Tuesday Poster Session
Category: Liver
P6139 - Concurrent HBsAg and Anti-HBs Positivity in Chronic Hepatitis B: Atypical Serologic Profile Raising Concern for Immune Escape Variants
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NA
Nabiha Atiquzzaman, BS
Nova Southeastern University College Of Osteopathic Medicine
Davie, FL
Presenting Author(s)
Michael Thomas. Hsieh, BS1, Nabiha Atiquzzaman, BS2, Srinivas Seela, MD3, Harinath Sheela, MD4, Seth Lipka, MD4
1University of Central Florida College of Medicine, San Ramon, CA; 2Nova Southeastern University College Of Osteopathic Medicine, Davie, FL; 3Digestive and Liver Center of Florida, LLC, Orlando, FL; 4Digestive and Liver Center of Florida, Orlando, FL
Introduction: Hepatitis B Virus (HBV) infection is the most common infectious cause of chronic hepatitis, and management is typically based on its well-characterized serological course. Presence of HBsAg, HBV DNA, HBeAg and anti-Hbc IgM indicate acute infection, while presence of Anti-HBs and Anti-HBe indicate recovery. Rarely, patients have been documented to present with atypical serological profiles, complicating management. We present a case of a patient with prolonged concurrent HBsAg and anti-HBs positivity in the absence of liver fibrosis or dysfunction, a presentation that raises diagnostic and management challenges.
Case Description/
Methods: The patient is a 47 year old Hispanic male with a history of unspecified hepatitis presented in 2019 for GERD. He denied a history of alcohol use, IV drug use, or multiple sexual partners. Evaluation was unremarkable, and he was lost to follow-up. Serology workup during 2020-2021 revealed positive HBV DNA, anti-HBe, and concurrent HBsAg and anti-HBs. However, liver ultrasound revealed only mild hepatic steatosis and LFTs were within normal limits. Given low HBV DNA titer and normal LFTs, treatment was deferred.
The patient was lost to follow-up after 2022, returning in 2024 with epigastric pain. HBV serology continued to demonstrate persistent positive HBsAg, anti-HBs and HBV DNA. Liver elastography and needle core biopsy demonstrated chronic hepatitis without fibrosis, steatosis or significant inflammation (METAVIR F0-F1; Batts-Ludwig Grade 0, Stage 0). Immunostain for HBsAg was negative. Biopsy demonstrated no structural abnormalities, and iron, copper, reticulin, trichrome, PAS with diastase stains were normal.
Discussion: This patient’s atypical HBV serologic profile and low-level viremia in the absence of liver fibrosis represent a diagnostic scenario that may reflect low-replicative chronic infection. The patient’s persistent HBsAg raises the possibility of impaired immune clearance, or immune escape variants. Although genotypic confirmation was not pursued, future genotypic analysis may help identify immune escape and preC/C variants in the case of declining liver function, to guide therapeutic options.
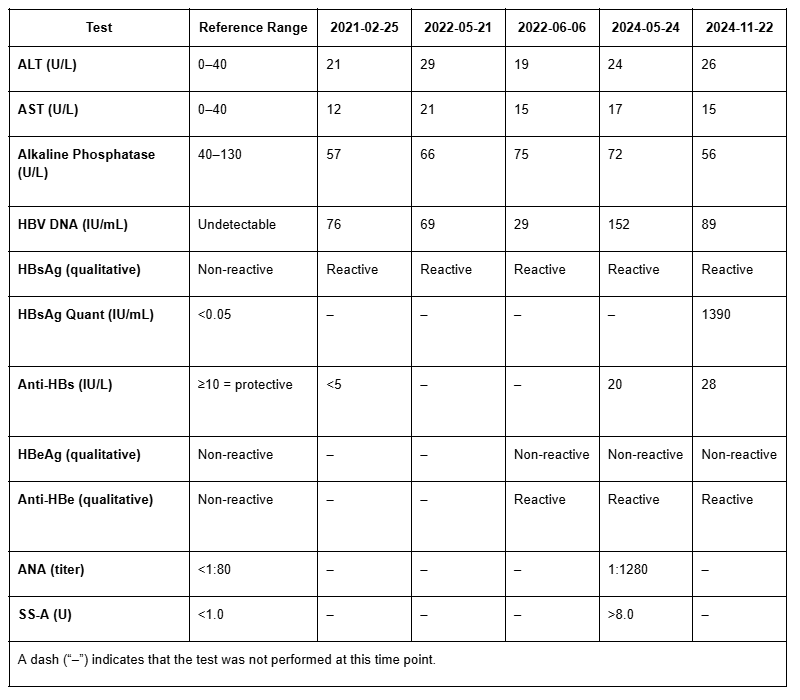
Figure: Table 1. Longitudinal Laboratory and Serologic Data Demonstrates Stable Liver Enzymes and Persistent Low-Level HBV Viremia
Serial laboratory results from 2021 to 2024 demonstrate normal liver function tests (ALT, AST, ALP), persistently low-level detectable HBV DNA, and concurrent HBsAg and anti-HBs positivity. The patient remained HBeAg-negative with consistent anti-HBe reactivity. Autoimmune markers (ANA and SS-A) were elevated in 2024. The patient had no evidence of liver function impairment, fibrosis or inflammation.
Disclosures:
Michael Hsieh indicated no relevant financial relationships.
Nabiha Atiquzzaman indicated no relevant financial relationships.
Srinivas Seela indicated no relevant financial relationships.
Harinath Sheela indicated no relevant financial relationships.
Seth Lipka indicated no relevant financial relationships.
