Tuesday Poster Session
Category: Liver
P6151 - An Unexpected Turn: Jejunal Varices in Post-Transplant Alagille Syndrome
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JL
Jinye Liu, DO
East Carolina University Medical Center
Greenville, NC
Presenting Author(s)
Jinye Liu, DO1, Kayleigh C. Lewis, MD2, Daniel Gildea, MD3, Sahaj Rathi, MD3, Sanjeev Jairath, MD3
1East Carolina University Medical Center, Greenville, NC; 2Mountain Area Health Education Center, Asheville, NC; 3Virginia Commonwealth University Medical Center, Richmond, VA
Introduction: Alagille syndrome is a rare genetic disorder (~1 in 70,000) affecting multiple organs; hepatic involvement can manifest as cholestasis from bile duct paucity. Symptoms may include conjugated hyperbilirubinemia, xanthomas, and pruritus, and up to 15% develop end-stage liver disease. Additionally, jejunal varices may form. These rare occurrences arise from prior radiation, portal and/or splanchnic vein thrombosis, or surgery, and can cause hemorrhagic shock.
Case Description/
Methods: A 37-year-old African American male with Alagille syndrome with deceased donor liver transplant (DDLT) at age 4 on tacrolimus presented with hemorrhagic shock from a gastrointestinal bleed. History included biliary anastomotic stricture with hepaticojejunostomy, percutaneous cholecystostomy, allograft cirrhosis with portal hypertension, multiple varices, splenomegaly s/p splenic artery embolization (Figure 1), chronic portal, mesenteric, and splenic vein thrombosis, and neuroendocrine tumor with mesenteric metastasis s/p bowel resection.
The patient had multiple prior admissions for GIB. CTA showed a 15cm cluster of jejunal varices at the anastomotic site (Figure 1) and esophageal varices (EV), which were confirmed alongside duodenal varices on EGD (Figure 2). This time he had a hemoglobin of 7 (baseline 9) and hematochezia. He was transfused; bleeding resolved spontaneously, per usual. MELD was 13 (INR low 1, creatine mid 1, platelets 30k, sodium normal, all baseline), with his ALP and AST chronically elevated in the 300s and 50s, respectively. ALT was normal.
Discussion: This case is unique as there are no reports of jejunal varices after DDLT in Alagille syndrome. His ectopic varices are likely related to prior hepaticojejunostomy and graft cirrhosis (thus portal thrombosis). Treatments in literature include endoscopic sclerotherapy, coil embolization, small bowel resection (SBR), and TIPS. Decisions must be individualized.
TIPS was not feasible due to extensive thrombosis in our patient. IR-guided embolization and re-transplantation was also limited by vasculature due to thrombosis. SBR required creating a new anastomosis, with high recurrence risk without treating underlying liver disease. Multivisceral transplant was contemplated but limited due to high mortality and thrombosis.
Double-balloon sclerotherapy would be technically challenging because of depth and would only be temporizing; also, it may injure the varices. The patient continues with hepatology follow-up, with treatment pending further discussion.
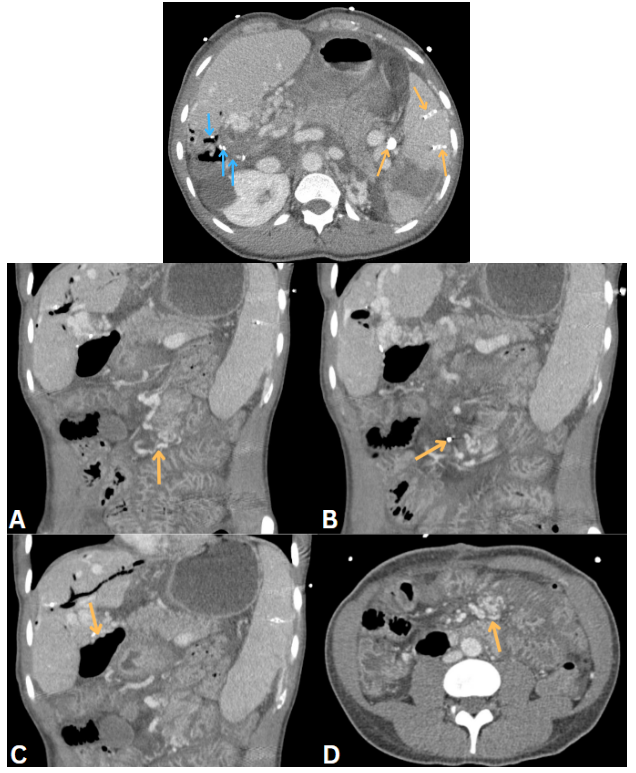
Figure: Figure 1. Blue arrows demonstrating old stables from hepaticojejunostomy and yellow arrows demonstrating coils from splenic embolization (top figure). (A): Yellow arrow pointing to a vascular cluster in the jejunal region of the small bowel. (B): Yellow arrow pointing to mechanical clip with shadowing used in anastomosis site in the jejunum. (C): Further irregular notches representing likely varices located at the hepaticojejunostomy site. (D): Axial view of the patient's small bowel, with the yellow arrow pointing towards jejunal varices.
