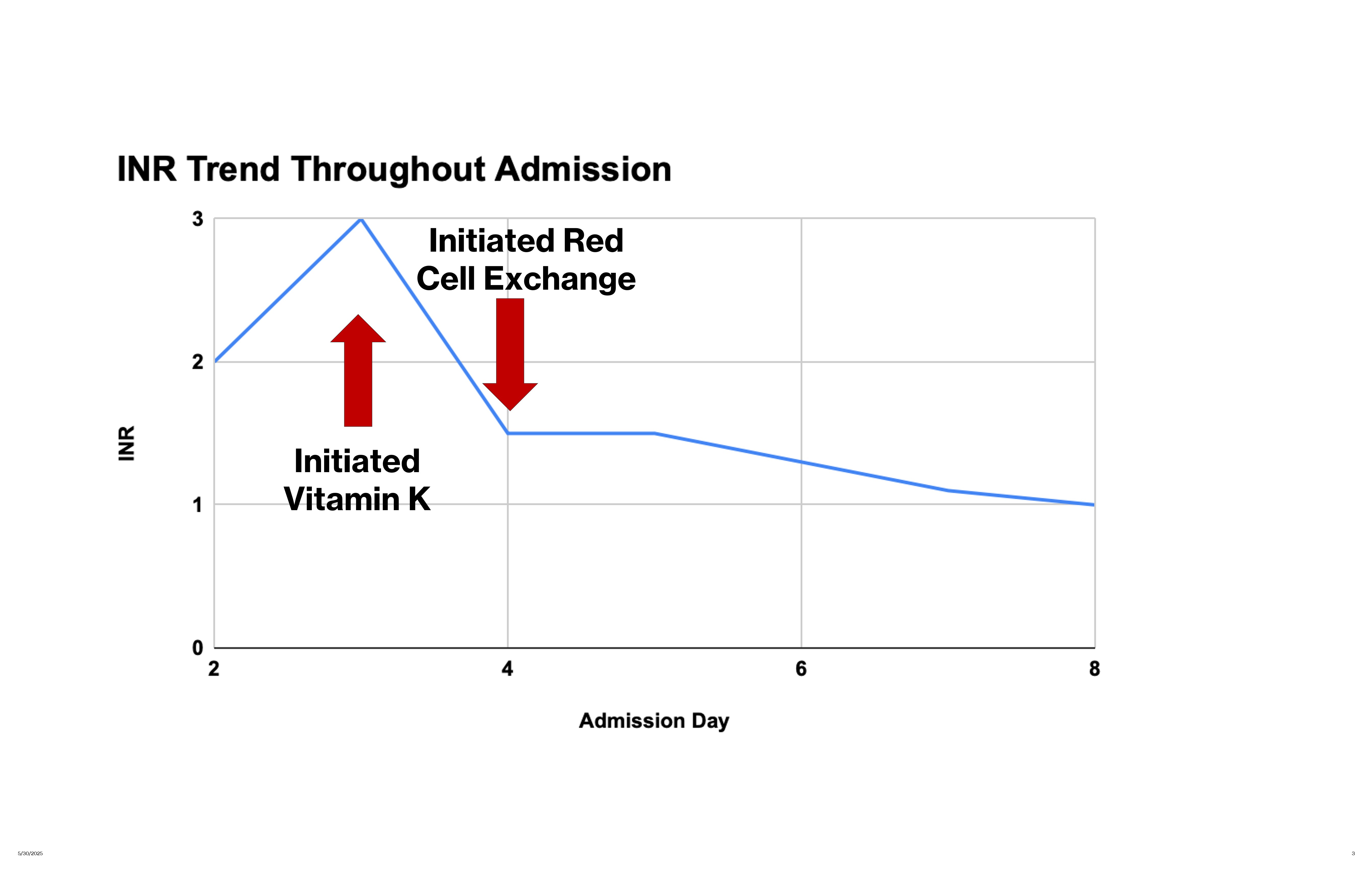
Figure: Figure 2: INR trend before and after Vitamin K and red cell exchange
Disclosures:
Veronica West indicated no relevant financial relationships.
John Sheehy indicated no relevant financial relationships.
Carolyn Hogan indicated no relevant financial relationships.
Miguel Agudelo indicated no relevant financial relationships.
Veronica West, DO1, John Sheehy, BS2, Carolyn Hogan, MD1, Miguel Agudelo, MD1. P6055 - A Rare Case of Severe Hepatic Crisis in a Patient With Sickle Cell Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Acute hepatic vaso-occlusive episodes are seen in approximately 10% of adults with sickle cell disease (SCD). The typical presentation includes RUQ pain, tender hepatomegaly, and aminotransferase levels that rarely surpass 300 units/L. We present a case of a 29-year-old male with sickle cell hemoglobin SC disease who presented with a sickle cell pain crisis found to have towering transaminases secondary to ischemic injury from sickle cell hepatopathy (SCH).
