Tuesday Poster Session
Category: Small Intestine
P6218 - Duodenal Metastasis From Nasopharyngeal Carcinoma: A Case Report of an Uncommon Metastatic Site
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ethan Abrishamian, DO
NYC Health + Hospitals - - New York, NY
Roslyn Heights, NY
Presenting Author(s)
Ethan Abrishamian, DO1, Niyaz Arif, MD1, Prasad Rajalingamgari, MD1, Justin Wagner, DO2, Akil Olliverre, MD3, Michael Bernstein, MD2
1NYC Health + Hospitals - - New York, NY, Roslyn Heights, NY; 2NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 3NYC Health + Hospitals/South Brooklyn Health, New York, NY
Introduction: Nasopharyngeal carcinoma (NPC) is a rare malignancy with variable metastatic patterns, most commonly to bone, lymph nodes, liver, and lungs (1). Gastrointestinal (GI) involvement is exceedingly rare; one report identified only five cases (2). We present a rare case of duodenal metastasis from NPC, highlighting an uncommon pattern of dissemination (3).
Case Description/
Methods: A 50-year-old Asian American male with stage IVb WHO type II NPC, diagnosed in 2014 with cerebral and hepatic metastases, presented with hypotension (83/53 mmHg), abdominal pain, coffee-ground emesis, and 30-lb weight loss over three months. Exam showed cachexia, jaundice, and epigastric tenderness.
Labs revealed marked hepatocellular injury (AST 6000 U/L, ALT 1700 U/L), cholestasis (ALP 500 U/L), hypoalbuminemia (2.0 g/dL), leukocytosis (27 × 10³/μL), anemia (6.7 g/dL), thrombocytopenia (116 × 10³/μL), and coagulopathy (INR 5.15). CT abdomen showed progression of hepatic metastases (Fig. 1). The patient was admitted to ICU, where he developed hematemesis requiring massive transfusion. EGD revealed a large, actively bleeding duodenal mass (Fig. 2). Despite aggressive resuscitation, the patient expired shortly after.
Discussion: NPC is rare globally but more common in East and Southeast Asia. WHO type II NPC is aggressive with a high rate of distant metastasis, though GI spread, especially to the duodenum, is extremely rare (4). In this case, the patient presented with hypotension, anemia, weight loss, and GI bleeding. Endoscopy showed an ulcerated, fungating, and partially obstructive duodenal mass. Though biopsy was precluded by bleeding risk, the endoscopic appearance and clinical history strongly supported duodenal metastasis.
Primary GI malignancies (e.g., adenocarcinoma, GIST, lymphoma) were considered but deemed unlikely due to lack of risk factors and close temporal association with systemic disease progression. Rare reports of duodenal metastases from NPC exist, often presenting with GI bleeding or obstruction (5,6). Autopsy studies also reveal small bowel involvement in advanced NPC (7).
This case underscores the importance of considering GI metastasis in NPC patients with GI symptoms and the diagnostic challenges when biopsy is not feasible.