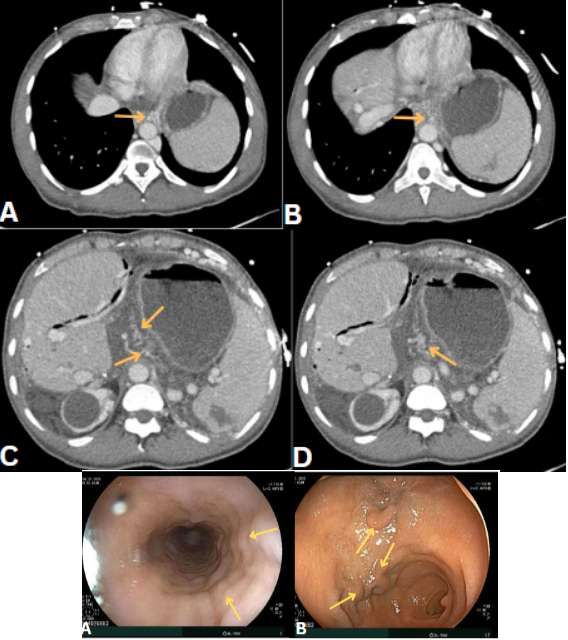
Figure: Figure 2. (A-D): Axial views of yellow arrow pointing to esophageal varices, traced and followed cranially to caudally. Bottom demonstrating esophageal varices (A), and duodenal bulb varices (B) on EGD.
Disclosures:
Jinye Liu indicated no relevant financial relationships.
Kayleigh Lewis indicated no relevant financial relationships.
Daniel Gildea indicated no relevant financial relationships.
Sahaj Rathi indicated no relevant financial relationships.
Sanjeev Jairath indicated no relevant financial relationships.
Jinye Liu, DO1, Kayleigh C. Lewis, MD2, Daniel Gildea, MD3, Sahaj Rathi, MD3, Sanjeev Jairath, MD3. P6151 - An Unexpected Turn: Jejunal Varices in Post-Transplant Alagille Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1East Carolina University Medical Center, Greenville, NC; 2Mountain Area Health Education Center, Asheville, NC; 3Virginia Commonwealth University Medical Center, Richmond, VA
Introduction: Alagille syndrome is a rare genetic disorder (~1 in 70,000) affecting multiple organs; hepatic involvement can manifest as cholestasis from bile duct paucity. Symptoms may include conjugated hyperbilirubinemia, xanthomas, and pruritus, and up to 15% develop end-stage liver disease. Additionally, jejunal varices may form. These rare occurrences arise from prior radiation, portal and/or splanchnic vein thrombosis, or surgery, and can cause hemorrhagic shock.
Case Description/
Methods: A 37-year-old African American male with Alagille syndrome with deceased donor liver transplant (DDLT) at age 4 on tacrolimus presented with hemorrhagic shock from a gastrointestinal bleed. History included biliary anastomotic stricture with hepaticojejunostomy, percutaneous cholecystostomy, allograft cirrhosis with portal hypertension, multiple varices, splenomegaly s/p splenic artery embolization (Figure 1), chronic portal, mesenteric, and splenic vein thrombosis, and neuroendocrine tumor with mesenteric metastasis s/p bowel resection.
The patient had multiple prior admissions for GIB. CTA showed a 15cm cluster of jejunal varices at the anastomotic site (Figure 1) and esophageal varices (EV), which were confirmed alongside duodenal varices on EGD (Figure 2). This time he had a hemoglobin of 7 (baseline 9) and hematochezia. He was transfused; bleeding resolved spontaneously, per usual. MELD was 13 (INR low 1, creatine mid 1, platelets 30k, sodium normal, all baseline), with his ALP and AST chronically elevated in the 300s and 50s, respectively. ALT was normal.
Discussion: This case is unique as there are no reports of jejunal varices after DDLT in Alagille syndrome. His ectopic varices are likely related to prior hepaticojejunostomy and graft cirrhosis (thus portal thrombosis). Treatments in literature include endoscopic sclerotherapy, coil embolization, small bowel resection (SBR), and TIPS. Decisions must be individualized.
