Tuesday Poster Session
Category: Liver
P6048 - Treatment of Dapsone-Induced Methemoglobinemia in a Transplant Recipient With Isosulfan Blue Allergy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Joy Zhao, MD
Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Award: ACG Presidential Poster Award
Joy Zhao, MD1, Caroline Conlon, MD1, Madison Force, MD1, Jamie Schulte, PharmD, BCPS1, Kiran Goli, MD1, Dina Halegoua-DeMarzio, MD2
1Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Few cases highlight the use of cimetidine in dapsone-induced methemoglobinemia (MetHb). This case explores its utility in the setting of an isosulfan blue allergy when methylene blue is not a safe option.
Case Description/
Methods: This is a case of a 69 year old female 1 year post liver transplant (LT) for MASH cirrhosis with HCC and 3 months post kidney transplant (KT) for acute tubular necrosis. 1 month post-LT, pneumocystis jirovecii pneumonia (PJP) prophylaxis was switched from sulfamethoxazole/trimethoprim (SMZ/TMP) to dapsone due to renal impairment. G6PD level was normal (14.3 U/g). Her post-KT course was complicated by leukopenia and anemia. Dapsone was switched to atovaquone, which was not tolerated due to nausea; and was restarted 21 days later. Other medications included tacrolimus, cellcept and valcyte.
She was admitted with dyspnea, fatigue, and lightheadedness. SpO2 was 91% on room air. Cardiopulmonary examination was normal. Labs showed worsening anemia Hgb 8.2 g/dL, MCV 116 fL. The patient had increasing O2 requirement. ABG showed pH 7.42 and pO2 160 mmHg. Chest Xray, CT chest, V-Q scan, and echocardiogram were unremarkable.
Hematological work-up showed haptoglobin < 10 mg/dL and LDH 430 IU/L concerning for hemolysis. Peripheral blood smear had Heinz bodies and bite cells. Methemoglobin was 13.3%.
Dapsone was held due to MethHb. Standard treatment of methylene blue was avoided due to potential cross-reactivity of an anaphylactic allergy to isosulfan blue. Cimetidine 400mg TID was initiated to inhibit the CYP metabolism of dapsone to its toxic hydroxylamine metabolites and continued for 7 doses.
Over 3 days her dyspnea resolved and she transitioned to room air. Methemoglobin levels were trended (Figure 1). She was discharged on alternative PJP prophylaxis (inhaled pentamidine) with labs as follows: Hgb 7.6 g/dL, methemoglobin 1.2%. In 1 week, Hgb improved to 9.3 g/dL.
Discussion: Dapsone is used for PJP prophylaxis post-transplant when SMZ/TMP is not tolerated. MethHb is an adverse effect of dapsone. High index of suspicion is needed to recognize it as a cause of unexplained hypoxemia and anemia in post-transplant patients on dapsone, even with normal G6PD activity.
This case was complicated by potential cross-reactivity of anaphylaxis to isosulfan blue with methylene blue, previously documented in literature. Cimetidine use was weighed with balancing the risks for kidney injury due to acute interstitial nephritis with recent KT with improvement in MethHb.
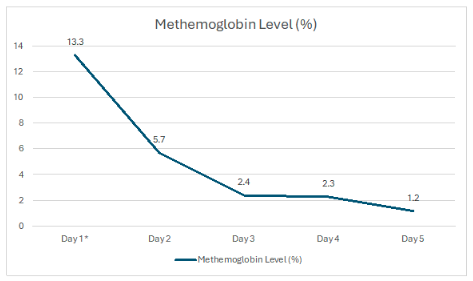
Figure: Figure 1. Methemoglobin Level after Cimetidine Initiation
*Day of Cimetidine 400mg TID for 5 days initiation
Disclosures:
Joy Zhao indicated no relevant financial relationships.
Caroline Conlon indicated no relevant financial relationships.
Madison Force indicated no relevant financial relationships.
Jamie Schulte indicated no relevant financial relationships.
Kiran Goli indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: 89BIO – Grant/Research Support. Akero – Grant/Research Support. Galectin – Grant/Research Support. Madigral – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Novo Nordisk – Grant/Research Support. Vertex – Advisor or Review Panel Member.