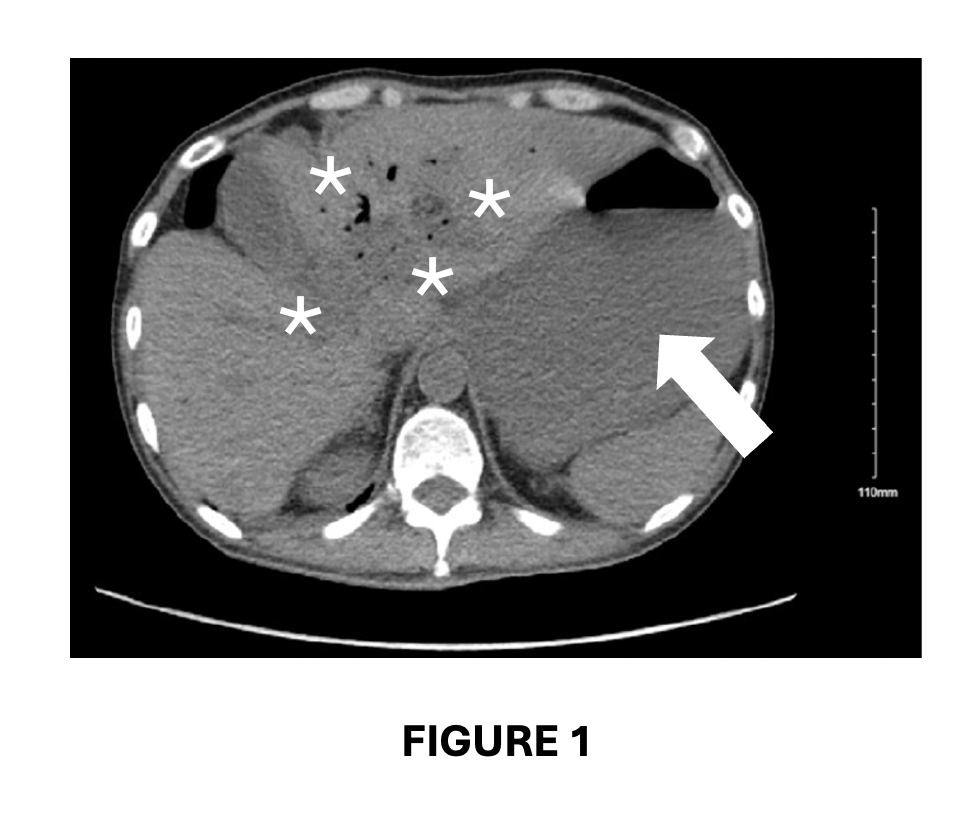
Figure: Figure 1:
Contrast-enhanced CT of the Abdomen and Pelvis.
Multiple hypodense, solid, round lesions are seen in the left hepatic lobe (indicated by asterisks), and a similar hypodense lesion is noted in the right hepatic lobe (indicated by the arrow). These findings are suspicious for hepatic metastatic disease.
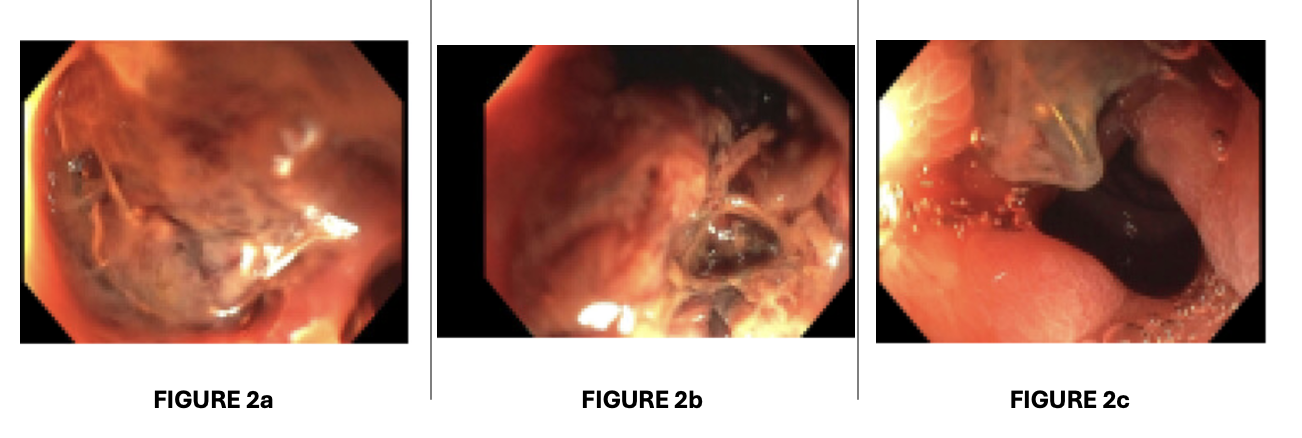
Figure: Figure 2a-c:
Endoscopy Images of an actively bleeding, large, partially obstructive ulcerated mass. Visibly irregular, nodular, fungating or infiltrative, consistent with malignancy.
Disclosures:
Ethan Abrishamian indicated no relevant financial relationships.
Niyaz Arif indicated no relevant financial relationships.
Prasad Rajalingamgari indicated no relevant financial relationships.
Justin Wagner indicated no relevant financial relationships.
Akil Olliverre indicated no relevant financial relationships.
Michael Bernstein indicated no relevant financial relationships.
