Tuesday Poster Session
Category: Stomach and Spleen
P6383 - Diagnostic Challenges in Chylous Ascites: A Case Report of Suspected Lymphatic Obstruction Following Distal Gastrectomy and Vagotomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Shayan Ravanassa, BS
University of Texas Medical Branch, John Sealy School of Medicine
Galveston, TX
Presenting Author(s)
Shayan Ravanassa, BS1, Reema Patel, MD2, Raakhi Menon, DO2, Keegan Colletier, MD2, Sreeram Parupudi, MD2
1University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Chylous ascites (CA) is a rare condition characterized by triglyceride-rich, milky peritoneal fluid. It can arise from trauma, malignancies, infections, or abdominal surgery complications, leading to chronic leakage, immune suppression, and malnutrition. With a mortality rate of 40 to 70%, early diagnosis and treatment are vital. This case discusses a patient with newly diagnosed CA, with at least a two-year delay in diagnosis following his initial presentation.
Case Description/
Methods: We present the case of a 61-year-old male with a history of lymphedema, alcohol use disorder, and perforated peptic ulcer disease repaired by distal gastrectomy and vagotomy in 2013 who presented with worsening dyspnea, bilateral lower extremity edema, and ascites. Previously managed with paracentesis and diuretics for presumed alcohol-related cirrhosis, his condition progressed to monthly taps despite therapy, developing severe lymphedema, scrotal swelling, and ascites. Lab findings showed chronic hypoalbuminemia, hypocalcemia, and a MELD-3.0 score of 11. Abdominal ultrasound revealed large-volume ascites and a possible micronodular liver contour. Ascitic fluid analysis (serum-albumin ascites gradient < 0.5, protein levels < 1.0 g/dL) excluded portal hypertension or cardiac disease.
Subsequent paracentesis revealed 4 liters of milky fluid (triglycerides > 1,050 mg/dL). Follow-up IR-lymphangiography revealed dilated lymphatic channels, but no apparent leak. He was discharged on an optimized diuretic and nutritional regimen, with instructions for outpatient follow-up to undergo MR lymphangiography to evaluate for lymphatic disruption and identify potential areas for therapeutic intervention.
Discussion: CA is a rare accumulation of triglyceride-rich peritoneal fluid, often due to malignancy, cirrhosis, or infections. In our patient, asymmetric lymphedema following distal gastrectomy and vagotomy, along with fatty ascites, suggests postoperative lymphatic obstruction, an underrecognized cause of CA. Early diagnostic paracentesis (e.g., triglycerides > 220 mg/dL) is crucial to prevent malnutrition and immunodeficiency. Computerized tomography may reveal ductal injury, while lymphangiography localizes leaks for intervention. Prognosis varies by etiology, with high mortality if surgical or oncologic interventions aren’t feasible. Further MR lymphangiography or lymphoscintigraphy, carcinoembryonic antigen tests, and infectious workup are necessary to exclude malignancy or infection and strategize treatment.
