Tuesday Poster Session
Category: Stomach and Spleen
P6369 - More Than a Gut Feeling: Uncovering ICI Gastritis in the Outpatient Setting
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Rammy Bashir, MD, MSc
Norwalk Hospital/Yale University
Norwalk, CT
Presenting Author(s)
Rammy Bashir, MD, MSc1, Ana Finke Abbott, MD1, Zablon Sewalem, MD, MSc1, Jenny Joseph, MBBS1, Mohammed Al-Aquily, MD1, Triston Berger, MD2, Rakhee N. Mangla, MD1
1Norwalk Hospital/Yale University, Norwalk, CT; 2Norwalk Hospital, Norwalk, CT
Introduction: Immune checkpoint inhibitors (ICIs) have transformed the treatment of advanced malignancies but also introduced unique complications. Immune-related adverse events (irAEs) from ICIs can affect any part of the gastrointestinal (GI) tract, with upper GI toxicities often underrecognized. ICI-associated gastritis is rare, with an incidence estimated at 0.35%–1.46%. It typically presents with nonspecific symptoms such as nausea, vomiting, or abdominal pain. The lack of specific grading systems or guidelines further complicates diagnosis and management. We present a case of ICI gastritis diagnosed in the outpatient setting.
Case Description/
Methods: A 69-year-old woman with metastatic lung adenocarcinoma presented with progressive nausea, vomiting, and intermittent diarrhea. She had initiated ipilimumab/nivolumab five months earlier following progression on multiple prior therapies, including pembrolizumab. Symptoms persisted despite antiemetics and acid-reducing therapy. Imaging, labs, and infectious stool workup were unremarkable, but fecal calprotectin was markedly elevated at 2980. Due to persistent symptoms, upper endoscopy was performed, revealing diffuse gastric mucosal congestion and thick mucoid exudate. Biopsies showed chronic active gastritis with lymphoplasmacytic and neutrophilic infiltrates, neutrophilic gland abscesses, and intraepithelial lymphocytosis. Given her ICI exposure, these findings were consistent with ICI-related gastric injury. ICIs were discontinued, and corticosteroids were initiated. A flexible sigmoidoscopy performed for ongoing diarrhea revealed mild mucosal congestion but normal histology. This was likely influenced by concurrent steroid use, which may have masked underlying ICI colitis. She was subsequently transitioned to docetaxel with complete resolution of GI symptoms.
Discussion: ICI-induced gastritis remains a diagnostic challenge in the outpatient setting, as early symptoms mimic chemotherapy side effects or functional dyspepsia. Although less common than ICI colitis, upper GI irAEs can be equally severe. In one study, 70% of patients with biopsy-proven ICI gastritis had concurrent colitis. This case highlights the importance of endoscopic evaluation and biopsy, and underscores the need for validated, ICI gastritis-specific grading tools and management algorithms as combination immunotherapy becomes more widely used.

Figure: Diffuse, severely congested and hyperemic mucosa, covered with a thick mucoid exudate that was lavaged and aspirated, was observed throughout the examined stomach.
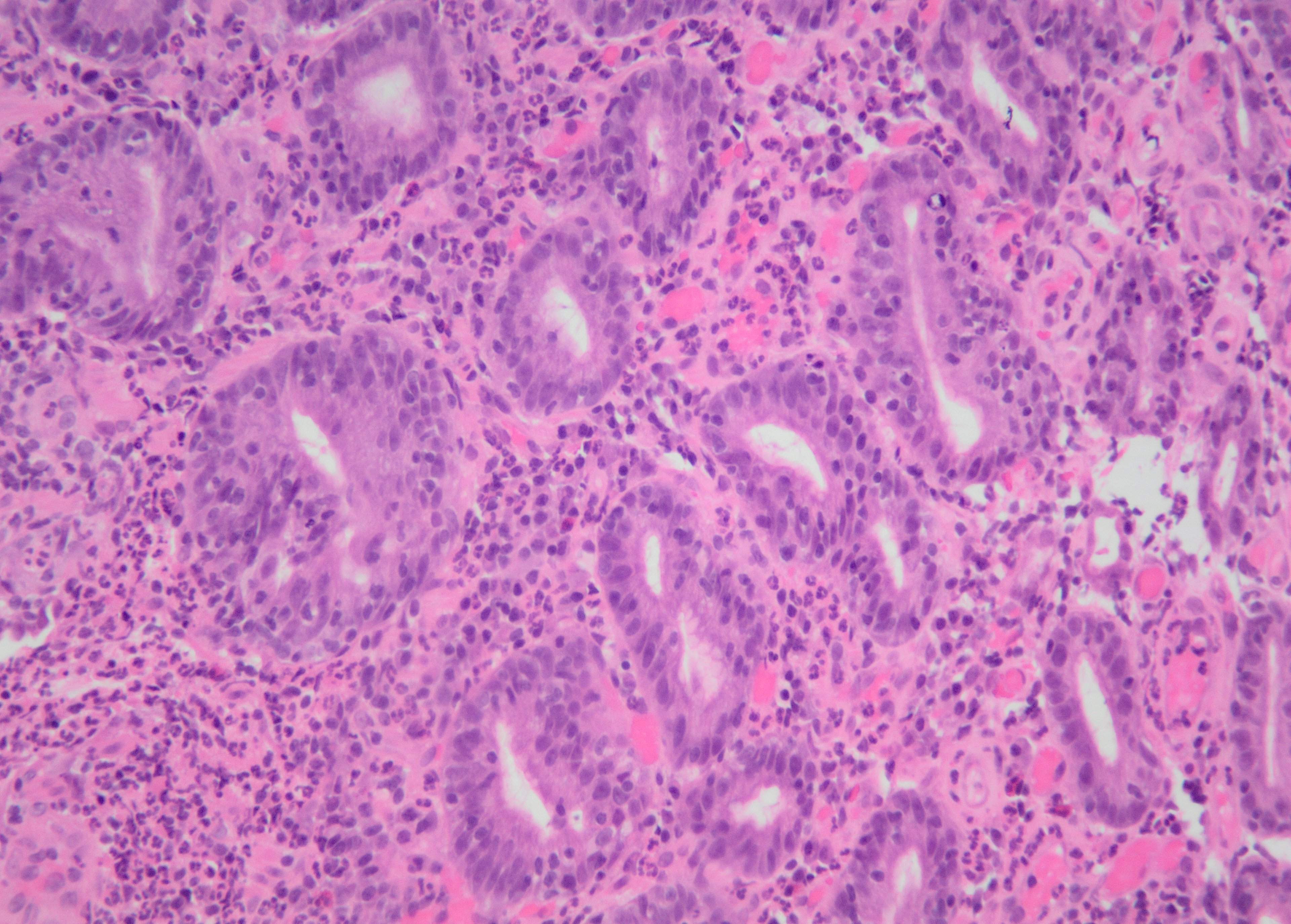
