Tuesday Poster Session
Category: Stomach and Spleen
P6408 - Through-the-Scope Suturing for Full-Thickness Perforation Closure - A Case Series
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fernanda Pessorrusso, MD, PhD (she/her/hers)
University of Colorado Anschutz Medical Campus
Erie, CO
Presenting Author(s)
Fernanda Pessorrusso, MD, PhD1, Paul Menard-Katcher, Md2, Mohammad Bilal, MD, FACG3, Thomas Enke, MD4
1University of Colorado Anschutz Medical Campus, Erie, CO; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Denver, CO; 4University of Colorado, Aurora, CO
Introduction: Gastrointestinal perforation after endoscopic procedures is a serious adverse event that can be managed endoscopically using through-the-scope (TTS) clips, over-the-scope clips and over-the-scope suturing. The use of TTS suturing with the helix tack system, allows for immediate defect closure without the need to withdraw and reload the endoscope, however, its use has primarily been described for mucosal closure post endoscopic resection. We describe two cases of full-thickness perforation that were successfully managed with TTS suturing (TTSS) device.
Case Description/
Methods: Case 1:
A 78 year old male with Lynch syndrome and prior small bowel adenocarcinoma was recently diagnosed with gastric adenocarcinoma. Staging endoscopic ultrasound (EUS) was performed and a 4 cm lesion was seen at the incisura and EUS was unable to differentiate between T1 versus T2 disease. After multidisciplinary discussion, patient was deemed a non-surgical candidate and referred for endoscopic submucosal dissection (ESD). ESD was performed and intense submucosal fibrosis raised concerns for muscular invasion. Endoscopic intra-muscular dissection was performed. Post-resection, a 1 cm area of full-thickness perforation was noted within a 5 cm resection bed. Attempts to close it with endoclips failed. A TTSS system was used and total of 5 systems were used (each set of tacks applied in Z configuration) for closure of the complete defect (Figure 1). No leak was seen on post-procedure upper gastrointestinal (UGI) series. Patient was discharged home after observation.
Case 2: An 84 year old woman with history of esophageal squamous cell carcinoma treated withchemoradiation complicated by an esophageal stricture refractory to endoscopic dilations underwent placement of a fully covered esophageal stent. Five days after the stent placement, the patient experienced chest pain and intolerance to oral intake. Upper endoscopy was performed for evaluation. Upon stent removal, a large full-thickness perforation was discovered in the gastric cardia measuring 5 cm in length. The defect was closed using a TTSS system utilizing a total of 5 systems (each set of tacks applied in Z configuration) (Figure 2). Follow-up UGI series showed no residual leak. Patient was discharged home after 48 hours.
Discussion: TTSS system can be used for closure of large full-thickness perforations, often needing multiple systems for complete defect closure.
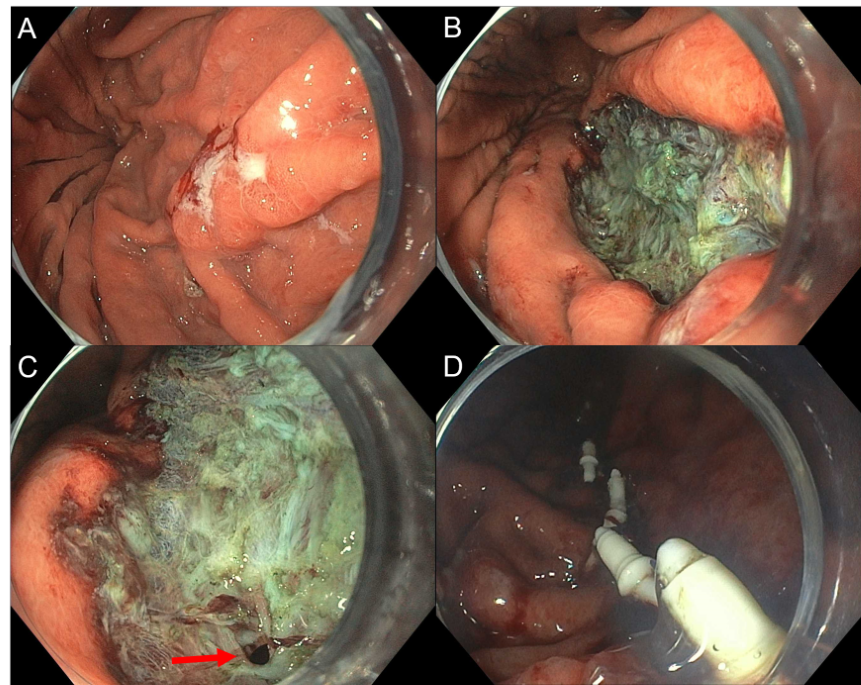
Figure: Figure 1. Gastric mass (A) and subsequent resection bed (B) following endoscopic submucosal dissection which demonstrated a full-thickness perforation (C, red arrow) successfully closed using a through-the-scope suturing device (D).