Joy Zhao, MD1, Caroline Conlon, MD1, Madison Force, MD1, Jamie Schulte, PharmD, BCPS1, Kiran Goli, MD1, Dina Halegoua-DeMarzio, MD2. P6048 - Treatment of Dapsone-Induced Methemoglobinemia in a Transplant Recipient With Isosulfan Blue Allergy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Joy Zhao, MD1, Caroline Conlon, MD1, Madison Force, MD1, Jamie Schulte, PharmD, BCPS1, Kiran Goli, MD1, Dina Halegoua-DeMarzio, MD2
1Thomas Jefferson University, Philadelphia, PA; 2Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Few cases highlight the use of cimetidine in dapsone-induced methemoglobinemia (MetHb). This case explores its utility in the setting of an isosulfan blue allergy when methylene blue is not a safe option.
Case Description/
Methods: This is a case of a 69 year old female 1 year post liver transplant (LT) for MASH cirrhosis with HCC and 3 months post kidney transplant (KT) for acute tubular necrosis. 1 month post-LT, pneumocystis jirovecii pneumonia (PJP) prophylaxis was switched from sulfamethoxazole/trimethoprim (SMZ/TMP) to dapsone due to renal impairment. G6PD level was normal (14.3 U/g). Her post-KT course was complicated by leukopenia and anemia. Dapsone was switched to atovaquone, which was not tolerated due to nausea; and was restarted 21 days later. Other medications included tacrolimus, cellcept and valcyte.
She was admitted with dyspnea, fatigue, and lightheadedness. SpO2 was 91% on room air. Cardiopulmonary examination was normal. Labs showed worsening anemia Hgb 8.2 g/dL, MCV 116 fL. The patient had increasing O2 requirement. ABG showed pH 7.42 and pO2 160 mmHg. Chest Xray, CT chest, V-Q scan, and echocardiogram were unremarkable.
Hematological work-up showed haptoglobin < 10 mg/dL and LDH 430 IU/L concerning for hemolysis. Peripheral blood smear had Heinz bodies and bite cells. Methemoglobin was 13.3%.
Dapsone was held due to MethHb. Standard treatment of methylene blue was avoided due to potential cross-reactivity of an anaphylactic allergy to isosulfan blue. Cimetidine 400mg TID was initiated to inhibit the CYP metabolism of dapsone to its toxic hydroxylamine metabolites and continued for 7 doses.
Over 3 days her dyspnea resolved and she transitioned to room air. Methemoglobin levels were trended (Figure 1). She was discharged on alternative PJP prophylaxis (inhaled pentamidine) with labs as follows: Hgb 7.6 g/dL, methemoglobin 1.2%. In 1 week, Hgb improved to 9.3 g/dL.
Discussion: Dapsone is used for PJP prophylaxis post-transplant when SMZ/TMP is not tolerated. MethHb is an adverse effect of dapsone. High index of suspicion is needed to recognize it as a cause of unexplained hypoxemia and anemia in post-transplant patients on dapsone, even with normal G6PD activity.
This case was complicated by potential cross-reactivity of anaphylaxis to isosulfan blue with methylene blue, previously documented in literature. Cimetidine use was weighed with balancing the risks for kidney injury due to acute interstitial nephritis with recent KT with improvement in MethHb.
Figure: Figure 1. Methemoglobin Level after Cimetidine Initiation
*Day of Cimetidine 400mg TID for 5 days initiation
Disclosures:
Joy Zhao indicated no relevant financial relationships.
Caroline Conlon indicated no relevant financial relationships.
Madison Force indicated no relevant financial relationships.
Jamie Schulte indicated no relevant financial relationships.
Kiran Goli indicated no relevant financial relationships.
Dina Halegoua-DeMarzio: 89BIO – Grant/Research Support. Akero – Grant/Research Support. Galectin – Grant/Research Support. Madigral – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Novo Nordisk – Grant/Research Support. Vertex – Advisor or Review Panel Member.
Joy Zhao, MD1, Caroline Conlon, MD1, Madison Force, MD1, Jamie Schulte, PharmD, BCPS1, Kiran Goli, MD1, Dina Halegoua-DeMarzio, MD2. P6048 - Treatment of Dapsone-Induced Methemoglobinemia in a Transplant Recipient With Isosulfan Blue Allergy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

