Tuesday Poster Session
Category: Small Intestine
P6236 - The Yellow Flag: A Rare Case of Primary Renal Cell Carcinoma Presenting as Obstructive Jaundice
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shaina Ailawadi, MD
Case Western Reserve University/University Hospitals
University Heights, OH
Presenting Author(s)
Leah Z. Montgomery, MD1, Shaina Ailawadi, MD1, Carine Bou-Abboud Matta, MD2
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Obstructive jaundice secondary to malignancy is most commonly attributed to primary tumors originating in the liver, pancreas, biliary tree, or duodenum, as well as their associated metastases. When renal cell carcinoma (RCC) results in hepatic dysfunction, it is typically due to direct extension into the inferior vena cava leading to Budd-Chiari syndrome, hepatic metastases, or paraneoplastic phenomena such as Stauffer syndrome. To date, there have been no documented reports of RCC causing obstructive jaundice via direct invasion into the small bowel. We describe a rare case of obstructive jaundice resulting from locally advanced RCC with direct transmural invasion of the small intestine - an unusual and, to our knowledge, previously unreported clinical presentation.
Case Description/
Methods: A 68-year-old female with a history of hypertension and hyperlipidemia presented with a three-week history of fatigue, gastric reflux, post-prandial fullness, and jaundice. Laboratory results showed a lipase of 42 U/L, ALP 1,160, ALT 291, AST 230, total bilirubin 10.0, and direct bilirubin 6.1. A CT scan revealed a 6.1cm mass in the upper pole of the right kidney with exophytic extension obstructing the distal common bile duct (CBD) and invading the early duodenum (Figure 1a). MRI confirmed a partially exophytic mass in the right kidney, suggesting renal cell carcinoma with invasion into the renal vein, the first and second duodenal segments, and obstruction at the ampulla, leading to bile duct dilation (Figure 1b). Esophagogastroduodenoscopy (EGD) showed an obstructing mass in the distal duodenal bulb, extrinsically compressing and eroding the duodenal wall with ulceration. No malignancy was identified on biopsy (Figure 2). A biopsy of the right renal mass confirmed RCC, clear cell type. To relieve hepatic congestion, a biliary drainage catheter was initially placed. The patient subsequently underwent a Whipple procedure, right nephrectomy, and regional lymphadenectomy. Further imaging revealed no distant metastases.
Discussion: We present this rare case of a locally advanced RCC primary mass with direct invasion into the duodenum resulting in significant obstructive jaundice. This case is a unique manifestation of direct invasion from RCC into the biliary system. Clinicians should consider a wide differential diagnosis when evaluating patients who present with obstructive jaundice, employing a multimodal strategy inclusive of imaging, endoscopy, and collaboration with a multidisciplinary team.
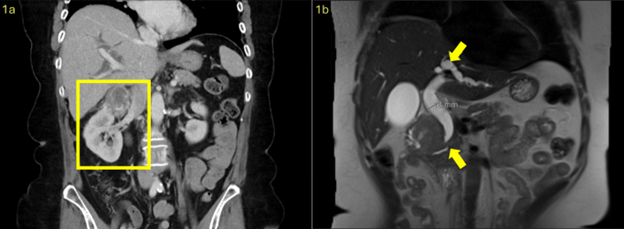
Figure: Figure 1: CT scan of mass in the upper pole of the right kidney (Figure 1a). MRI of right upper pole renal mass causing obstruction at the level of the ampulla (bottom arrow) resulting in dilation of the CBD and intrahepatic bile ducts (top arrow) (Figure 1b).
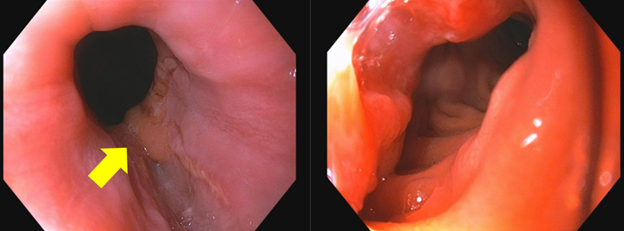
Figure: Figure 2: EGD images showing nearly obstructing mass at the distal duodenal bulb, secondary to extrinsic compression, and erosion through the duodenal wall with ulceration (arrow).
Disclosures:
Leah Montgomery indicated no relevant financial relationships.
Shaina Ailawadi indicated no relevant financial relationships.
Carine Bou-Abboud Matta indicated no relevant financial relationships.