TIPS was not feasible due to extensive thrombosis in our patient. IR-guided embolization and re-transplantation was also limited by vasculature due to thrombosis. SBR required creating a new anastomosis, with high recurrence risk without treating underlying liver disease. Multivisceral transplant was contemplated but limited due to high mortality and thrombosis.
Double-balloon sclerotherapy would be technically challenging because of depth and would only be temporizing; also, it may injure the varices. The patient continues with hepatology follow-up, with treatment pending further discussion.
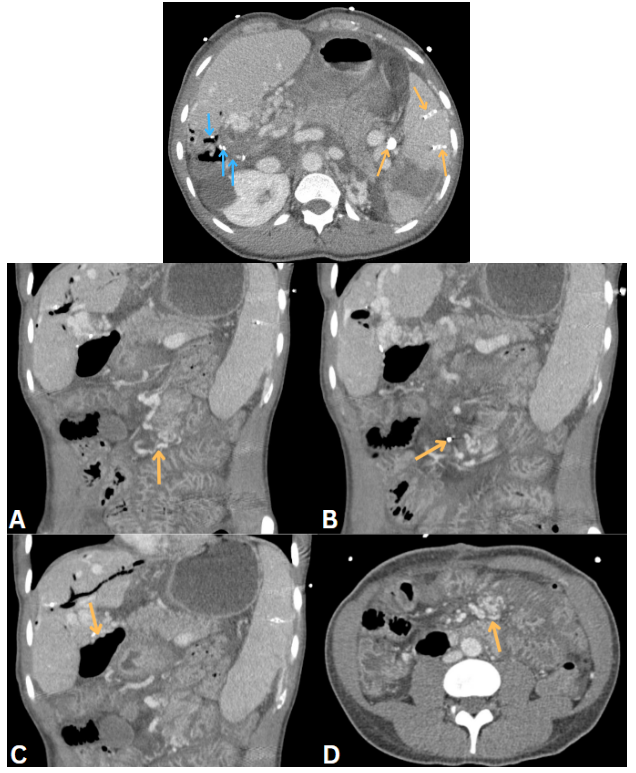
Figure: Figure 1. Blue arrows demonstrating old stables from hepaticojejunostomy and yellow arrows demonstrating coils from splenic embolization (top figure). (A): Yellow arrow pointing to a vascular cluster in the jejunal region of the small bowel. (B): Yellow arrow pointing to mechanical clip with shadowing used in anastomosis site in the jejunum. (C): Further irregular notches representing likely varices located at the hepaticojejunostomy site. (D): Axial view of the patient's small bowel, with the yellow arrow pointing towards jejunal varices.
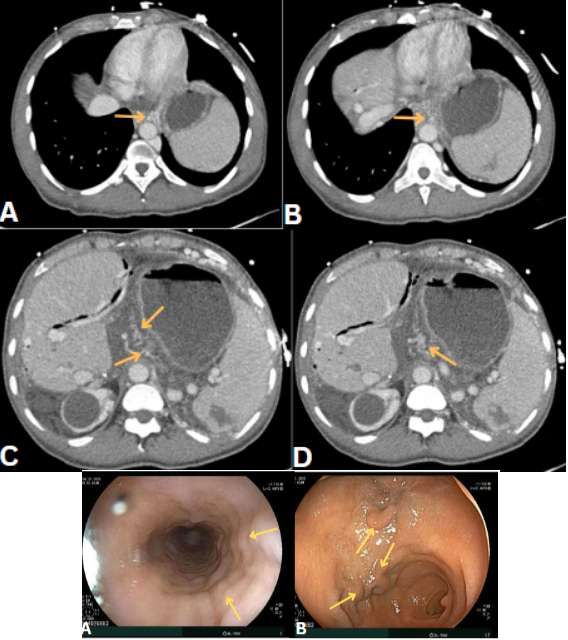
Figure: Figure 2. (A-D): Axial views of yellow arrow pointing to esophageal varices, traced and followed cranially to caudally. Bottom demonstrating esophageal varices (A), and duodenal bulb varices (B) on EGD.
Disclosures:
Jinye Liu indicated no relevant financial relationships.
Kayleigh Lewis indicated no relevant financial relationships.
Daniel Gildea indicated no relevant financial relationships.
Sahaj Rathi indicated no relevant financial relationships.
Sanjeev Jairath indicated no relevant financial relationships.
Jinye Liu, DO1, Kayleigh C. Lewis, MD2, Daniel Gildea, MD3, Sahaj Rathi, MD3, Sanjeev Jairath, MD3. P6151 - An Unexpected Turn: Jejunal Varices in Post-Transplant Alagille Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