Ethan Abrishamian, DO1, Niyaz Arif, MD1, Prasad Rajalingamgari, MD1, Justin Wagner, DO2, Akil Olliverre, MD3, Michael Bernstein, MD2. P6218 - Duodenal Metastasis From Nasopharyngeal Carcinoma: A Case Report of an Uncommon Metastatic Site, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals - - New York, NY, Roslyn Heights, NY; 2NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 3NYC Health + Hospitals/South Brooklyn Health, New York, NY
Introduction: Nasopharyngeal carcinoma (NPC) is a rare malignancy with variable metastatic patterns, most commonly to bone, lymph nodes, liver, and lungs (1). Gastrointestinal (GI) involvement is exceedingly rare; one report identified only five cases (2). We present a rare case of duodenal metastasis from NPC, highlighting an uncommon pattern of dissemination (3).
Case Description/
Methods: A 50-year-old Asian American male with stage IVb WHO type II NPC, diagnosed in 2014 with cerebral and hepatic metastases, presented with hypotension (83/53 mmHg), abdominal pain, coffee-ground emesis, and 30-lb weight loss over three months. Exam showed cachexia, jaundice, and epigastric tenderness.
Labs revealed marked hepatocellular injury (AST 6000 U/L, ALT 1700 U/L), cholestasis (ALP 500 U/L), hypoalbuminemia (2.0 g/dL), leukocytosis (27 × 10³/μL), anemia (6.7 g/dL), thrombocytopenia (116 × 10³/μL), and coagulopathy (INR 5.15). CT abdomen showed progression of hepatic metastases (Fig. 1). The patient was admitted to ICU, where he developed hematemesis requiring massive transfusion. EGD revealed a large, actively bleeding duodenal mass (Fig. 2). Despite aggressive resuscitation, the patient expired shortly after.
Discussion: NPC is rare globally but more common in East and Southeast Asia. WHO type II NPC is aggressive with a high rate of distant metastasis, though GI spread, especially to the duodenum, is extremely rare (4). In this case, the patient presented with hypotension, anemia, weight loss, and GI bleeding. Endoscopy showed an ulcerated, fungating, and partially obstructive duodenal mass. Though biopsy was precluded by bleeding risk, the endoscopic appearance and clinical history strongly supported duodenal metastasis.
Primary GI malignancies (e.g., adenocarcinoma, GIST, lymphoma) were considered but deemed unlikely due to lack of risk factors and close temporal association with systemic disease progression. Rare reports of duodenal metastases from NPC exist, often presenting with GI bleeding or obstruction (5,6). Autopsy studies also reveal small bowel involvement in advanced NPC (7).
This case underscores the importance of considering GI metastasis in NPC patients with GI symptoms and the diagnostic challenges when biopsy is not feasible.
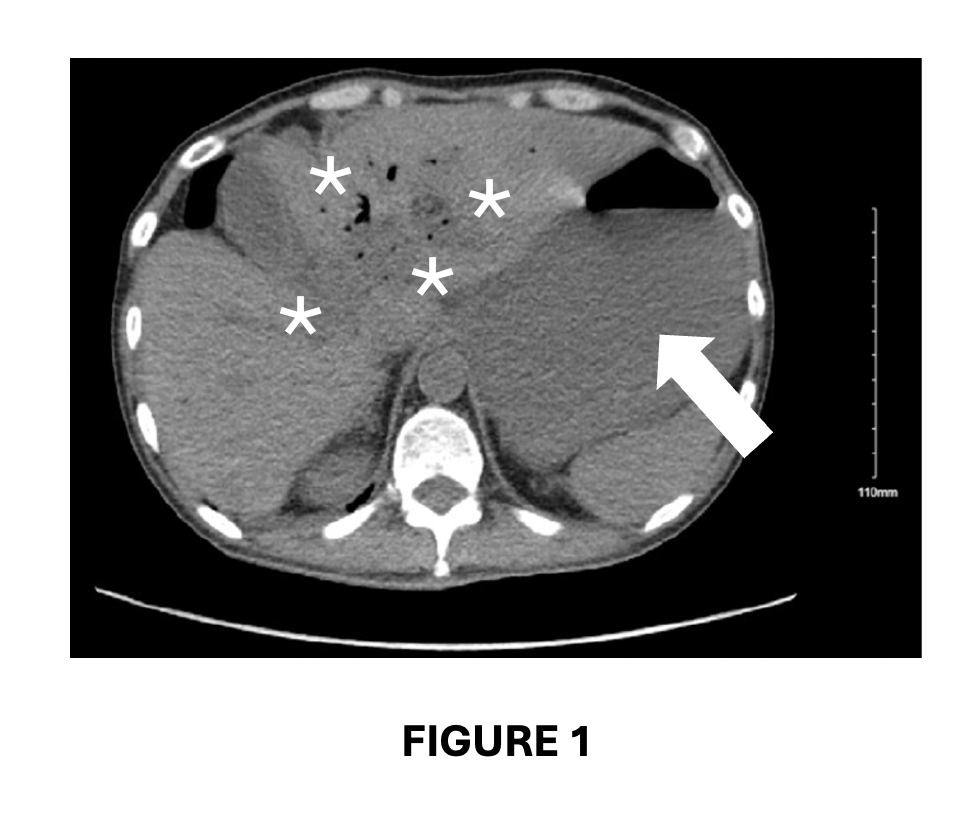
Figure: Figure 1:
Contrast-enhanced CT of the Abdomen and Pelvis.