Figure: Neutrophils, identifiable by their multilobed nuclei and pink cytoplasm, are seen infiltrating the epithelium. Intraepithelial lymphocytosis is evident as small dark round lymphocytes embedded between epithelial cells. No organisms consistent with Helicobacter pylori are seen.
Disclosures:
Rammy Bashir indicated no relevant financial relationships.
Ana Finke Abbott indicated no relevant financial relationships.
Zablon Sewalem indicated no relevant financial relationships.
Jenny Joseph indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Rakhee Mangla indicated no relevant financial relationships.
Rammy Bashir, MD, MSc1, Ana Finke Abbott, MD1, Zablon Sewalem, MD, MSc1, Jenny Joseph, MBBS1, Mohammed Al-Aquily, MD1, Triston Berger, MD2, Rakhee N. Mangla, MD1. P6369 - More Than a Gut Feeling: Uncovering ICI Gastritis in the Outpatient Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Norwalk Hospital/Yale University, Norwalk, CT; 2Norwalk Hospital, Norwalk, CT
Introduction: Immune checkpoint inhibitors (ICIs) have transformed the treatment of advanced malignancies but also introduced unique complications. Immune-related adverse events (irAEs) from ICIs can affect any part of the gastrointestinal (GI) tract, with upper GI toxicities often underrecognized. ICI-associated gastritis is rare, with an incidence estimated at 0.35%–1.46%. It typically presents with nonspecific symptoms such as nausea, vomiting, or abdominal pain. The lack of specific grading systems or guidelines further complicates diagnosis and management. We present a case of ICI gastritis diagnosed in the outpatient setting.
Case Description/
Methods: A 69-year-old woman with metastatic lung adenocarcinoma presented with progressive nausea, vomiting, and intermittent diarrhea. She had initiated ipilimumab/nivolumab five months earlier following progression on multiple prior therapies, including pembrolizumab. Symptoms persisted despite antiemetics and acid-reducing therapy. Imaging, labs, and infectious stool workup were unremarkable, but fecal calprotectin was markedly elevated at 2980. Due to persistent symptoms, upper endoscopy was performed, revealing diffuse gastric mucosal congestion and thick mucoid exudate. Biopsies showed chronic active gastritis with lymphoplasmacytic and neutrophilic infiltrates, neutrophilic gland abscesses, and intraepithelial lymphocytosis. Given her ICI exposure, these findings were consistent with ICI-related gastric injury. ICIs were discontinued, and corticosteroids were initiated. A flexible sigmoidoscopy performed for ongoing diarrhea revealed mild mucosal congestion but normal histology. This was likely influenced by concurrent steroid use, which may have masked underlying ICI colitis. She was subsequently transitioned to docetaxel with complete resolution of GI symptoms.
Discussion: ICI-induced gastritis remains a diagnostic challenge in the outpatient setting, as early symptoms mimic chemotherapy side effects or functional dyspepsia. Although less common than ICI colitis, upper GI irAEs can be equally severe. In one study, 70% of patients with biopsy-proven ICI gastritis had concurrent colitis. This case highlights the importance of endoscopic evaluation and biopsy, and underscores the need for validated, ICI gastritis-specific grading tools and management algorithms as combination immunotherapy becomes more widely used.