Leah Z. Montgomery, MD1, Shaina Ailawadi, MD1, Carine Bou-Abboud Matta, MD2. P6236 - The Yellow Flag: A Rare Case of Primary Renal Cell Carcinoma Presenting as Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Obstructive jaundice secondary to malignancy is most commonly attributed to primary tumors originating in the liver, pancreas, biliary tree, or duodenum, as well as their associated metastases. When renal cell carcinoma (RCC) results in hepatic dysfunction, it is typically due to direct extension into the inferior vena cava leading to Budd-Chiari syndrome, hepatic metastases, or paraneoplastic phenomena such as Stauffer syndrome. To date, there have been no documented reports of RCC causing obstructive jaundice via direct invasion into the small bowel. We describe a rare case of obstructive jaundice resulting from locally advanced RCC with direct transmural invasion of the small intestine - an unusual and, to our knowledge, previously unreported clinical presentation.
Case Description/
Methods: A 68-year-old female with a history of hypertension and hyperlipidemia presented with a three-week history of fatigue, gastric reflux, post-prandial fullness, and jaundice. Laboratory results showed a lipase of 42 U/L, ALP 1,160, ALT 291, AST 230, total bilirubin 10.0, and direct bilirubin 6.1. A CT scan revealed a 6.1cm mass in the upper pole of the right kidney with exophytic extension obstructing the distal common bile duct (CBD) and invading the early duodenum (Figure 1a). MRI confirmed a partially exophytic mass in the right kidney, suggesting renal cell carcinoma with invasion into the renal vein, the first and second duodenal segments, and obstruction at the ampulla, leading to bile duct dilation (Figure 1b). Esophagogastroduodenoscopy (EGD) showed an obstructing mass in the distal duodenal bulb, extrinsically compressing and eroding the duodenal wall with ulceration. No malignancy was identified on biopsy (Figure 2). A biopsy of the right renal mass confirmed RCC, clear cell type. To relieve hepatic congestion, a biliary drainage catheter was initially placed. The patient subsequently underwent a Whipple procedure, right nephrectomy, and regional lymphadenectomy. Further imaging revealed no distant metastases.
Discussion: We present this rare case of a locally advanced RCC primary mass with direct invasion into the duodenum resulting in significant obstructive jaundice. This case is a unique manifestation of direct invasion from RCC into the biliary system. Clinicians should consider a wide differential diagnosis when evaluating patients who present with obstructive jaundice, employing a multimodal strategy inclusive of imaging, endoscopy, and collaboration with a multidisciplinary team.
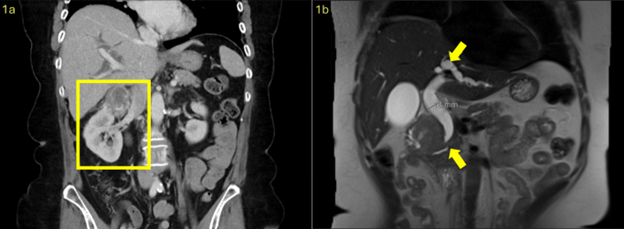
Figure: Figure 1: CT scan of mass in the upper pole of the right kidney (Figure 1a). MRI of right upper pole renal mass causing obstruction at the level of the ampulla (bottom arrow) resulting in dilation of the CBD and intrahepatic bile ducts (top arrow) (Figure 1b).
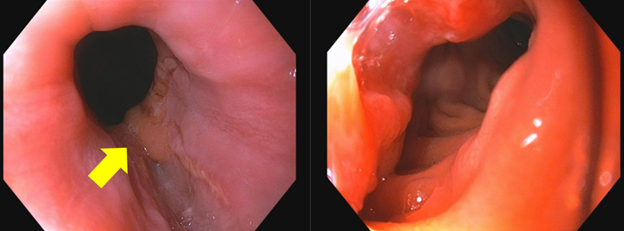
Figure: Figure 2: EGD images showing nearly obstructing mass at the distal duodenal bulb, secondary to extrinsic compression, and erosion through the duodenal wall with ulceration (arrow).
Disclosures:
Leah Montgomery indicated no relevant financial relationships.
Shaina Ailawadi indicated no relevant financial relationships.
Carine Bou-Abboud Matta indicated no relevant financial relationships.
Leah Z. Montgomery, MD1, Shaina Ailawadi, MD1, Carine Bou-Abboud Matta, MD2. P6236 - The Yellow Flag: A Rare Case of Primary Renal Cell Carcinoma Presenting as Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
