Tuesday Poster Session
Category: Small Intestine
P6297 - Unmasking the Silent Culprit: Olmesartan-Induced Gastroenteropathy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nina Quirk, MD, MS
University of Texas Health Sciences Center in Houston
Houston, TX
Presenting Author(s)
Nina Quirk, MD, MS1, Priscila Olague, MD2, Sruthi Subramanian, MD1, Suhair Al-Salihi, MD3, Erin Rubin, MD4, Andrew Dupont, MD1
1University of Texas Health Sciences Center in Houston, Houston, TX; 2Univeristy of Texas Health Sciences Center in Houston, Houston, TX; 3University of Texas Health Science Center Houston, Houston, TX; 4McGovern Medical School at UTHealth Houston, Houston, TX
Introduction: Olmesartan has been associated with the development of a unique seronegative celiac-like enteropathy called olmesartan-induced enteropathy (OIE). This rare condition can manifest with chronic diarrhea and abdominal pain which may be misdiagnosed as irritable bowel syndrome. Diagnosing OIE is challenging, necessitating a process of exclusion as histopathological examination of biopsied tissue is similar to celiac disease. We present a case of a patient on long-term olmesartan who developed chronic diarrhea and significant weight loss requiring multiple hospitalizations.
Case Description/
Methods: A 47-year-old female presented to the clinic with chronic diarrhea for 4 months with recent worsening nausea, vomiting, abdominal pain, decreased oral intake, and weight loss. Her home medications included olmesartan 40 mg, which she had been taking for more than ten years for hypertension. She was hospitalized a week prior and underwent negative stool studies for C. difficile, CT of the abdomen and pelvis was unremarkable, and sigmoidoscopy with random biopsies was normal. Fecal calprotectin was 608. She was empirically treated with metronidazole without improvement and subsequently discharged off olmesartan with improvement of diarrhea. After discharge, she became hypertensive and olmesartan was restarted. She was seen in GI clinic one month later with severe diarrhea, dehydration, 25-pound weight loss, and was admitted to the hospital with hypotension. Olmesartan was stopped; MR enterography was unrevealing; infectious stool studies were negative and celiac serologies were negative. EGD and colonoscopy revealed diffuse gastric erythema and normal appearing small bowel. Colonoscopy was unremarkable. Biopsies revealed total villous blunting in the duodenum and ileum and diffuse active chronic gastritis (Images 1a-3c). Given the severity of the disease, she was prescribed a prednisone taper and olmesartan was discontinued due to strong suspicion of OIE. At a follow-up clinic visit, the patient reported significant improvement in her symptoms.
Discussion: Our case report presents a patient with a history of chronic olmesartan use who developed persistent diarrhea after more than 10 years of treatment. This case underscores the importance of recognizing medication-induced enteropathies in patients exhibiting celiac-like features, allowing for early detection and optimal management, even in cases with extended exposure to susceptible medications.