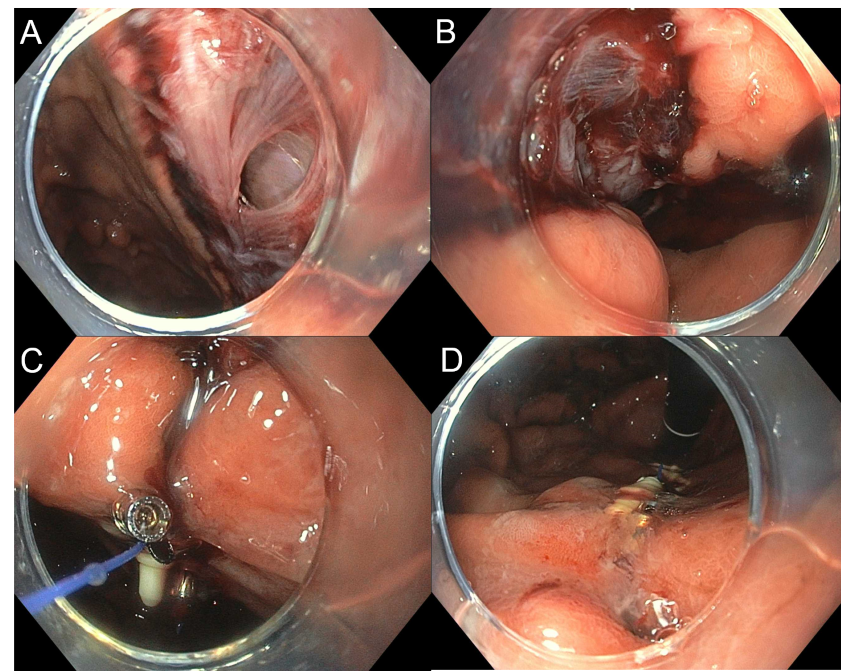
Figure: Figure 2. Full-thickness gastric perforation (A, B) successfully closed using a through-the-scope suturing device (C,D).
Disclosures:
Fernanda Pessorrusso indicated no relevant financial relationships.
Paul Menard-Katcher indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Thomas Enke indicated no relevant financial relationships.
Fernanda Pessorrusso, MD, PhD1, Paul Menard-Katcher, Md2, Mohammad Bilal, MD, FACG3, Thomas Enke, MD4. P6408 - Through-the-Scope Suturing for Full-Thickness Perforation Closure - A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Colorado Anschutz Medical Campus, Erie, CO; 2University of Colorado Anschutz Medical Campus, Aurora, CO; 3University of Colorado Anschutz Medical Campus, Denver, CO; 4University of Colorado, Aurora, CO
Introduction: Gastrointestinal perforation after endoscopic procedures is a serious adverse event that can be managed endoscopically using through-the-scope (TTS) clips, over-the-scope clips and over-the-scope suturing. The use of TTS suturing with the helix tack system, allows for immediate defect closure without the need to withdraw and reload the endoscope, however, its use has primarily been described for mucosal closure post endoscopic resection. We describe two cases of full-thickness perforation that were successfully managed with TTS suturing (TTSS) device.
Case Description/
Methods: Case 1:
A 78 year old male with Lynch syndrome and prior small bowel adenocarcinoma was recently diagnosed with gastric adenocarcinoma. Staging endoscopic ultrasound (EUS) was performed and a 4 cm lesion was seen at the incisura and EUS was unable to differentiate between T1 versus T2 disease. After multidisciplinary discussion, patient was deemed a non-surgical candidate and referred for endoscopic submucosal dissection (ESD). ESD was performed and intense submucosal fibrosis raised concerns for muscular invasion. Endoscopic intra-muscular dissection was performed. Post-resection, a 1 cm area of full-thickness perforation was noted within a 5 cm resection bed. Attempts to close it with endoclips failed. A TTSS system was used and total of 5 systems were used (each set of tacks applied in Z configuration) for closure of the complete defect (Figure 1). No leak was seen on post-procedure upper gastrointestinal (UGI) series. Patient was discharged home after observation.
Case 2: An 84 year old woman with history of esophageal squamous cell carcinoma treated withchemoradiation complicated by an esophageal stricture refractory to endoscopic dilations underwent placement of a fully covered esophageal stent. Five days after the stent placement, the patient experienced chest pain and intolerance to oral intake. Upper endoscopy was performed for evaluation. Upon stent removal, a large full-thickness perforation was discovered in the gastric cardia measuring 5 cm in length. The defect was closed using a TTSS system utilizing a total of 5 systems (each set of tacks applied in Z configuration) (Figure 2). Follow-up UGI series showed no residual leak. Patient was discharged home after 48 hours.