Multiple hypodense, solid, round lesions are seen in the left hepatic lobe (indicated by asterisks), and a similar hypodense lesion is noted in the right hepatic lobe (indicated by the arrow). These findings are suspicious for hepatic metastatic disease.
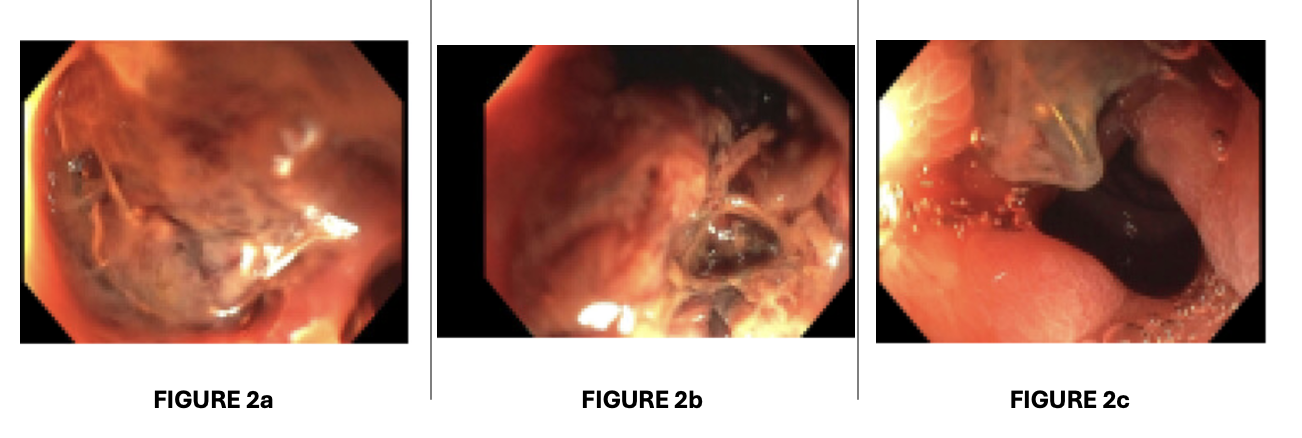
Figure: Figure 2a-c:
Endoscopy Images of an actively bleeding, large, partially obstructive ulcerated mass. Visibly irregular, nodular, fungating or infiltrative, consistent with malignancy.
Disclosures:
Ethan Abrishamian indicated no relevant financial relationships.
Niyaz Arif indicated no relevant financial relationships.
Prasad Rajalingamgari indicated no relevant financial relationships.
Justin Wagner indicated no relevant financial relationships.
Akil Olliverre indicated no relevant financial relationships.
Michael Bernstein indicated no relevant financial relationships.
Ethan Abrishamian, DO1, Niyaz Arif, MD1, Prasad Rajalingamgari, MD1, Justin Wagner, DO2, Akil Olliverre, MD3, Michael Bernstein, MD2. P6218 - Duodenal Metastasis From Nasopharyngeal Carcinoma: A Case Report of an Uncommon Metastatic Site, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