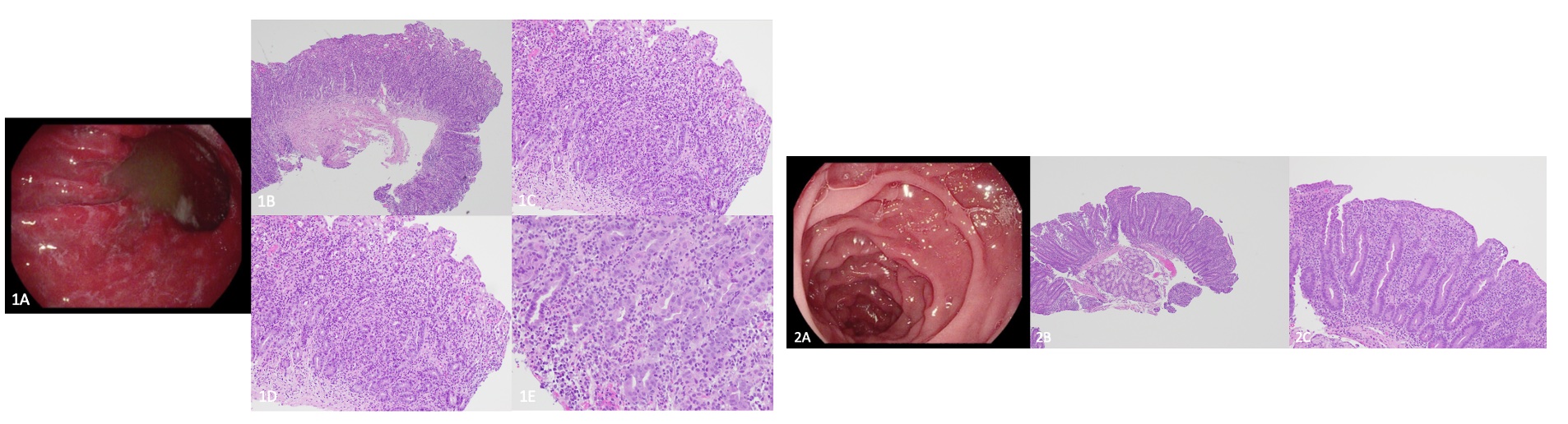
Figure: 1a. Stomach antrum erosion on EGD. 1b. Stomach antrum, H&E stain, 4x objective. Eroded gastric antral mucosa with moderately active chronic gastritis and bacterial overgrowth. 1c. Stomach antrum, H&E stain, 10x objective. Loss of the foveolar surface epithelium with regenerative atypia is indicative of an erosion. Mixed lamina propria inflammation is present with a predominantly lymphocytic inflammatory infiltrate. 1d. Stomach body/fundus H&E stain, 10x objective. The gastric body fundic mucosa is eroded with moderately active chronic gastritis. 1e. Stomach body/fundus H&E stain, 20x objective. There is attenuation of the surface epithelium with expansion of the lamina propria with mixed inflammation and regenerative atypia. Lamina propria as evident by presence of neutrophils, eosinophils, and plasma cells. Inflammation is seen. 2a. Second part of duodenum. 2b. Duodenum H&E stain, 4x objective. Eroded duodenal mucosa with total villous blunting. 2c. Duodenum H&E stain, 10x objective H&E stain. Eroded duodenal mucosa with villous blunting and loss of goblet cells.
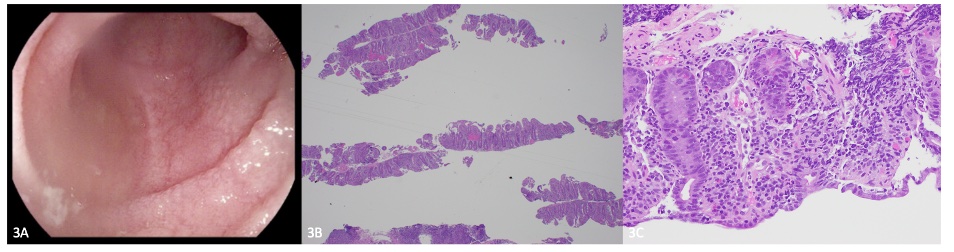
Figure: 3a. Terminal ileum. 3b. Ileum, H&E stain, 2x objective. Eroded ileal mucosa with total villous blunting. 3c. Ileum, H&E stain, 20x objective. Eroded ileal mucosa with villous blunting and diffuse expansion of lamina propria with chronic inflammatory infiltrate. There is moderate activity with neutrophilic cryptitis.
Disclosures:
Nina Quirk indicated no relevant financial relationships.
Priscila Olague indicated no relevant financial relationships.
Sruthi Subramanian indicated no relevant financial relationships.
Suhair Al-Salihi indicated no relevant financial relationships.
Erin Rubin indicated no relevant financial relationships.
Andrew Dupont indicated no relevant financial relationships.