Michael Thomas. Hsieh, BS1, Nabiha Atiquzzaman, BS2, Srinivas Seela, MD3, Harinath Sheela, MD4, Seth Lipka, MD4. P6139 - Concurrent HBsAg and Anti-HBs Positivity in Chronic Hepatitis B: Atypical Serologic Profile Raising Concern for Immune Escape Variants, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida College of Medicine, San Ramon, CA; 2Nova Southeastern University College Of Osteopathic Medicine, Davie, FL; 3Digestive and Liver Center of Florida, LLC, Orlando, FL; 4Digestive and Liver Center of Florida, Orlando, FL
Introduction: Hepatitis B Virus (HBV) infection is the most common infectious cause of chronic hepatitis, and management is typically based on its well-characterized serological course. Presence of HBsAg, HBV DNA, HBeAg and anti-Hbc IgM indicate acute infection, while presence of Anti-HBs and Anti-HBe indicate recovery. Rarely, patients have been documented to present with atypical serological profiles, complicating management. We present a case of a patient with prolonged concurrent HBsAg and anti-HBs positivity in the absence of liver fibrosis or dysfunction, a presentation that raises diagnostic and management challenges.
Case Description/
Methods: The patient is a 47 year old Hispanic male with a history of unspecified hepatitis presented in 2019 for GERD. He denied a history of alcohol use, IV drug use, or multiple sexual partners. Evaluation was unremarkable, and he was lost to follow-up. Serology workup during 2020-2021 revealed positive HBV DNA, anti-HBe, and concurrent HBsAg and anti-HBs. However, liver ultrasound revealed only mild hepatic steatosis and LFTs were within normal limits. Given low HBV DNA titer and normal LFTs, treatment was deferred.
The patient was lost to follow-up after 2022, returning in 2024 with epigastric pain. HBV serology continued to demonstrate persistent positive HBsAg, anti-HBs and HBV DNA. Liver elastography and needle core biopsy demonstrated chronic hepatitis without fibrosis, steatosis or significant inflammation (METAVIR F0-F1; Batts-Ludwig Grade 0, Stage 0). Immunostain for HBsAg was negative. Biopsy demonstrated no structural abnormalities, and iron, copper, reticulin, trichrome, PAS with diastase stains were normal.
Discussion: This patient’s atypical HBV serologic profile and low-level viremia in the absence of liver fibrosis represent a diagnostic scenario that may reflect low-replicative chronic infection. The patient’s persistent HBsAg raises the possibility of impaired immune clearance, or immune escape variants. Although genotypic confirmation was not pursued, future genotypic analysis may help identify immune escape and preC/C variants in the case of declining liver function, to guide therapeutic options.
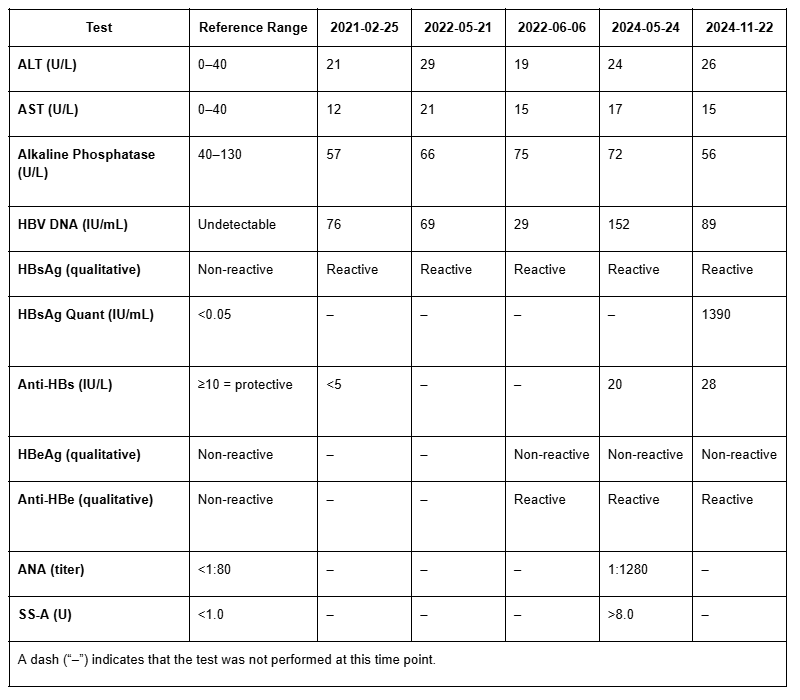
Figure: Table 1. Longitudinal Laboratory and Serologic Data Demonstrates Stable Liver Enzymes and Persistent Low-Level HBV Viremia
Serial laboratory results from 2021 to 2024 demonstrate normal liver function tests (ALT, AST, ALP), persistently low-level detectable HBV DNA, and concurrent HBsAg and anti-HBs positivity. The patient remained HBeAg-negative with consistent anti-HBe reactivity. Autoimmune markers (ANA and SS-A) were elevated in 2024. The patient had no evidence of liver function impairment, fibrosis or inflammation.
Disclosures:
Michael Hsieh indicated no relevant financial relationships.
Nabiha Atiquzzaman indicated no relevant financial relationships.
Srinivas Seela indicated no relevant financial relationships.
Harinath Sheela indicated no relevant financial relationships.
Seth Lipka indicated no relevant financial relationships.
Michael Thomas. Hsieh, BS1, Nabiha Atiquzzaman, BS2, Srinivas Seela, MD3, Harinath Sheela, MD4, Seth Lipka, MD4. P6139 - Concurrent HBsAg and Anti-HBs Positivity in Chronic Hepatitis B: Atypical Serologic Profile Raising Concern for Immune Escape Variants, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