Discussion: TTSS system can be used for closure of large full-thickness perforations, often needing multiple systems for complete defect closure.
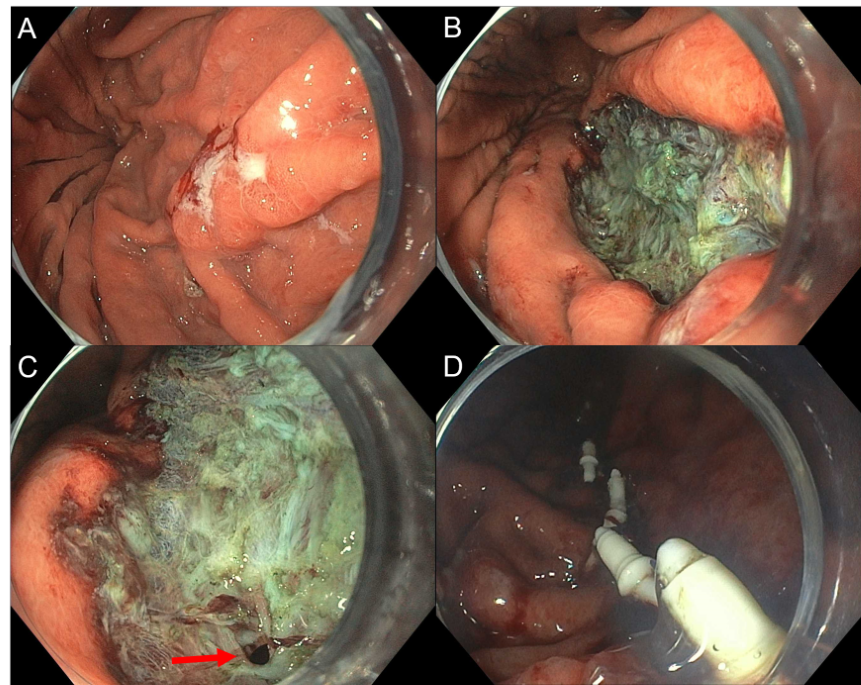
Figure: Figure 1. Gastric mass (A) and subsequent resection bed (B) following endoscopic submucosal dissection which demonstrated a full-thickness perforation (C, red arrow) successfully closed using a through-the-scope suturing device (D).
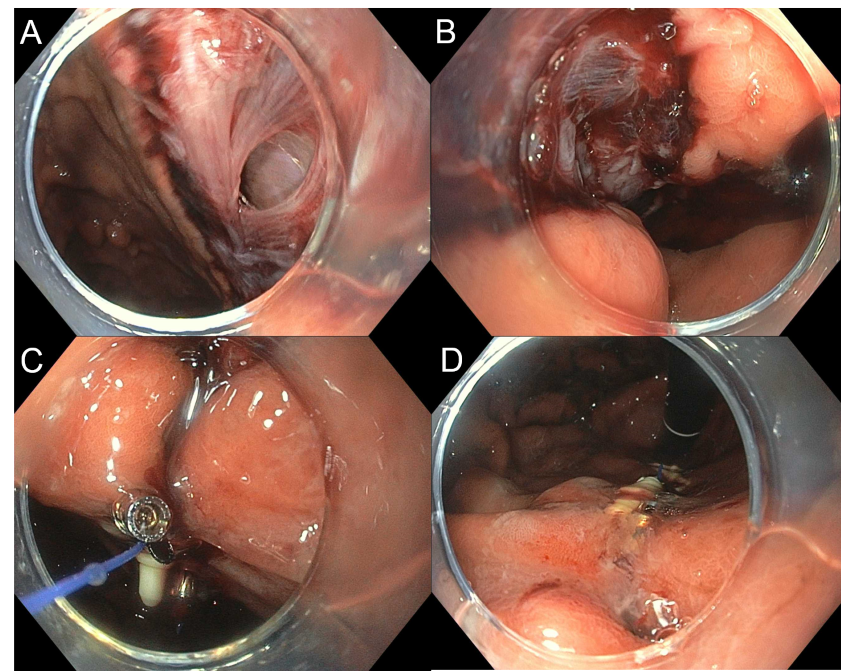
Figure: Figure 2. Full-thickness gastric perforation (A, B) successfully closed using a through-the-scope suturing device (C,D).
Disclosures:
Fernanda Pessorrusso indicated no relevant financial relationships.
Paul Menard-Katcher indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Thomas Enke indicated no relevant financial relationships.
Fernanda Pessorrusso, MD, PhD1, Paul Menard-Katcher, Md2, Mohammad Bilal, MD, FACG3, Thomas Enke, MD4. P6408 - Through-the-Scope Suturing for Full-Thickness Perforation Closure - A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