Nina Quirk, MD, MS1, Priscila Olague, MD2, Sruthi Subramanian, MD1, Suhair Al-Salihi, MD3, Erin Rubin, MD4, Andrew Dupont, MD1. P6297 - Unmasking the Silent Culprit: Olmesartan-Induced Gastroenteropathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health Sciences Center in Houston, Houston, TX; 2Univeristy of Texas Health Sciences Center in Houston, Houston, TX; 3University of Texas Health Science Center Houston, Houston, TX; 4McGovern Medical School at UTHealth Houston, Houston, TX
Introduction: Olmesartan has been associated with the development of a unique seronegative celiac-like enteropathy called olmesartan-induced enteropathy (OIE). This rare condition can manifest with chronic diarrhea and abdominal pain which may be misdiagnosed as irritable bowel syndrome. Diagnosing OIE is challenging, necessitating a process of exclusion as histopathological examination of biopsied tissue is similar to celiac disease. We present a case of a patient on long-term olmesartan who developed chronic diarrhea and significant weight loss requiring multiple hospitalizations.
Case Description/
Methods: A 47-year-old female presented to the clinic with chronic diarrhea for 4 months with recent worsening nausea, vomiting, abdominal pain, decreased oral intake, and weight loss. Her home medications included olmesartan 40 mg, which she had been taking for more than ten years for hypertension. She was hospitalized a week prior and underwent negative stool studies for C. difficile, CT of the abdomen and pelvis was unremarkable, and sigmoidoscopy with random biopsies was normal. Fecal calprotectin was 608. She was empirically treated with metronidazole without improvement and subsequently discharged off olmesartan with improvement of diarrhea. After discharge, she became hypertensive and olmesartan was restarted. She was seen in GI clinic one month later with severe diarrhea, dehydration, 25-pound weight loss, and was admitted to the hospital with hypotension. Olmesartan was stopped; MR enterography was unrevealing; infectious stool studies were negative and celiac serologies were negative. EGD and colonoscopy revealed diffuse gastric erythema and normal appearing small bowel. Colonoscopy was unremarkable. Biopsies revealed total villous blunting in the duodenum and ileum and diffuse active chronic gastritis (Images 1a-3c). Given the severity of the disease, she was prescribed a prednisone taper and olmesartan was discontinued due to strong suspicion of OIE. At a follow-up clinic visit, the patient reported significant improvement in her symptoms.