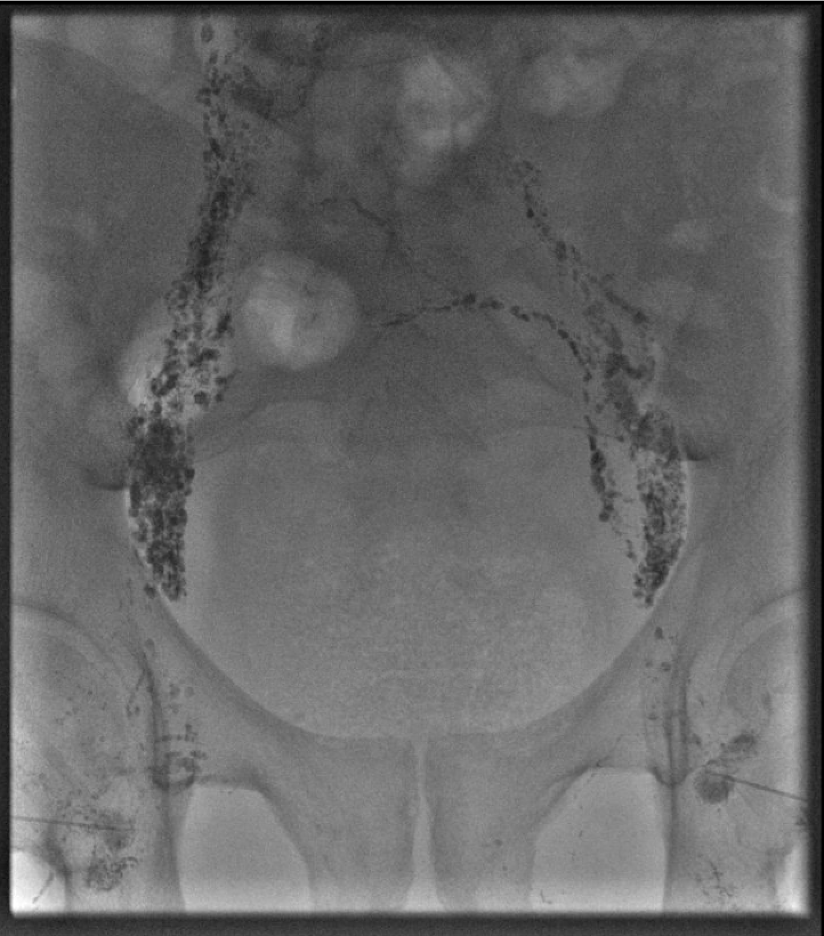
Figure: Photographs demonstrating lymphedema and hyperkeratosis of the right upper extremity, right lower extremity, and left lower extremity, respectively.

Figure: Ultrasound and fluoroscopy-guided lymphangiogram demonstrating ectatic lymphatic channels.
Disclosures:
Shayan Ravanassa indicated no relevant financial relationships.
Reema Patel indicated no relevant financial relationships.
Raakhi Menon indicated no relevant financial relationships.
Keegan Colletier indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Shayan Ravanassa, BS1, Reema Patel, MD2, Raakhi Menon, DO2, Keegan Colletier, MD2, Sreeram Parupudi, MD2. P6383 - Diagnostic Challenges in Chylous Ascites: A Case Report of Suspected Lymphatic Obstruction Following Distal Gastrectomy and Vagotomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX; 2University of Texas Medical Branch, Galveston, TX
Introduction: Chylous ascites (CA) is a rare condition characterized by triglyceride-rich, milky peritoneal fluid. It can arise from trauma, malignancies, infections, or abdominal surgery complications, leading to chronic leakage, immune suppression, and malnutrition. With a mortality rate of 40 to 70%, early diagnosis and treatment are vital. This case discusses a patient with newly diagnosed CA, with at least a two-year delay in diagnosis following his initial presentation.
Case Description/
Methods: We present the case of a 61-year-old male with a history of lymphedema, alcohol use disorder, and perforated peptic ulcer disease repaired by distal gastrectomy and vagotomy in 2013 who presented with worsening dyspnea, bilateral lower extremity edema, and ascites. Previously managed with paracentesis and diuretics for presumed alcohol-related cirrhosis, his condition progressed to monthly taps despite therapy, developing severe lymphedema, scrotal swelling, and ascites. Lab findings showed chronic hypoalbuminemia, hypocalcemia, and a MELD-3.0 score of 11. Abdominal ultrasound revealed large-volume ascites and a possible micronodular liver contour. Ascitic fluid analysis (serum-albumin ascites gradient < 0.5, protein levels < 1.0 g/dL) excluded portal hypertension or cardiac disease.
Subsequent paracentesis revealed 4 liters of milky fluid (triglycerides > 1,050 mg/dL). Follow-up IR-lymphangiography revealed dilated lymphatic channels, but no apparent leak. He was discharged on an optimized diuretic and nutritional regimen, with instructions for outpatient follow-up to undergo MR lymphangiography to evaluate for lymphatic disruption and identify potential areas for therapeutic intervention.