Case Description/
Methods: History was notable for days of extremity, back pain, nausea after a binge alcohol ingestion. The patient was hemodynamically stable and had no encephalopathy. Labs were notable for an alanine aminotransferase of 374 U/L peaking at 2,201 U/L, an aspartate aminotransferase of 849 U/L peaking at 4,267 U/L, prolonged INR of 3.0, and a direct hyperbilirubinemia peaking at 5.1 mg/dl. Viral hepatitides were negative. Contrasted CT showed acute pancreatitis and cholelithiasis, but was negative for choledocholithiasis, cholecystitis, portal vein thrombosis, or outflow obstruction. His only risk factor for liver disease was alcohol use. To decrease the amount of sickling, red cell exchange was used to lower the hemoglobin S-C level. His liver function and enzymes subsequently improved.
Discussion: The rapid improvement in his aminotransferase levels was consistent with ischemic hepatopathy. The likely etiology was SCH, resulting from microvascular vaso-occlusion due to red blood cell sickling within the hepatic vasculature. In SCH, aminotransferase levels typically peak around 300 U/L; values exceeding 1,000 U/L, as seen in this case, are rare. Although hepatic crisis in SCD of this severity are uncommon, they are clinically significant and can have serious consequences. Severe hepatic crisis accounts for over 7% of SCD-related deaths, and 16–29% of individuals with SCD develop cirrhosis. Routine monitoring of liver function tests (LFTs) is essential in patients with SCD to detect early signs of hepatic dysfunction. Optimizing SCD management to reduce the frequency of vaso-occlusive episodes is critical in preventing sickle cell hepatopathy and minimizing long-term liver damage.
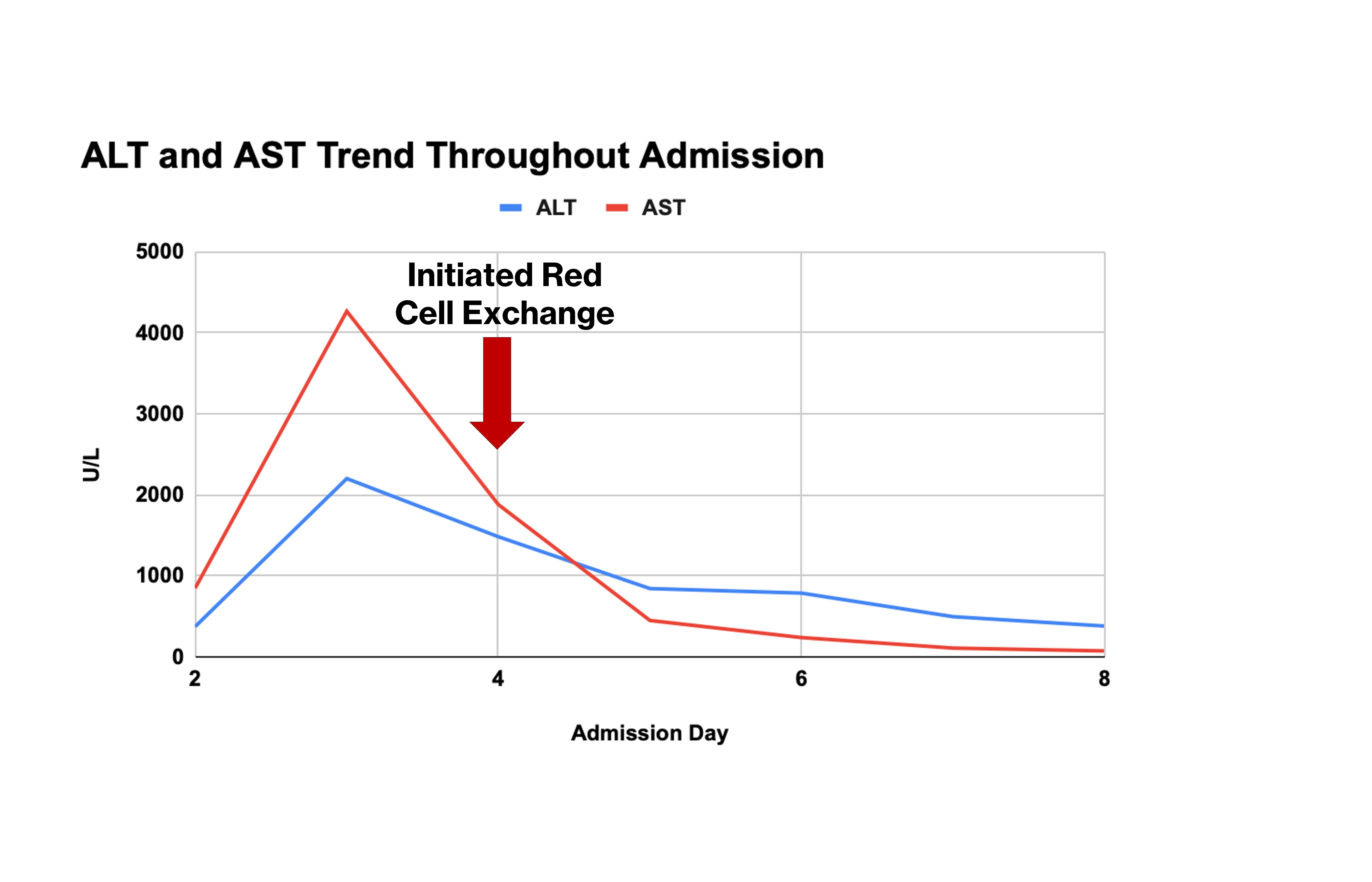
Figure: Figure 1: ALT and AST trend before and after red cell exchange
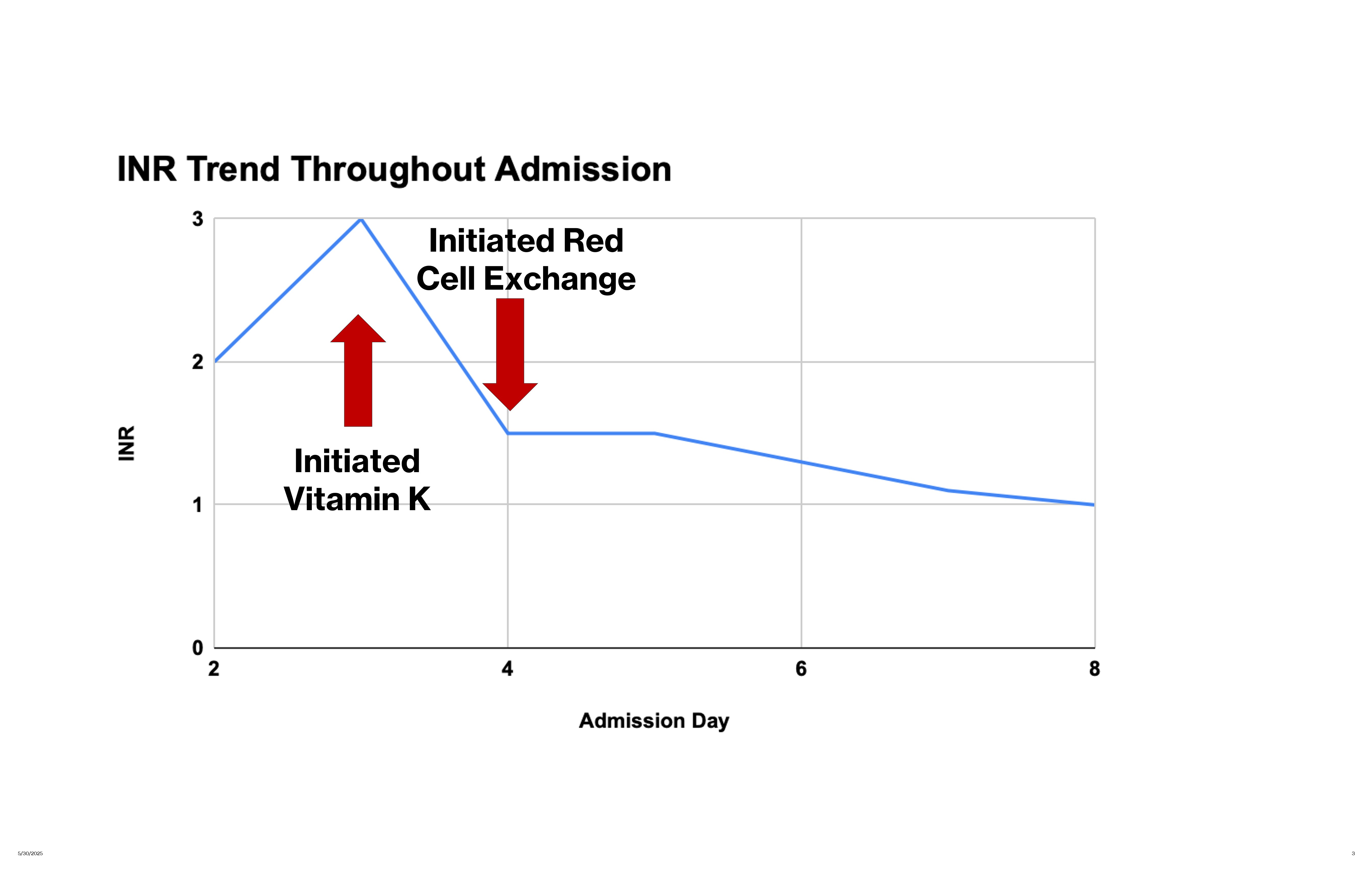
Figure: Figure 2: INR trend before and after Vitamin K and red cell exchange
Disclosures:
Veronica West indicated no relevant financial relationships.
John Sheehy indicated no relevant financial relationships.
Carolyn Hogan indicated no relevant financial relationships.
Miguel Agudelo indicated no relevant financial relationships.
Veronica West, DO1, John Sheehy, BS2, Carolyn Hogan, MD1, Miguel Agudelo, MD1. P6055 - A Rare Case of Severe Hepatic Crisis in a Patient With Sickle Cell Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