Figure: Diffuse, severely congested and hyperemic mucosa, covered with a thick mucoid exudate that was lavaged and aspirated, was observed throughout the examined stomach.
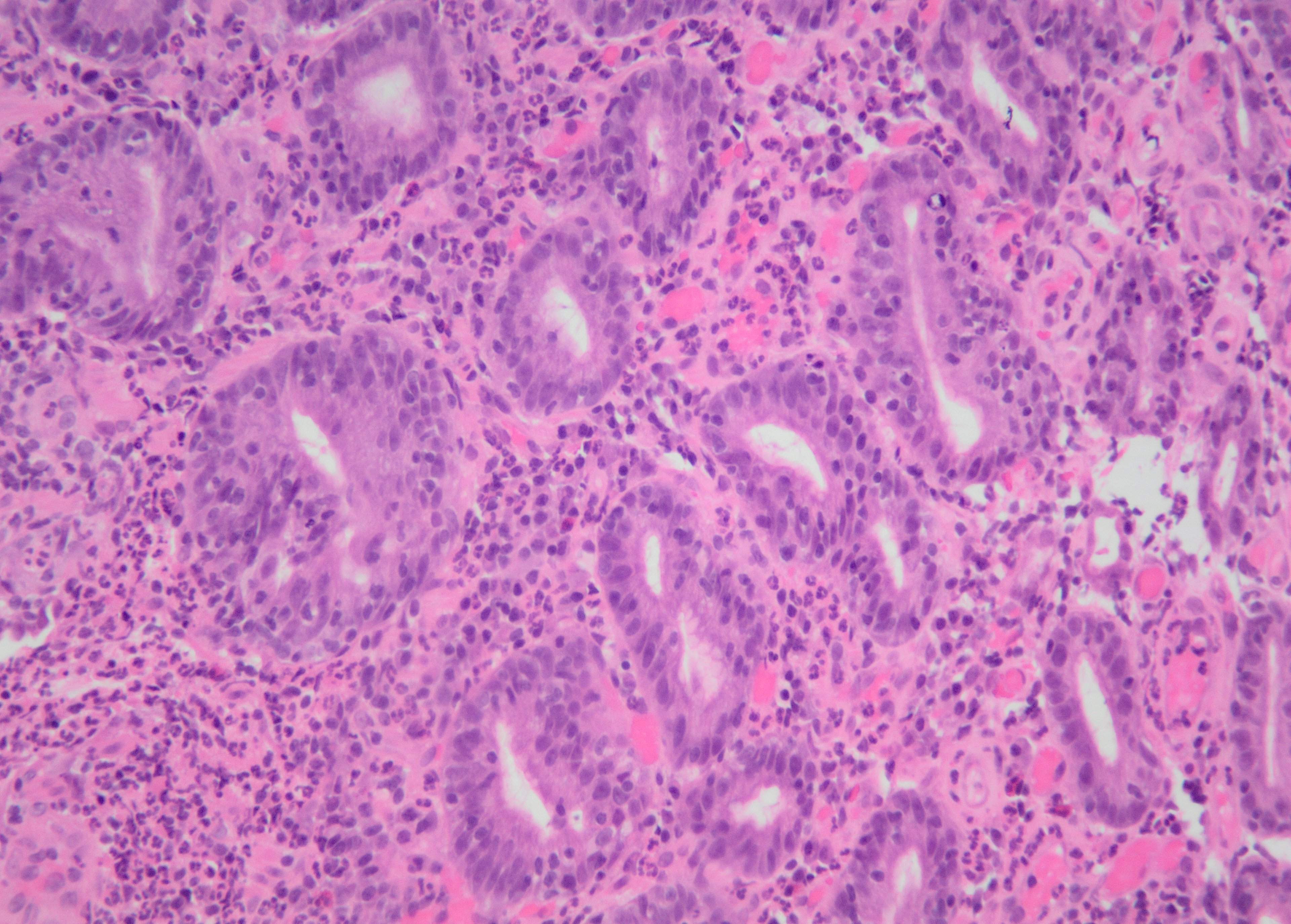
Figure: Neutrophils, identifiable by their multilobed nuclei and pink cytoplasm, are seen infiltrating the epithelium. Intraepithelial lymphocytosis is evident as small dark round lymphocytes embedded between epithelial cells. No organisms consistent with Helicobacter pylori are seen.
Disclosures:
Rammy Bashir indicated no relevant financial relationships.
Ana Finke Abbott indicated no relevant financial relationships.
Zablon Sewalem indicated no relevant financial relationships.
Jenny Joseph indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Rakhee Mangla indicated no relevant financial relationships.
Rammy Bashir, MD, MSc1, Ana Finke Abbott, MD1, Zablon Sewalem, MD, MSc1, Jenny Joseph, MBBS1, Mohammed Al-Aquily, MD1, Triston Berger, MD2, Rakhee N. Mangla, MD1. P6369 - More Than a Gut Feeling: Uncovering ICI Gastritis in the Outpatient Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