Discussion: CA is a rare accumulation of triglyceride-rich peritoneal fluid, often due to malignancy, cirrhosis, or infections. In our patient, asymmetric lymphedema following distal gastrectomy and vagotomy, along with fatty ascites, suggests postoperative lymphatic obstruction, an underrecognized cause of CA. Early diagnostic paracentesis (e.g., triglycerides > 220 mg/dL) is crucial to prevent malnutrition and immunodeficiency. Computerized tomography may reveal ductal injury, while lymphangiography localizes leaks for intervention. Prognosis varies by etiology, with high mortality if surgical or oncologic interventions aren’t feasible. Further MR lymphangiography or lymphoscintigraphy, carcinoembryonic antigen tests, and infectious workup are necessary to exclude malignancy or infection and strategize treatment.
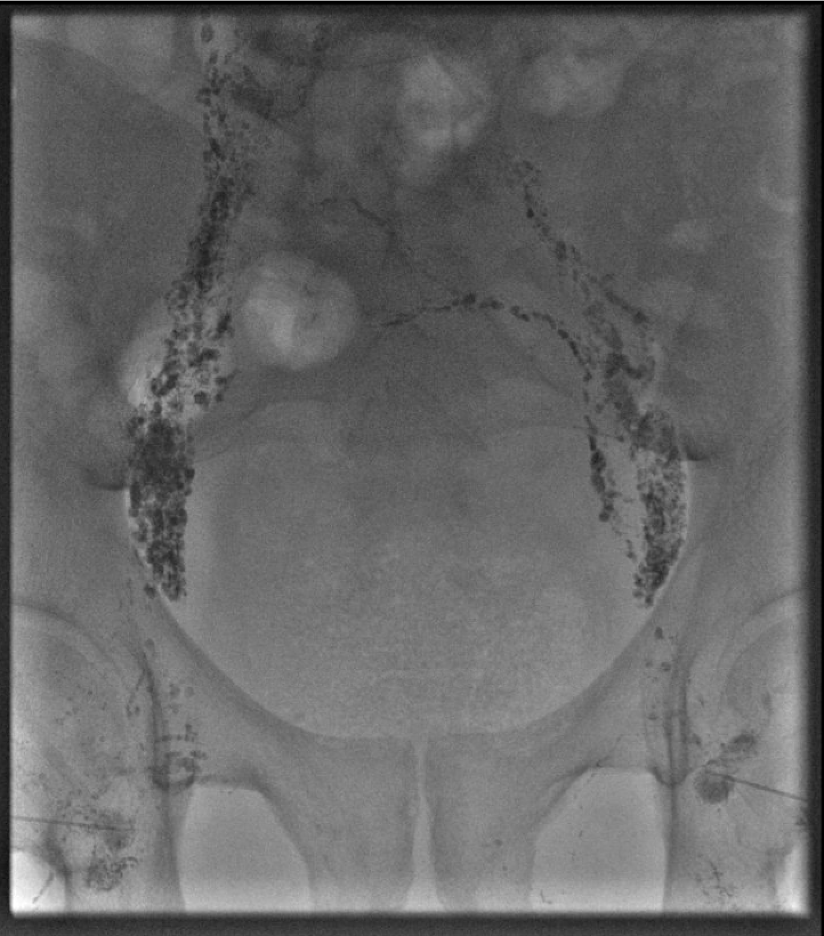
Figure: Photographs demonstrating lymphedema and hyperkeratosis of the right upper extremity, right lower extremity, and left lower extremity, respectively.

Figure: Ultrasound and fluoroscopy-guided lymphangiogram demonstrating ectatic lymphatic channels.
Disclosures:
Shayan Ravanassa indicated no relevant financial relationships.
Reema Patel indicated no relevant financial relationships.
Raakhi Menon indicated no relevant financial relationships.
Keegan Colletier indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Shayan Ravanassa, BS1, Reema Patel, MD2, Raakhi Menon, DO2, Keegan Colletier, MD2, Sreeram Parupudi, MD2. P6383 - Diagnostic Challenges in Chylous Ascites: A Case Report of Suspected Lymphatic Obstruction Following Distal Gastrectomy and Vagotomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