Discussion: Our case report presents a patient with a history of chronic olmesartan use who developed persistent diarrhea after more than 10 years of treatment. This case underscores the importance of recognizing medication-induced enteropathies in patients exhibiting celiac-like features, allowing for early detection and optimal management, even in cases with extended exposure to susceptible medications.
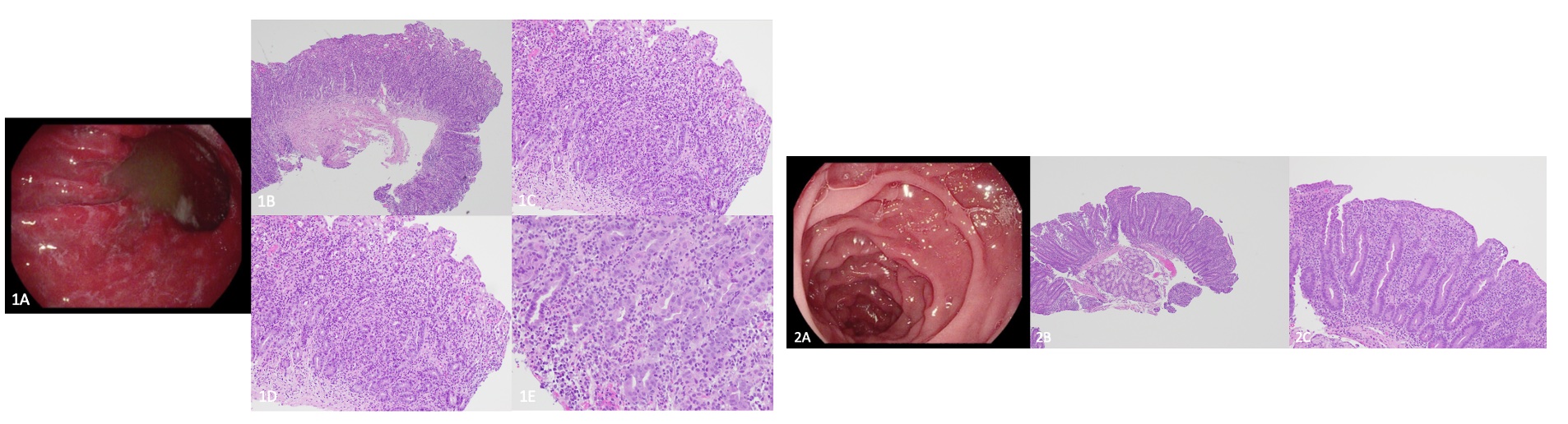
Figure: 1a. Stomach antrum erosion on EGD. 1b. Stomach antrum, H&E stain, 4x objective. Eroded gastric antral mucosa with moderately active chronic gastritis and bacterial overgrowth. 1c. Stomach antrum, H&E stain, 10x objective. Loss of the foveolar surface epithelium with regenerative atypia is indicative of an erosion. Mixed lamina propria inflammation is present with a predominantly lymphocytic inflammatory infiltrate. 1d. Stomach body/fundus H&E stain, 10x objective. The gastric body fundic mucosa is eroded with moderately active chronic gastritis. 1e. Stomach body/fundus H&E stain, 20x objective. There is attenuation of the surface epithelium with expansion of the lamina propria with mixed inflammation and regenerative atypia. Lamina propria as evident by presence of neutrophils, eosinophils, and plasma cells. Inflammation is seen. 2a. Second part of duodenum. 2b. Duodenum H&E stain, 4x objective. Eroded duodenal mucosa with total villous blunting. 2c. Duodenum H&E stain, 10x objective H&E stain. Eroded duodenal mucosa with villous blunting and loss of goblet cells.
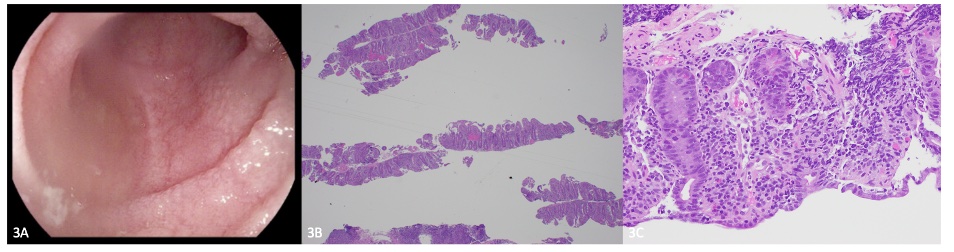
Figure: 3a. Terminal ileum. 3b. Ileum, H&E stain, 2x objective. Eroded ileal mucosa with total villous blunting. 3c. Ileum, H&E stain, 20x objective. Eroded ileal mucosa with villous blunting and diffuse expansion of lamina propria with chronic inflammatory infiltrate. There is moderate activity with neutrophilic cryptitis.
Disclosures:
Nina Quirk indicated no relevant financial relationships.
Priscila Olague indicated no relevant financial relationships.
Sruthi Subramanian indicated no relevant financial relationships.
Suhair Al-Salihi indicated no relevant financial relationships.
Erin Rubin indicated no relevant financial relationships.
Andrew Dupont indicated no relevant financial relationships.
Nina Quirk, MD, MS1, Priscila Olague, MD2, Sruthi Subramanian, MD1, Suhair Al-Salihi, MD3, Erin Rubin, MD4, Andrew Dupont, MD1. P6297 - Unmasking the Silent Culprit: Olmesartan-Induced Gastroenteropathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
