Tuesday Poster Session
Category: Small Intestine
P6304 - Fatal Duodenal Hematoma Post-DAPT in STEMI: The Bleeding-Thrombosis Dilemma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amen I. Javaid, MD (she/her/hers)
INOVA Fairfax Hospital
Woodbridge, VA
Presenting Author(s)
Amen I. Javaid, MD
INOVA Fairfax Hospital, Woodbridge, VA
Introduction: Intramural duodenal hematomas are rare and typically occur in the setting of trauma, anticoagulation, or as a complication of endoscopic procedures. A spontaneous hematoma developing while on dual antiplatelet therapy has not been previously described. This case presents a life threatening challenge of how to manage antiplatelet therapy in a patient at risk for in stent thrombosis after recent coronary intervention, while also facing serious gastrointestinal bleeding.
Case Description/
Methods: A 62 year old man presented with hematemesis and abdominal pain one month after undergoing percutaneous coronary intervention (PCI) with drug eluting stent (DES) placement to the mid right coronary artery (RCA) for ST elevation myocardial infarction. At presentation, he was on DAPT with aspirin and ticagrelor. Initial abdominal CT showed asymmetric thickening of the distal stomach and proximal duodenum, consistent with an intramural hematoma. EGD revealed a 30 millimeter pedunculated and highly vascular polyp in the duodenum which was biopsied.
Within 72 hours, the patient developed hemodynamic instability. Repeat imaging showed progression of the hematoma causing gastric outlet obstruction, requiring nasogastric decompression. The cardiology team reviewed the thrombotic risk of stopping DAPT and assessed it to be relatively low given the location in the RCA rather then left anterior descending or left main coronary artery. Ticagrelor was held, and then restarted as monotherapy one week after the initial bleeding event. Unfortunately, follow up imaging revealed a contained perforation of the duodenum. The patient underwent emergency surgery which revealed feculent peritonitis and hemorrhagic cholecystitis. Despite multiple operations and supportive care, he developed multiorgan failure and passed away.
Discussion: This appears to be the first reported case of spontaneous intramural duodenal hematoma associated solely with DAPT. It highlights the need for careful clinical judgment in patients with gastrointestinal symptoms after recent coronary intervention. The case illustrates the high stakes of balancing bleeding and thrombosis risk, particularly when there is limited guidance from current recommendations. Timely multidisciplinary collaboration is essential in these complex scenarios, and further research is needed to guide the timing of antiplatelet resumption to minimize both stent thrombosis and major bleeding.
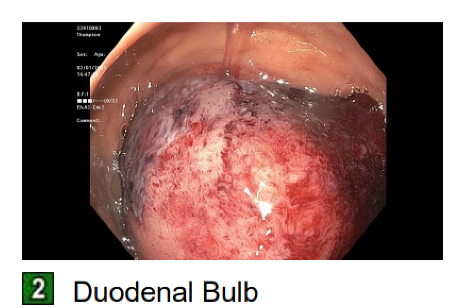
Figure: 30 mm duodenal polyp visualized on EGD
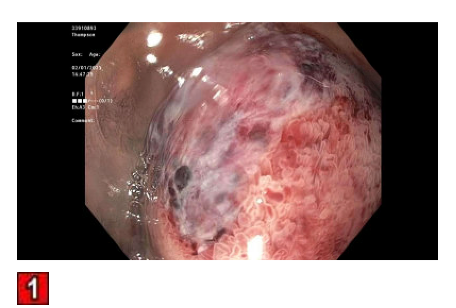
Figure: 30 mm duodenal polyp visualized on EGD
Disclosures:
Amen Javaid indicated no relevant financial relationships.
Amen I. Javaid, MD. P6304 - Fatal Duodenal Hematoma Post-DAPT in STEMI: The Bleeding-Thrombosis Dilemma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
INOVA Fairfax Hospital, Woodbridge, VA
Introduction: Intramural duodenal hematomas are rare and typically occur in the setting of trauma, anticoagulation, or as a complication of endoscopic procedures. A spontaneous hematoma developing while on dual antiplatelet therapy has not been previously described. This case presents a life threatening challenge of how to manage antiplatelet therapy in a patient at risk for in stent thrombosis after recent coronary intervention, while also facing serious gastrointestinal bleeding.
Case Description/
Methods: A 62 year old man presented with hematemesis and abdominal pain one month after undergoing percutaneous coronary intervention (PCI) with drug eluting stent (DES) placement to the mid right coronary artery (RCA) for ST elevation myocardial infarction. At presentation, he was on DAPT with aspirin and ticagrelor. Initial abdominal CT showed asymmetric thickening of the distal stomach and proximal duodenum, consistent with an intramural hematoma. EGD revealed a 30 millimeter pedunculated and highly vascular polyp in the duodenum which was biopsied.
Within 72 hours, the patient developed hemodynamic instability. Repeat imaging showed progression of the hematoma causing gastric outlet obstruction, requiring nasogastric decompression. The cardiology team reviewed the thrombotic risk of stopping DAPT and assessed it to be relatively low given the location in the RCA rather then left anterior descending or left main coronary artery. Ticagrelor was held, and then restarted as monotherapy one week after the initial bleeding event. Unfortunately, follow up imaging revealed a contained perforation of the duodenum. The patient underwent emergency surgery which revealed feculent peritonitis and hemorrhagic cholecystitis. Despite multiple operations and supportive care, he developed multiorgan failure and passed away.
Discussion: This appears to be the first reported case of spontaneous intramural duodenal hematoma associated solely with DAPT. It highlights the need for careful clinical judgment in patients with gastrointestinal symptoms after recent coronary intervention. The case illustrates the high stakes of balancing bleeding and thrombosis risk, particularly when there is limited guidance from current recommendations. Timely multidisciplinary collaboration is essential in these complex scenarios, and further research is needed to guide the timing of antiplatelet resumption to minimize both stent thrombosis and major bleeding.
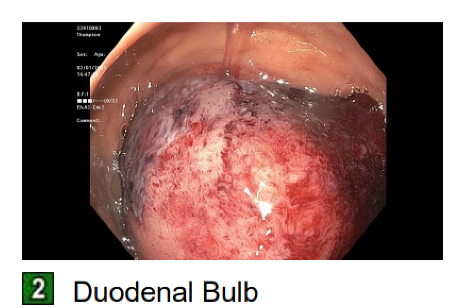
Figure: 30 mm duodenal polyp visualized on EGD
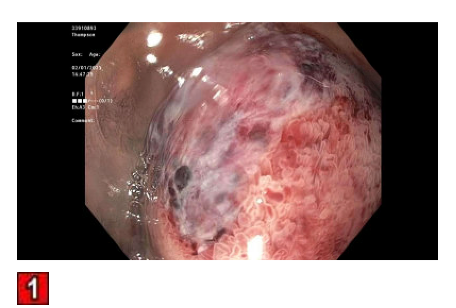
Figure: 30 mm duodenal polyp visualized on EGD
Disclosures:
Amen Javaid indicated no relevant financial relationships.
Amen I. Javaid, MD. P6304 - Fatal Duodenal Hematoma Post-DAPT in STEMI: The Bleeding-Thrombosis Dilemma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

